Autologous Bone Marrow Therapy to Operative Site Following Modified Radical Mastectomy to Prevent Flap Complications
Breast cancer is the second leading cause of cancer-related deaths, second to lung cancer, with approximately 40,000 deaths caused by breast cancer annually. Breast cancer is also a global health problem, with more than one million cases of breast cancer diagnosed worldwide each year [1]. Though breast-conserving surgery is more and more welcomed among female patients, modified radical mastectomy (MRM) still plays an important role in the operation for breast cancer. Postoperative complications such as wound pain, hematoma, marginal necrosis, flap necrosis, seroma, wound infection, shoulder stiffness and prolonged drainage led to a delay of adjuvant therapy after the operation [2]. In our study we have tried the autologous bone marrow therapy to operative site to prevent such complications. Two groups of patients were selected randomly containing 20 patients in each group. The patients under control group were treated by modified radical mastectomy alone whereas the patents under study group were treated by modified radical mastectomy followed by autologous bone marrow therapy to operative site. The patients were followed postoperatively and parameters like post-operative pain, seroma collection, marginal necrosis, flap necrosis, wound infection, hypertrophic scar or keloid, local recurrence of tumour was observed in both the groups of patients. After our study we found that Post operatively the patients in study group experienced less pain as compared to control group. Out of 20 patients in control group marginal necrosis was observed in 4 (20%) patients whereas in study group it was seen in 2 (10%) patients (p value = 0.4459). Flap necrosis was seen in 2 (10%) patients in control group whereas no such complication was observed in study group (p value = 0.1670). In control group 9 (45%) patients were observed to have seroma collection after removal of drain which required aspiration but in study group none of the patient had seroma collection after removal of drain (p value = 0.0058). In control group shoulder stiffness was observed in 8 patients (40%) whereas in in study group it was observed in 2 (10%) patients (p value = 0.0873). local recurrence of tumour and hypertrophic scar was only seen in 1 patient respectively in control group. No local recurrence of tumour, hypertrophic scar, keloid was seen in study group.
Keywords: Autologous Bone Marrow Therapy; Modified Radical Mastectomy; Carcinoma Breast
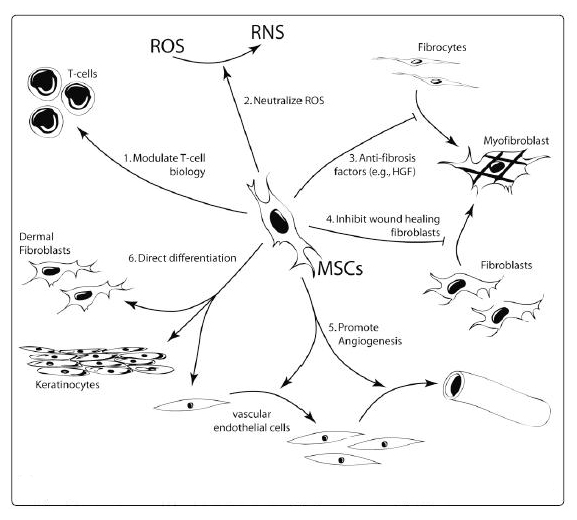
List of Abbreviations: HGF: Hepatic Growth Factor; MSC: Mesenchymal Stem Cell; RNS: Reactive Nitrogen Speces; ROS: Reactive Oxygen Species; LEC: Lymphatic Endothelial Cell; HRT: Hormone Replacement Therapy
The overall incidence of breast cancer was increasing until approximately 1999 because of increases in the average life span, lifestyle changes that increase the risk for breast cancer and improved survival rates for other diseases. Breast cancer incidence decreased from 1999 to 2006 by approximately 2% per year. This decrease was attributed to a reduction in the use of HRT after the initial results of the Women’s health Initiative were published but may also be the result of a reduction in use of screening mammography. During the year 2006 to 2010, the breast cancer incidence rates were stable [1]. But in our country where early diagnosis of breast cancer is not possible due to illiteracy, ignorance and social stigma many patients go into locally advanced stage or metastatic stage. Thus majority of them require modified radical mastectomy rather than breast conservative surgery. But after modified radical mastectomy they suffer from the common immediate complications like wound pain, marginal necrosis, flap necrosis, seroma, wound infection, lymphoedema, stiff shoulder and also from delayed complications like hypertrophic scar, keloid and local recurrence of tumour [2-4]. Due to these complications the duration of stay in surgery ward increases and the adjuvant therapy for such patients also gets delayed. Many studies have been done all over the world to prevent these complications like the use of herbal medicines by the Chinese, delaying post-operative physiotherapy [5-10]. For a week, use of harmonic scalpel instead of electrocautery [6,11], use of negative suction drain and compressive dressings[11,12] etc. None of the methods alone is sufficient to prevent such problems thus a combined approach is used. Autologous bone marrow therapy is a new concept which is based on the facts that bone marrow contains mesenchymal stem cells which stimulates the local stem cells, fibroblast and macrophages for their enhanced activity. They also liberate cytokines and growth factors which helps in rapid wound healing and preventing early flap complications like wound pain, flap and marginal necrosis and seroma formation.
