Actinomycotic Osteomyelitis of the Jaw in a Child
We report the case of a healthy child with a mandibular swelling at a site of former dental care. No other risk factors associated with jaw osteomyelitis were noted. Laboratory workup and physical examination were suggestive of a tooth abscess that was subsequently drained and cultured, thus revealing a growth of Actinomyces odontolyticus. The patient was then treated with oral amoxicilline-clavulanate for twelve days, but recurrence occurred. CT-scan and MRI were performed and confirmed the diagnosis of recurrent mandibular osteomyelitis. Treatment with intravenous meropenem and amoxicilline-clavulanate at a higher dosage was then administered for a month with complete resolution of the infection. This case suggests that a short-course treatment with intravenous antibiotic therapy, eventually followed by oral therapy, can successfully treat actinomycotic osteomyelitis.
Keywords: Actinomyces odontolyticus; Jaw; Pediatric; Osteomyelitis
Pediatric osteomyelitis has an incidence of 13 every 1, 00,000 children per year in developed countries, but occurs with a higher rate in children <3 years of age [1]. The most commonly affected sites are notably the lower extremities (femur and tibia) [2]. Mandibular osteomyelitis is reported in <1% of pediatric cases [2]. Osteomyelitis can be diagnosed by means of advanced imaging and histopatology of the infected focus. Plain radiographs have low sensitivity and specificity for detecting acute osteomyelitis [3], whereas magnetic resonance imaging has the highest sensitivity and allows to exclude osteomyelitis as a diagnosis whenever negative [4]. Despite its poorer soft tissue resolution, CT-scan offers an in-depth study of the bone component as well and is often performed before MRI, being less time-consuming. Nuclear medicine studies have very high sensitivity, but may be positive in the presence of other conditions, such as traumatic or surgical injury as well as malignancy [5]. The use of bone scintigraphy should be considered in the differential diagnosis with multifocal chronic inflammatory bone disease (CRMO). In fact, up to 10% of pediatric patients with CRMO have a mandibular involvement [6]. Recently, ultrasound imaging has also been proposed as a non-invasive and inexpensive technique in emergency departments [7]. Osteomyelitis due to Actinomyces is a rare condition, although its incidence seems higher in patients with osteopetrosis [8], bisphosphonate use [9, 10] and a compromised immune system [11]. Jaw osteomyelitis caused by Actinomyces species represents a rare clinical condition. Actinomyocosis is a chronic granulomatous disease that most commonly manifests as a cervico-facial, thoracic, abdominal, and pelvic or central nervous system disease. Among Actinomyces species, Actinomyces israelii and Actinomyces gerencseriae are the most frequently reported than Actinomyces naeslundii, Actinomyces meyeri, Actinomyces viscosus, Actinomyces odontolyticus and Actinomyces georgiae [12]. Even though the pathogenesis of Actinomyces in dental caries is not yet well known, the germ has proven to have a role in root caries [13]. In this context, the most frequent species are Actinomyces israelii and Actinomyces gerencseriae [14]. More specifically, Actinomyces gerencseriae is the causative agent of dental plaque in children suffering from severe early childhood caries, a chronic disease causing extensive destruction of primary dentition [14]. Actinomyces israelii and gerencseriae, are the main causative organisms of root caries among elderly subjects with exposed root surfaces (usually due to treated or untreated advanced periodontitis). Actinomyces naeslundii, odontolyticus and georgiae have also been isolated [12,13]. In this case we report an immunocompetent and healthy child that experienced an Actinomyces odontolyticus (AO) acute infection of the jaw and was successfully treated with antibiotic therapy.
We describe a 10-year-old caucasian immunocompetent child admitted to the surgery department of our institution. He complained of a painful swelling of the left mandible that had appeared 20 days before. Physical examination of the swelling revealed an ill-defined 4 cm wide mass, located at the angle of the left mandible, covered by normally looking skin. On palpation the lump had elastic hard consistency with a softer and tender central area, firmly adherent to the underlying bone. Oral inspection revealed a dental filling of the lower left first molar (3.6) communicating with the pulp, surrounded by inflamed gums. Medical history was notable for former dental care of the given molar (3.6). No fever was reported. The patient lacked a history of trauma and/or chronic periodontal infections. Laboratory workup showed an increase of white blood cells, notably neutrophils (WBC 17.000/mm3, neutrophils 75%). C reactive protein and erythrocyte sedimentation rate were not elevated. Mandibular X-ray showed no structural alterations of the bone. As physical examination was suggestive of a tooth abscess with overlying cellulitis, the patient underwent dental surgery with opening of the pulp chamber and drainage of the abscess. Culture examination of the purulent material revealed a growth of Actinomyces odontolyticus, whose testing proved sensitivity to most antibiotics, except metronidazole. The patient was then orally treated with amoxicillin/clavulanate 875+125 mg (60 mg/kg/day) for twelve days and betamethasone (0.5mg/kg/day) as anti-inflammatory agent for seven days. On the fifth day of hospitalization, the tooth 3.6 was extracted and the deep alveolar cavity was exposed. The culture of the swab from the cavity showed persistence of the AO infection. Given the negativity of laboratory indexes and the clinical stability of the patient, he was discharged on the sixth day of hospitalization without being seen by an infectious diseases specialist and he was prescribed oral antibiotic therapy for 5 days.
