A Simple Technique for Treatment of Post Traumatic Sialocele of Parotid Gland
Sialocele refers to extra parotid collection of saliva in peri-parotid soft tissue secondary to injury to glandular parenchyma or parotid duct. Sialocele is seen more commonly after parotidectomy and penetrating injury to face. Sialocele secondary to blunt injury to face is quite a rare phenomenon. Clinically it presents as a soft, cystic swelling in cheek region. Imaging with MRI and MR sialography is usually diagnostic, in which sialocele appears as hyper intense lesion on T2 images. Status of duct, level of ductal injury or stenosis can be easily identified with MRI sialography. Various treatment options are available for the management of sialocele. It includes conservative approaches like repeated aspiration with pressure bandage, anti-sialogogues, intra-lesional Botulinum toxin injection etc. Available surgical options include tympanic neurectomy, ductal repair via open approach or sialendoscopic assisted repair. Intra oral drainage of sialocele along with stenting of diseased duct is done when there is ductal injury in distal part near parotid orifice. Sialendoscopy during stenting helps in localization of level of lesion and guides stent placement. Various materials have been used as stent and it includes infant feeding tube, epidural catheter, cuff balloon of endotracheal tube etc. In addition ureteric stent (DJ stent) can also be used as a stent and it addresses the issue of stent dislodgement during post-operative period. Here we present a case of post traumatic sialocele of parotid duct treated successfully by intra oral drainage and stenting using DJ stent under sialendoscopic guidance in our institute.
Keywords: Sialocele; Sialendoscopy; DJ stenting
Sialocele refers to extra parotid collection of salivary secretions in peri-parotid soft tissue space. Sialocele is seen more commonly after superficial parotidectomy or penetrating injury to face. However incidence of post traumatic sialocele after blunt injury to face is very rare and it is sparsely reported in literature [1]. Most common clinical presentation is presence of soft, cystic swelling in the region of cheek, which recurs even after repeated aspirations. Traditionally USG and CT scan of face with digital sialograhy were used in evaluation such parotid area lesions. Imaging usually reveals fluid filled cystic swelling in relation to parotid duct. To assess the status of duct, traditionally digital sialography was done after injecting dye into the duct via parotid orifice. Currently MR sialography is replacing digital sialography as it is non-invasive, it precisely localizes the site of ductal injury, provides status of proximal duct upto second order branches [2,3]. Available treatment options for sialocele include repeated aspiration with pressure bandage, tympanic neurectomy, botox injection over parotid gland and anti-sialogogues [4]. Most of these options are used for treatment of sialocele that develops over parotid gland. When sialocele occurs along the course of parotid duct, it is usually due to ductal injury. Most commonly due to laceration injury to face [5] or as a complication of surgical procedures like maxillo facial fracture repair [1], rhytidectomy procedure etc. In such cases, treatment involves surgical repair of ductal injury after localising the site of involvement. Also therapeutic challenges happen when there is diagnostic delay or delay in initiation of treatment, failure of response to treatment, secondary infection or fistula formation. When addressing ductal injury, stenting of duct is essential to prevent restenosis. Ductal dilatation and stenting can be done either intra-orally or via open approach depending upon site of involvement. Sialendoscope when available can be used to localize the site of leak, placement of stent, to confirm ductal patency after repair of ductal injury [6]. Here we present a case of post traumatic sialocele, secondary to blunt injury over face treated in a novel way using salivary endoscopy at our tertiary care institution.
50 year old gentleman presented with symptoms of swelling on left side of cheek for 2 weeks duration. On eliciting history, it was noted that patient developed this swelling soon after a road traffic accident, when he sustained blunt injury over his face. He was initially evaluated in nearby hospital and referred to us for further management. At presentation, patient had soft, cystic swelling in left side of cheek and it was non-tender, non-compressible and it showed brilliant Trans illumination. Aspiration of swelling revealed clear fluid which upon biochemical analysis revealed presence of salivary amylase. Intra-orally there was scarring over parotid orifice area and parotid duct orifice could not be visualized. A clinical diagnosis of parotid sialocele was made and MRI of parotid region and MR sialogram was done which confirmed the presence of sialocele with evidence of terminal duct injury (Figure 1). Parotid gland and proximal portion of duct appeared normal.
Patient was taken up for recanalization and stenting of terminal portion of parotid duct. Intra orally parotid duct orifice was identified after probing with lacrimal probe. Ductal dilatation was done with lacrimal probe till size 6 (Figure 2). Endoscopic visualisation of sialocele cavity was done with ureteric endoscope of size 1.2 mm. Level of ductal laceration was found to be near the parotid orifice and scope could not be passed easily into the proximal portion of duct. Ureteric stent (DJ stent) of size 1mm was kept as stent (Figure 3). Outer end of stent was fixed to buccal mucosa. Free flow of saliva was noted in post-operative period. Pressure bandage was applied externally in cheek over area of sialocele. Stent was removed after 4 weeks period. After stent removal, ductal orifice was found to be patent and there was clear flow of saliva through the orifice.