In this prospective study from November 2013 to November 2016 we have done a prospective analysis in the study on the effect of autologous bone marrow therapy to breast bed, axillary bed and breast flaps to prevent flap complications.
“To Study The Effect of Autologous Bone Marrow Therapy to Breast Bed, Axillary Bed and Breast Flaps to Prevent Flap Complications”.
“To Study The Effect of Autologous Bone Marrow Therapy to Breast Bed, Axillary Bed and Breast Flaps Following Modified Radical Mastectomy to Prevent Hypertrophic Scar, Keloid Formation and Local Recurrance of Cancer”.
Institutional ethics committee clearance and informed consent of the patients was taken before the study. Then total fourty breast cancer patients with stage T1-3 N0-1 M0 in this study underwent modified radical mastectomy surgery at VSS Institute of Medical Sciences and Research Institute, Burla, Odisha, India in one surgical unit during the year 2013-16. Out of 40 patients, 20 patients were kept in study group and rest 20 in control group. Auchincloss type modified radical mastectomy was performed in all patients. In the study group, on operative table bone marrow was aspirated from the sternum of the patients using bone marrow aspiration needle under anaesthesia. Then the aspirate was kept aside after priming with heparin in a sterile syringe. Then skin flaps were raised as per standard procedure, mastectomy and axillary clearance and hemo stasis was obtained in all the cases. Bone marrow aspirate was infiltrated to under surfaces of breast flaps and breast bed and to axillary bed. Skin flaps were closed with a suction drain. Pressure garment and suction drains were used routinely in both study and control group. Post operatively the patients were followed and parameters like wound pain, marginal necrosis, flap necrosis, wound infection, seroma collection, shoulder joint stiffness, hypertrophic scar, keloid and local recurrences were studied (Figure 1 and 2).
Post operatively the patients in study group experienced less pain as compared to control group. Out of 20 patients in control group marginal necrosis was observed in 4(20%) patients whereas in study group it was seen in 2 (10%) patients (p value = 0.4459). Flap necrosis was seen in 2(10%) patients in control group whereas no such complication was observed in study group (p value = 0.1670). In control group 9(45%) patients were observed to have seroma collection after removal of drain which required aspiration but in study group none of the patient had seroma collection after removal of drain (p value = 0.0058). In control group shoulder stiffness was observed in 8 patients (40%) whereas in in study group it was observed in 2(10%) patients (p value = 0.0873). local recurrence of tumour and hypertrophic scar was only seen in 1 patient in control group. No local recurrence of tumour, hypertrophic scar and keloid was seen in study group [13-15] (Table 1, 2 and 3, Figure 3).
MSCs were initially isolated from bone marrow but are now shown to reside in almost every type of connective tissue [16]. MSCs are characterized as a heterogeneous population of cells that proliferate in vitro as plastic adherent cells able to develop as fibroblast colony forming-units [17]. MSCs are distinguished from hematopoietic cells by being negative for the cell surface markers CD11b, CD14, CD34, CD45 and human leukocyte antigen (HLA)-DR but expressing CD73, CD90 and CD105. Importantly, the capacity to differentiate into multiple mesenchymal lineages including bone, fat and cartilage is used as a functional criterion to define MSCs [18]. MSCs are clearly capable of responding and modulating their function when exposed to the cells and biochemical factors that are characteristic of an injury environment. Human MSCs migrate preferentially to regions of inflammation [19] and express several chemokine receptors that are necessary to coordinate their homing ability [20]. Furthermore, MSCs have demonstrated chemotaxis toward a variety of wound healing cytokines in vitro, including platelet-derived growth factor, insulin-like growth factor-1, IL-8 and TNFα [21,22]. These data suggest that bone-marrow-derived MSCS or endogenous cells resembling MSCs, such as pericytes, are likely to migrate to and participate in the response to tissue injury. During modified radical mastectomy we iatrogenically injure the lymphatic system, blood vessels and other tissues. Injury to lymphatic system causes seroma formation and lymphoedema.