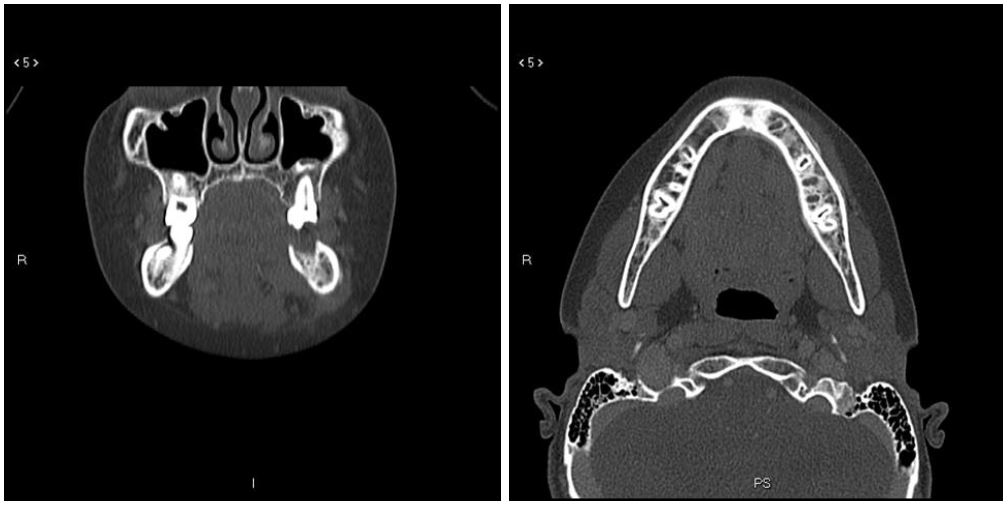
The patient was readmitted to our hospital on the 17th day after discharge for recurrence of the mandibular swelling, which showed to be increased in size and tenderness. The swelling appeared to be solid and adherent to the underlying layers, in the absence of other clinical findings. A facial CT-scan was performed and showed a lytic lesion of the left mandible along with scars from the dental extraction (Figure 1A). Other findings were a slight regional dishomogeneity with thickening of the spongiosa and a consensual fine irregularity of the cortical bone, which was unevenly thinned, especially on the lingual side (Figure 1B). The overall examination was compatible with the diagnosis of mandibular osteomyelitis. Laboratory testing proved negative.
Immunological workup was also carried out, but it did not show evidence of impairment of the immune system. According to sensibility tests performed on the culture, the patient was prescribed intravenous therapy with meropenem (90 mg/kg/day) and amoxicillin/clavulanate 875+125 mg (100 mg/kg/day) for 28 days. No side effects were reported.
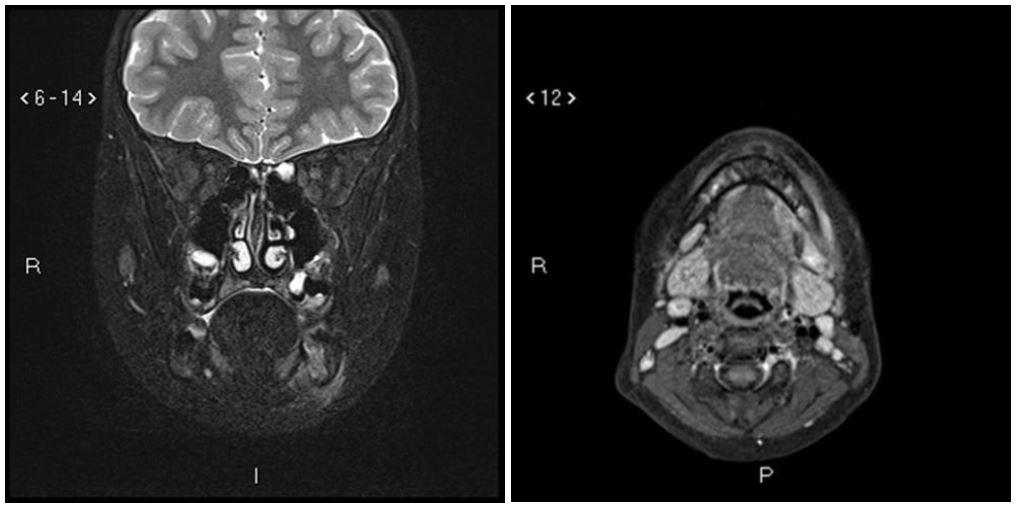
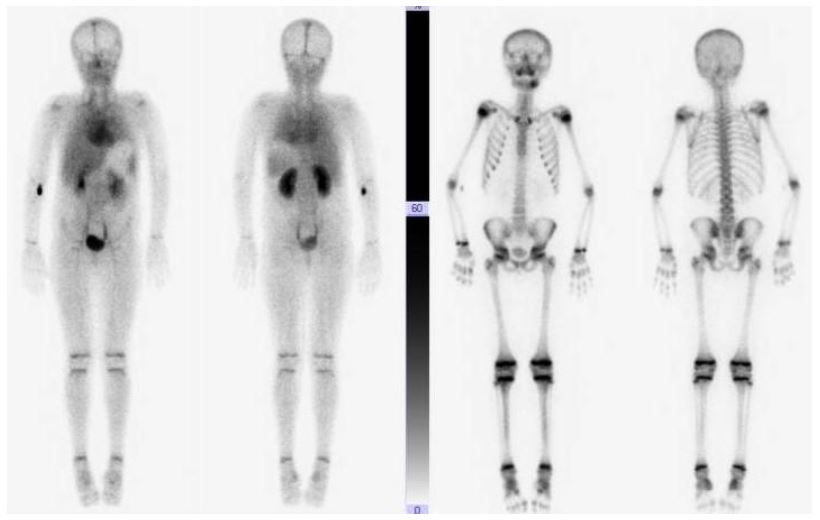
In order to exclude secondary bone localizations, the patient underwent a total body bone scintigraphy and MRI with gadolinium. Both exams confirmed a local mandibular osteomyelitis (Figure 2 and 3). The patient’s clinical course was good, with slow but progressive clinical improvement, which comprised reduction of the swelling and disappearance of pain. After a month of hospitalization, he was discharged with oral amoxicillin at 70 mg/kg/day for five weeks. During follow-up, two MRI exams were performed at the 3rd and 10th month after discharge, both of which confirmed a gradual improvement with disappearance of bone lesion signs. At the 18th month of follow-up, the patient did not present any sign or symptom of recurrence.
Actinomycosis is a rare chronic granulomatous disease caused by a group of anaerobic Gram-positive bacterium. There is little data in the literature on the prevalence of the various species of Actinomyces and even less in pediatric osteomyelitis. The main causes of actinomycotic osteomyelitis are trauma, periodontal infections, non-viable teeth and extraction sites. Actinomycosis may either be a rapidly progressive acute infection or a slowly spreading chronic lesion [15]. In addition, actinomycotic osteomyelitis often causes disease recurrence due to an incomplete response to antimicrobial agents [16]. Diagnosis of actinomycosis is obtained with isolation