Basal Cell Adenoma of the Parotid Gland: Case Report
Objective: Basal cell adenomas are rare form of monomorfic adenomas of the parotid gland. This rare form of the tumors are mostly seen on suprafacial part of the parotid gland. Basal cell adenomas are well demarcated and asymptomatic tumors that can be treated by surgical removal.
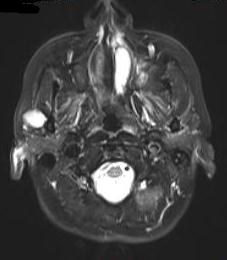
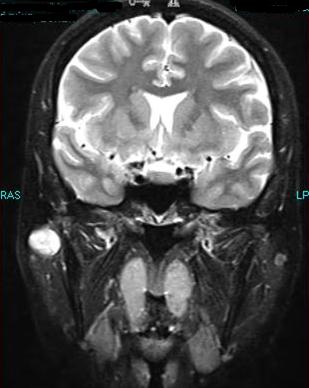
Case repor: 48 years old female referred to our clinic with complaint of right sided asymptomatic preauricular swelling over 8 months. On the magnetic resonance examination on the right side of the parotid region, there was a contrast enhanced well demarcated, about 1,9x1,5 cm in size, round shaped mass lesion on T2 weighted view. Fine needle aspiration biopsy was not conclusive.
Treatment and Prognosis: We planned superfacial parotidectomy but during surgery we recognize that the tumor was located on the deep lobe of the gland so performed partial parotidectomy for diagnosis and treatment. The pathologic investigation revealed basal cell adenoma. Recurrence was not detected in the 2 year follow up.
Conclusion: Basal cell adenomas are rare form of parotid benign adenomas which can be misdiagnosed with malign tumors such as adenoid cystic carcinoma. The diagnosis with fine needle aspiration is difficult so when detected on physical examination on parotid region we should not insist on fine neddle aspiration biopsy to diagnosis.
Keywords: Basal cell adenoma; Salivary gland tumors; Deep lobe; Parotid gland
Salivary gland tumors constitute only 2% to 6, 5% of all head and neck region tumors. Because of lots of types are defined, it is hard to diagnose the tumor definitely. Basal cell adenoma (BCA) is a rare neoplasm consisting of a monomorphic population of basaloid epithelial cells and accounts for 1-3% of all salivary gland tumors [1]. Most of these tumors are located on the parotid region. Also most of the parotid benign tumors are located on the superficial lobe.
We represent basal cell adenoma of the parotid gland which was located on the deep lobe of the gland with unusual location The tumor was excised successfully without total parotidectomy.
A 48 year-old female patient was admitted to our clinic, who suffered from asymptomatic right preauricular mass lesion for about 8 months. On the physical examination there was a palpable approximately 1x1 cm in size, well demarcated, painless, mobile mass located on anterior side of the tragus. According to the magnetic resonance image (MRI) examination on the right side of the parotid region, there was a contrast enhanced well demarcated, about 1,9x1,5 cm in size, round shaped mass lesion on T2 weighted view (Figure 1a,b).
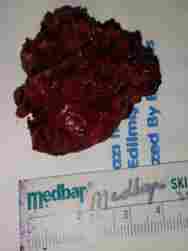
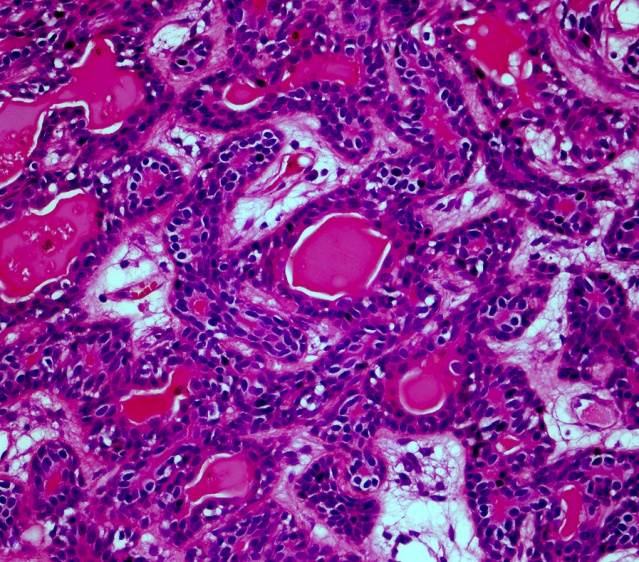
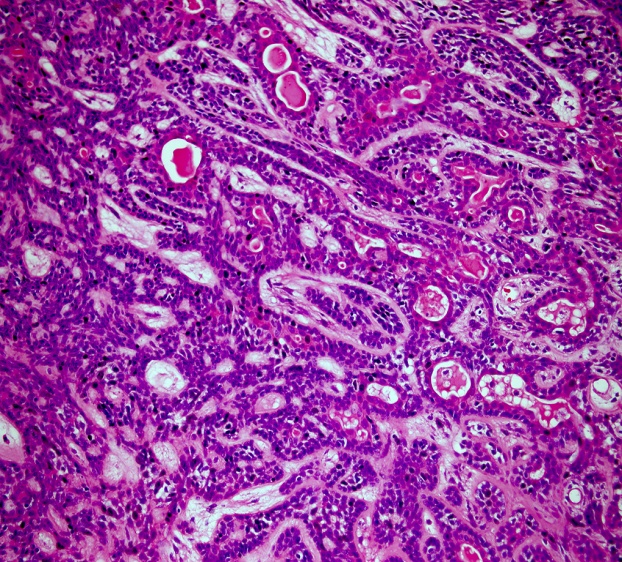
Fine needle aspiration biopsy (FNAB) revealed insufficient diagnosis. After Informed consent was obtained from patient, we considered parotidectomy. During the surgical procedure we found the facial nerve at first. Then we followed the trace of the facial nerve and detected the tumor was located on the deep lobe of the gland. We excised the lesion with intact surgical margin (Figure 2). At frozen section examination there was no invasion. Finally we surgically sutured and fixed the parotid gland. Pathologic examination define the tumor as BCA of the parotid gland (Figure 3a,b). The patient has a mild transient weakness during eye closing for one month period. Throughout the 1 year follow up, there was no complaint and recurrence detected.