Studies have shown that mesenchymal stem cells (MSCs) derived either from bone marrow or fat can express LEC markers (prox-1, VEGF-C, VEGF-A) and that stimulation of these cells in cultured media with recombinant VEGF-C, even for brief periods of time in vitro, markedly increased their ability to promote lymphangiogenesis in vivo [23, 24]. Thus adult mesenchymal stem cells may have an important role in decreasing seroma formation and also lymphoedema after modified radical mastectomy by early healing of injured lymphatic vessels. In our study we have observed less seroma collection in study group than control group and after removal of drain 9 patients out of 20 patients in control group came for seroma collection which required aspiration by needle whereas in study group none of the patient came with complaint of seroma collection after removal of drain. Our this finding supports the above literature there by suggesting the role of autologous bone marrow therapy in early healing of injured lymphatic system resulting into decreased seroma collection.
MSCs produce basic FGF and VEGF-A, which provide powerful mitogenic cues to promote proliferation, migration and differentiation of microvascular endothelial cells [25,26]. MSCs also express paracrine factors to promote vascular stability and vasoprotection [27,28], including adrenomedullin [29]. It has been hypothesized that these functions are unique to MSCs due to their possible perivascular origin, and they are able to exploit these functions to recreate their perivascular niche as theprocess of vasculature remodeling is concluded [30]. Enhancement of vascular formation by bone-marrow derived MSCs has been demonstrated in vitro [31] and to facilitate the development of long-lasting functional vasculature as perivascular progenitor cells [32]. Thus autologous bone marrow therapy may facilitate neovascularisation and thereby prevent marginal necrosis and flap necrosis. Though proper surgical technique like tension free suturing, not too thin flap, less thermal injury by electro cautery have an important role in preventing marginal necrosis and flap necrosis but despite the use of all these techniques marginal necrosis and flap necrosis are very frequent in patients after modified radical mastectomy.. In our study we have seen marginal necrosis in 4 out of 20 patients in control group and 2 out of 20 patients in study group and flap necrosis in 2 out of 20 patients in control group and none of the patients in study group. Though such finding is not statistically significant still relatively we have seen less marginal necrosis and no flap necrosis in study group as compared to control group. Regarding postoperative pain , patients experienced very less pain as compared to control group may be due to the anti- inflammatory activites of mesenchymal stem cells. MSCs have anti-inflammatory effects because they inhibit dendritic cell [DC] maturation and B and T cell proliferation and differentiation, that they attenuate natural killer [NK] cell killing, and that they also support suppressive T regulatory cells [Tregs][33-35]. MSCs also decrease the amount of IL-10 and TNF-α secreted by DC cells, and increase the amount of the anti-inflammatory IL-4 produced by T cells [33-35]. MSCs provide significant benefit during dermal wound healing, as they can,
1) Accelerate the rate of wound closure and re-epithelialization,
2) Improve the quality and strength of the regenerated tissue,
3) Recover wound healing pathologies that might otherwise result in a chronic, non-healing wound, and
4) Minimize the visual appearance of scar tissue.
In adult cutaneous wound healing, inflammatory cells are recruited to the wound and produce proinflammatory mediators such as monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein-1 beta (MIP-1β), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6). These mediators can not only induce additional inflammation but also contribute to excess extracellular matrix (ECM) deposition and fibrosis. Moreover, the inflammatory cells can produce growth factors such as transforming growth factor-beta 1 (TGF-β1) and platelet-derived growth factor, which stimulate fibroblast proliferation, myofibroblast differentiation, and excess ECM deposition, leading to scar formation. We have not seen any local recurrence and it need to be studied more to prove the anti-tumour effects of mesenchymal stem cells (Figure 4). This study is purely clinical and we have only seen the effects of autologous bone marrow therapy and the rationale behind them are still being studied at molecular level. At present our sample size is small and we will continue our research in more number of patients in future.
To minimize the skin flap complications after modified radical mastectomy for breast cancer, lesser use of cautery and infiltration of autologous bone marrow, routine use of suction drains and application of pressure garments may be recommended.