of the germ from culture examination of the material drawn from the infection site. However, less than 50% of the specimens are positive for Actinomyces. If no improvement is achieved after empirical therapy, a presumptive diagnosis can be made by demonstrating typical bacterial colonies in biopsy material [15]. In our case, a biopsy was not performed since the first diagnosis was that of a common tooth abscess with overlying cellulitis. Thus, neither surgical debridement nor histopatology of the bony fragments was performed.
No randomized controlled trials have evaluated antibiotic regimens for actinomycotic osteomyelitis and there is no consensus on the type and duration of treatment. Cervicofacial actinomycosis is a well-known condition in the general population, but data on such infection in children is lacking. In adults, treatment is usually based on the germ antibiotic sensitivity. Penicillins and quinolones, which cannot be used on children, are usually preferred [16,17]. The treatment of choice is oral amoxicillin, as most isolates are susceptible to beta-lactams. Adjunction of metronidazole or a beta-lactamase inhibitor may help when a polymicrobial etiology is suspected [18]. Given the low penetration of beta-lactams in bone, authors recommend a prolonged high-dose therapy in severe or chronic cases [15,19]. Several observations have reported satisfactory cure rates with 4- to 6-week antimicrobial therapy [20,21]. especially when an optimal surgical curettage and a satisfactory response to treatment is observed. In our case, intravenous therapy with meropenem and amoxicillin/clavulanate for 28 days was required, as the patient presented an acute lesion that did not respond to oral therapy with amoxicillin/clavulanate alone. After discharge, a 5 weeks oral therapy with amoxicillin was added, leading to clinical symptoms resolution and no recurrence in the following 18 months follow-up.
Guidelines on therapy of actinomycotic osteomyelitis are currently unavailable. A review of the literature proves that some cases require surgery and debridement while others may just respond to medical therapy alone [22]. This case shows how a short course of intravenous antibiotics led to a rapid eradication of actinomycotic jaw osteomyelitis in a child. Our experience suggests that pediatric mandibular osteomyelitis caused by Actinomyces species can be treated with a shorter Course of intravenous therapy than the standard 6-12 months treatment in adults [23]. Nonetheless, we believe that this assumption should be confirmed by further targeted studies in a pediatric population.