Case Series of Rare Cervical Nerve Root Schwannoma
10% of schwannoma that occur in the head and neck region mostly originate from the vagus or sympathetic nervous system whereas those arising from C2 and C6 nerve root are extremely rare. Extra cranial schwannomas in the head and neck region are rare neoplasm. Diagnosis is established by imaging studies such as magnetic resonance imaging or computed tomography, while FNAC is used to rule out other condition. Histopathology gives definitive diagnosis. The accepted treatment for these tumors is surgical resection with preservation of the neural pathway. We present two rare case of right cervical nerve C6 root schwannoma of 26 years old male who presented with right lateral neck swelling with radiating pain to arm. Another case of Cervical nerve (C2-C3) root schwannoma of 50 years old male who presented with right lateral neck swellingwith pain radiating to right shoulder associated with right shoulder stiffness, Complete surgical excision was done for both patients with no postoperative neurological affection.The clinicopathological evaluation and management are described.
Keywords: Schwannomas; Neurinomas; Cervical Root Schwannoma; Surgical Treatment
Schwannomas also known as neurilemmomas or neurinomas are benign nerve sheath tumors deriving from Schwann cells that occur in the head and neck region in 25-45% of cases [1]. About 10% of schwannoma that occur in the head and neck region mostly originate from the vagus or sympathetic nervous system whereas those arising from cervical nerve root are extremely rare. Preoperative imaging studies such as magnetic resonance imaging (MRI) and computed tomography (CT) are used to distinguish its location and origin. The treatment of schwannoma is primarily surgical resection.We present a rare case of right Cervical nerve C6 root schwannoma of 26 years old male who presented with right lateral neck swelling with pain. Pain was radiating to right arm without right shoulder stiffness, swelling was removed successfully through a posterior triangle incision with no post-operative neurological symptoms. Another case of Cervical nerve (C2-C3) root schwannoma of 50 years old male who presented with right lateral neck swelling with pain radiating to right shoulder associated with right shoulder stiffness, swelling which also had intervertebral part was removed successfully through neck incision with no post-operative neurological symptoms.
A 27 year old male patient presented to our department with a right sided lateral neck slow growing swelling which was noticed 3 months back (Figure 1 and 2). There was no dysphasia, dyspnea or hoarseness of voice or pain, fever or trauma. It was a well defined swelling 3 cm × 2.5cm in the right side lower posterior triangle of the neck deep to the right sternocleidomastoid muscle. It was firm in consistency without restricted mobility in all planes and showed no signs of inflammation.Carotid pulsations were displaced anteriorly. Neurological examination revealed no local or focal neurological deficits. On flexible laryngoscopy bilateral vocal cords were mobile. Ultrasound neck revealed well defined lobulated hetrogenous echogenic lesion mass 4.9 cm × 2.5 cm × 4.7cm with internal cystic area and septation noted.
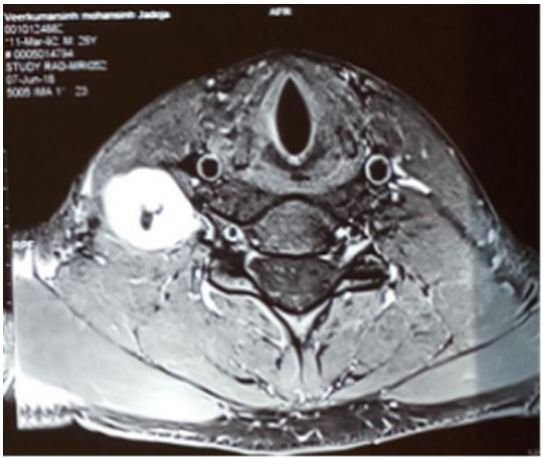
MRI cervical spine revealed well defined solitary ellipsoidal lesion in the right interscalene triangle with enhancement extending along the post ganglionic segment of the right C6 nerve root upto right C5-6 neural foramen without intradural extension represents a schwannoma arising from right C6 nerve root.