Sialocele is one of the common complications of superficial parotidectomy. It happens when the secretions from deep lobe of parotid gland accumulates in subcutaneous region. Traditionally such sialocele is treated by repeated aspiration and local compression bandage to prevent fluid re-accumulation [1]. Sialocele secondary to blunt injury to face is relatively less common and only less than 10 cases have been reported so far [1]. Common site of duct injury in blunt trauma is terminal portion of parotid duct where it bends over anterior margin of masseter muscle to pierce buccal pad of fat and opens into buccal mucosa [1,7]. At this region, duct is relatively freely mobile within buccal fat pad; fat pad acts as shock absorber. When there is frictional injury, it causes ductal shearing injury resulting in terminal ductal injury, sialocele formation and stenosis of distal portion of duct.
Initially repeated aspiration was attempted in outside hospital along with oral anti-sialogogue (glycopyrollate), but it failed. Other available treatment options include tympanic neurectomy and localised Botox injection [8]. In tympanic neurectomy, the secreto-motor fibres to the parotid gland that originates from tympanic plexus over promontory of middle ear is cut via trans canal approach [9,10]. Many times it is difficult to identify the nerve and the success rate depends on surgeon expertise. Alternatively botulinum toxin can be injected locally over the gland; it inhibits release of acetyl choline and thereby inhibits the secretory action of gland [11]. Both these procedures inhibit glandular secretion and may cause atrophy of gland in long term. In our patient parotid gland and proximal duct was intact, so we didn’t attempt these procedures.
In post traumatic cases, there is ductal tear/laceration leading to salivary extravasation and stenosis of distal duct. In such cases correction of sialocele involves repair of ductal tear and stenting of stenosed segment. Ductal reconstruction via open approach is met with high rate of complications like formation of cutaneous fistula, injury to terminal branches of facial nerve and restenosis. Hence open approach was not planned in our patient and he was taken up for ductal recanalization and stenting via intra oral approach [10]. Also in our patient the stenosis was confined to terminal potion of duct and it is best managed by intra oral drainage and stenting [12].
Intra oral canalisation could be done easily with lacrimal probe. Serial dilatation was done with lacrimal probe till size 6. Sialendoscopy was done with ureteric endoscope (size 1.2 mm), which showed sialocele cavity. Sialendoscopy has been used extensively in management of sialolithiasis. Nevertheless it is also useful in localizing site of ductal injury, check for ductal patency and assist in stent placement [6,13]. In institutions where sialendoscope is not available, one can consider using ureteric endoscope for visualization of salivary duct system as it is relatively easily available. Once ductal canalisation was done there was free flow of saliva and sialocele subsided completely.
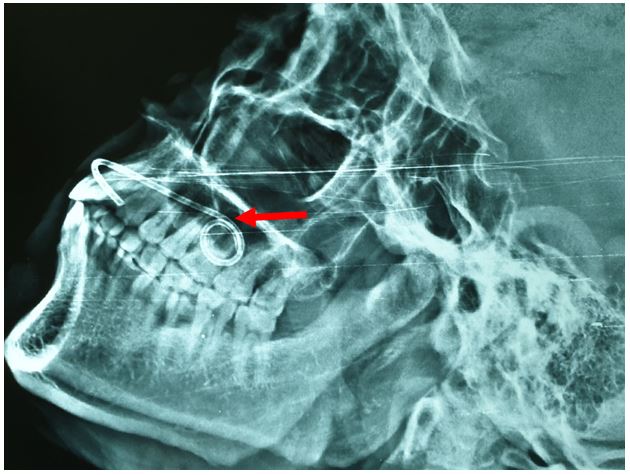
Stenting of the duct must be done to prevent restenosis. Various materials like infant feeding tube, epidural catheter [14], outer balloon of endotracheal tube [15] was considered for stenting. Fixing the stent in place was a challenge; poor fixation might lead to dislodgement of stent. To address this issue we used ureteric stent -DJ stent (double J stent).This stent has j shaped curled end at both endings [16]. The curled end can be straightened during insertion, once in place it curls up again. After insertion the curled up portion was inside sialocele cavity and another end was sutured to buccal mucosa. Post operatively check x-ray was done which revealed curled up portion within sialocele cavity ( Figure 4). Stent was kept for 4 weeks. Patient did not develop any recurrence of sialocele or restenosis ( Figure 5).
Post traumatic sialocele secondary to ductal injury is relatively less common especially after blunt injury to face. MR sialography shows better visualization of duct, sialocele cavity and glandular parenchyma. Stenosis confined to terminal portion of duct is best managed by intra oral ductal canalization, stenting and pressure bandage.