Kleinsasser and Klein suggested that monomorphic adenoma differs from pleomorphic adenoma by different structures [2]. Monomorphic adenoma was classified as basaloid and non basaloid type. BCA is a subtype of monomorphic adenoma.
BCA is a rare benign form of epithelial tumor which involves monomorphous and uniform basaloid cells. BCA are commonly seen on the parotid gland but less commonly detected on minor salivary gland and upper lip [3-5]. Salivary gland tumors with basaloid aspect sited in the upper lip usually are canalicular adenoma.
The most common tumor on the parotid region is the pleomorphic adenoma which corresponds 65% of all parotid tumors. But BCA corresponds only 1-3% of all salivary gland tumors.
BCA is mostly seen on parotid region and affects mostly adults and females [6-8].
Most of the tumors are detected between 5 and 6 decades of life. BCA is clinically slow growing, asymptomatic, painless, well demarcated, freely movable masses. As in our case the lesion on the parotid region was slow growing, painless, asymptomatic, well demarcated. Also the tumor was progressively growing over the 8 months.
The pathological diagnosis can be unfavorable on FNAB examintaion. On the differential diagnosis adenoid cystic carcinoma, basal cell adenocarcinoma and pleomorphic adenoma are suspected. The exact diagnosis can be done via pathologic examination of the mass. BCA differs from adenoid cystic carcinoma and basal cell adenocarcinoma with presence of squamous differentiation and hyalinization. Also BCA has no atypia, necrosis and significant mitotic activity [9] BCA differs from pleomorphic adenomas by naked nuclei without plasmacytic shape cells [10]. Immunohistochemical exam: the contribution of the markers to the diagnosis of BCA is not clear. There are a lot of myoepithelial markers and cytokeratins that should be employed in the differential diagnosis of BCA.
In our case we can not diagnose the tumor via FNAB. The real pathology defined when the specimen was examined.
On the MRI examination, contrast enhancement can be detected. But this study does not differantiate the malignancy subtype. On the studies, solid or cystic components can be also detected [11]. In our case, we also detected the contrast enhanced well demarcated 2x2 cm in size mass lesion on the deep lobe of the parotid gland.
The treatment is surgical excision via total or superficial parotidectomy. The primary aim is to excise the tumor with its capsule. Malign transformation of the BCA is very low. Most of the parotid gland masses are located on the superficial lobe of the gland. Superficial parotidectomy can be the choice for this tumors. For rarely seen deep lobe tumors, total parotidectomy can be performed. But total parotidectomy is a high risk surgical procedure because of the alongation of the facial nerve. In our case, the lesion was located on the deep lobe of the parotid gland below the temporofacial and cervicofacial branch of the facial nerve. We performed total excision of the mass with free surgical margins. So we were kept away the morbidity of the total parotidectomy. But all the BCA patients should be called for control examinations. During 1 year follow up there was no recurence. We suppose that BCA tumors which are located deep lobe of the parotid gland, can be treated via total excision without total parotidectomy.
Basal cell adenomas are rare tumors and most of these tumors located on the parotid gland. The diagnosis on fine needle aspiration may be unsufficient and can confuse the clinician with other tumors of the parotid gland. The exact diagnoses can be achieved by investigation of the mass completely. The main treatment procedure of these tumors is parotidectomy. We emphesize this rare tumor which can be detected on the deep lobe of the parotid gland and confuse the clinician with malign parotid tumors.