Caesarean Scar Ectopic Pregnancy: A Rare Case Report with Emphasis on Imaging Findings
Caesarean scar ectopic pregnancy is often considered the rarest type of ectopic pregnancy. Failure to diagnose this condition early can lead to uterine rupture and massive hemorrhage. In this report, we present an extremely rare case of a young woman with Caesarean scar ectopic pregnancy, diagnosed early by ultrasonography and confirmed by 3.0-T magnetic resonance imaging, and to our knowledge, this case represents the earliest diagnosed patient in the literature.
Keywords: Ectopic pregnancy; Caesarian scar; Ultrasonography; MRI
Pregnancy implanted in a previous Caesarean section scar is an extremely rare form of ectopic pregnancy. It has an estimated incidence of 1: 1800–2200 pregnancies [1]. However, its incidence is increasing over the past years due to the rise in Caesarean section rates worldwide and the more widespread use of the transvaginal scan that allows earlier detection of such pregnancies [2]. This type of pregnancy is potentially life-threatening if not diagnosed and treated early. It may lead to uterine rupture, massive hemorrhage, and hypovolemic shock [3]. The diagnosis is usually made on ultrasonography and can be confirmed by magnetic resonance imaging (MRI) or during laparoscopy and/or laparotomy. Herein, we present a case of early diagnosis of ectopic pregnancy in Caesarean section scar in a multiparous woman who had come with slight vaginal bleeding.
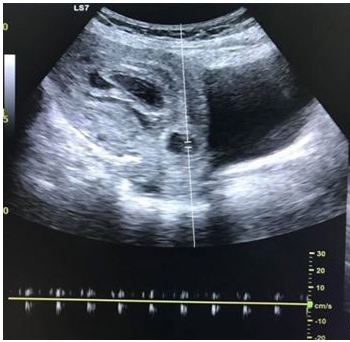
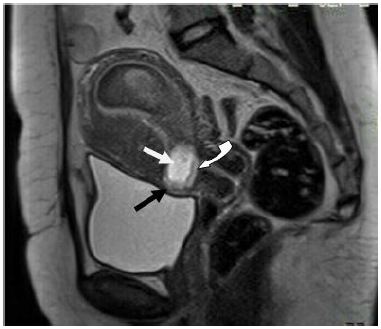
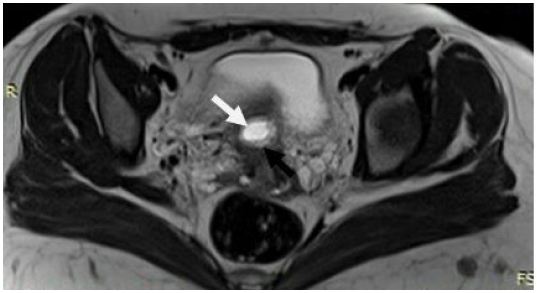
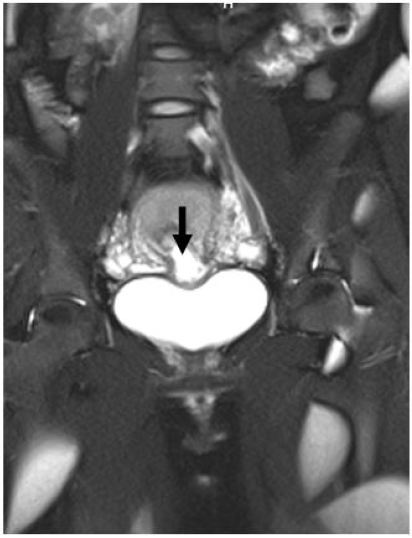
A 25-year-old woman had come to outpatient ultrasound clinic for checkup after 6 weeks of amenorrhea. She was complaining of slight active vaginal bleeding and lower abdominal pain. Her obstetrical history revealed 3 previous caesarean sections; the first one performed 5 years ago for cephalopelvic disproportion. The second one was due to placenta previa. The last one performed 1.5 years back for breech presentation. Transabdominal ultrasonography supplemented by transvaginal scan demonstrated thick fluid (blood) filled the endometrial cavity and a gestational sac of 16 mm (5 weeks + 6 days) surrounded by the decidual reaction within the anterior lower uterine wall at the location of the previous Caesarian section scar (Figure 1). The myometrium anterior to the gestational sac was thinned out. Spectral Doppler examination revealed cardiac activity within the gestational sac (Figure 2). The patient’s first set of serum beta human chorionic gonadotropin (beta- hCG) was 8470 IU/L increased to 16628 IU/L after 56 hours. MRI of the pelvis was performed in a 3.0-T MRI scanner (Siemens aera). The study confirmed a gestational sac implanted within the anterior myometrium of the lower uterine segment in the region of the scar of previous Cesarean section (Figure 3,4 and 5). The gestational sac showed a well-defined T2 hypointense fetal pole within and was surrounded by a well-appreciated decidual reaction. The myometrium anterior to the gestational sac was thinned out. Posteriorly, the gestational sac was seen extending into the endometrial cavity in the lower uterine segment. The posterior myometrium showed good wall thickness. The patient and her family were counseled about the management options and they offered the options of methotrexate therapy or diagnostic laparoscopy with the possibility of repairing the scar defect. The patient did not desire to preserve her uterus as she already had 3 living babies. She went on to have a laparotomy and hysterectomy. She tolerated the procedure well and post-procedure follow-up serial ultrasound examinations of the pelvis showed no complications.
Implantation of a pregnancy within a Caesarean section scar is considered to be the rarest form of ectopic pregnancy and a life-threatening condition. Of the many theories for explaining its occurrence, the most reasonable one seems to be that the blastocyst enters into the myometrium through a microscopic dehiscent tract. This may be created throughout a trauma of a previous Caesarean section, any other uterine surgery, or even following the manual removal of the placenta [4,3]. Another mechanism for intramural implantation is IVF and embryo transfer, even in the absence of any previous uterine surgery [5]. Two types of cesarean scar pregnancy have been reported by Vial, et al. [6]. The first type, a deep implantation in a cesarean scar defect towards the bladder and the abdominal cavity, is associated with a high risk of uterine rupture, uncontrollable bleeding, hysterectomy, and maternal morbidity; the second involves an implantation growing into the uterine cavity. The former type of cesarean scar pregnancy, with deep myometrium implantation, is more likely to cause uterine rupture even in early pregnancy. In principle, it is recommended that the pregnancy is terminated. Maymon, et al. in their study done on 8 women diagnosed with caesarean scar ectopic pregnancy believed that the prognosis for an uneventful term pregnancy is still very poor [7].
Typically, the diagnosis is made based on ultrasound evaluation of the uterus and confirmed by MRI or during laparoscopy and/or laparotomy. Sonography combined with Doppler flow imaging has been advocated as a very reliable tool for detecting these cases, without the need for a pelvic MRI for confirmation [2,7]. Described ultrasound criteria for diagnosis of Caesarian scar ectopic pregnancy include a gestational sac located in the anterior part of lower uterine segment, absence or thinning out of myometrium between the bladder wall and the gestational sac, no trophoblastic tissue visible in the uterine cavity and cervical canal, and clearly visible circular blood flow surrounding the sac [6,8].
A variety of conservative and surgical approaches have been proposed for the treatment of Caesarean scar pregnancy; however, the optimal mode of management is not established till now due to its rare occurrence. Methotrexate is the most common type of medical therapy that is suitable for use in early pregnancy and can be administered systemically and locally. It may be single- or multidose and can be combined with uterine artery embolization or curettage as an adjunct [9]. Failure of medical therapy will eventually necessitate secondary surgical intervention. Medical treatment is also unsuitable in cases of advanced gestation and uterine rupture. Surgical interventions include resection of the ectopic pregnancy or hysterectomy. Curettage was considered unsuitable as the first-line treatment option; the trophoblastic tissue was outside the uterine cavity and perforation of the implantation site may occur and result in severe peritoneal hemorrhage, which may ultimately require further surgical treatment. In the event of an emergency, laparotomy and hysterectomy may be required. However, if the diagnosis is made during early gestation in a hemodynamically stable patient, laparoscopic excision of the ectopic pregnancy is possible, with minimal morbidity and preservation of future fertility [10]. The ectopic pregnancy can thus be removed, the uterine defect repaired and the uterus conserved.
It is a recognized fact that a Caesarean section is associated with a future risk for placental pathologies (eg, placenta previa, placental abruption, and placenta acccreta) and ectopic pregnancies. However, a Caesarean scar pregnancy is considered to be even more aggressive than placenta previa or accrete because it invades the myometrium in the first trimester [11]. Patients who have undergone multiple caesarean sections appear to be at increased risk for in-scar implantation of the subsequent pregnancy because of increased scar surface area [7]. With the advent of transvaginal sonography and with the use of saline infusion, it is possible to assess post caesarean section uterine wall integrity even in the nonpregnant state [8,12]. Caesarean section scar defect is identified by the presence of fluid within the incision site or any filling defect, which is defined as a triangular anechoic structure at the presumed site of the scar [8,12].
The implantation of a pregnancy in a previous Caesarean section scar is the rarest of ectopic pregnancy locations. It may become complicated with uterine rupture and life-threatening hemorrhage. Therefore, early diagnosis using sonography combined with Doppler flow imaging is crucial, followed by confirmation of pelvic MRI if and when indicated. Although expectant management has been attempted in some cases, currently available data support termination of such a pregnancy once the correct early diagnosis is made.