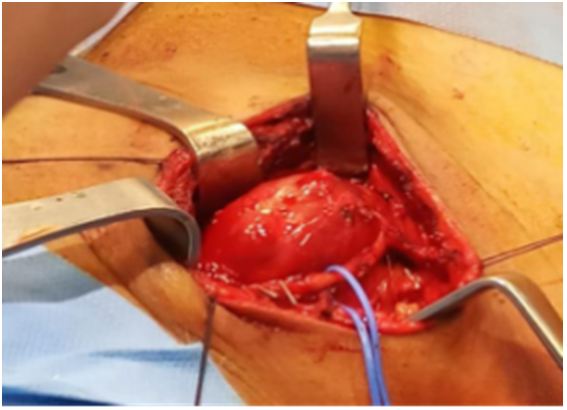
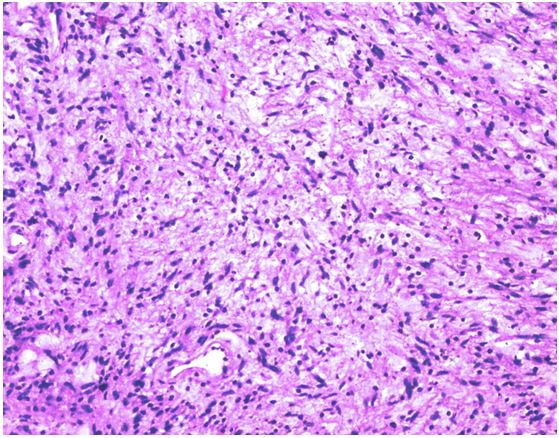
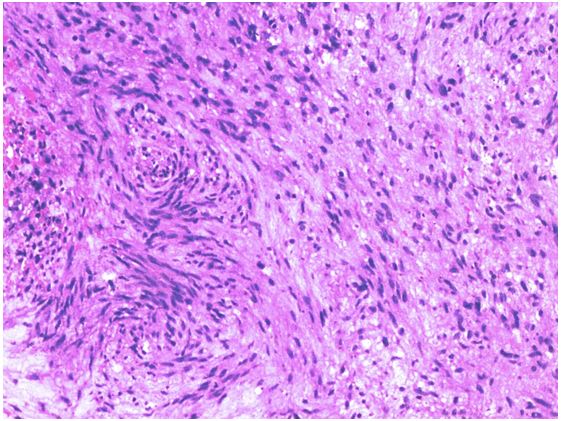
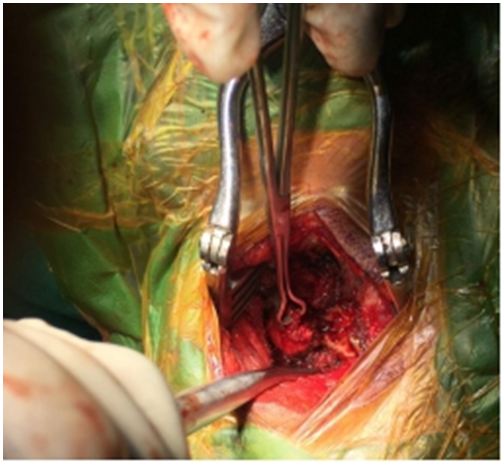
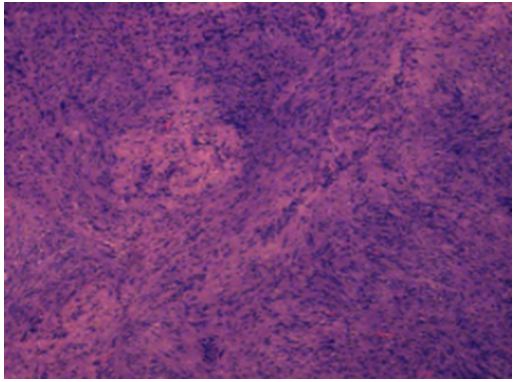
Excision of the mass was done by a neck crease incision in posterior triangle (Figure 3). Subplaplatysmal flaps raised. Sternocleidomastoid muscle dissected and retracted anteriorly. Subcutaneous tissue surrounding the tumour excised. Preserving the phrenic nerve trunk of C5 dissected, Perineurium of tumour incised and dissected then tumour separated from inferior end upwards preserving C6. Intraoperative monitoring of nerve function was not done The intracapsular resection of schwannoma was safely done. Post operatively patient was stable with no neurological deficits (Figure 4 and 5). Histopathological examination revealed a benign encapsulated neural tumour comprising of spindle shaped cells arranged in Antoni A and Antoni B pattern with verocay bodies. No evidence of any atypia or malignancy was noted.
A 50 year old male patient presented to our department with a right sided lateral neck slow growing swelling which was noticed 3 months back (Figure 6). There was no dysphasia, dyspnea or hoarseness of voice or pain, fever or trauma. It was a well defined swelling 2 cm × 2 cm in the posterior triangle of the neck deep to the right sternocleidomastoid muscle. It was firm in consistency with restricted mobility in all planes and showed no signs of inflammation. Carotid pulsations were displaced anteriorly. Neurological examination revealed no local or focal neurological deficits. On flexible laryngoscopy bilateral vocal cords were mobile. Ultrasound neck revealed mixed echogenic lesion mass 1.3 cm × 1.4 cm × 2.3 cm along the posterior-lateral aspect right sternocleidomastoid and superior aspect of neck muscle.
MRI cervical spine revealed well defined encapsulated pear shaped lesion in the right paraspinal region with its tail in the right C2-3 neural foramen with central cystic component with nodular wall showing blooming on gradient images representing neoplastic etiology of nerve sheath origin like shwannoma.
An excision of the mass was planned by a posterior neck incision (Figure 7). Tumour was approached from posterior mid line approach to cervical spine of the neck. Right C2-C3 laminotomy and facetectomy done. A globular yellowish well defined mass visualized and the capsule (intracapsular) dissected out after taking an incision over it reaching up to the root of the swelling which was seen arising from the C2-C3 inter vertebral foramen. The tumor was identified, separated and removed. Post-operatively the patient was stable with no neurological deficits (Figure 8). Histopathological examination revealed a benign encapsulated neural tumour comprising of spindle shaped cells arranged in Antoni A and Antoni B pattern with verocay bodies (Figure 9 and 10).
Schwannomas, neurilemmomas or neurinomas are benign nerve sheath tumors deriving from Schwann cells that occur in the head and neck region in 25-45% of cases [1]. About 10% of schwannoma that occur in the head and neck region generally originate from the vagus or sympathetic nervous system [2]. Rarely, they arise near the vertebral foramina presenting with intraspinal and extraspinal components [1].
Vagal schwannoma is typically characterized by dysphagia and hoarseness. Sympathetic schwannoma is characterized by Horner’s syndrome. In most cases, however, there are no symptoms, thus it is difficult to identify the neurological origin based on the physical examination [3].
As in our case 2 though tumour was arising from C2 nerve root which had intervertebral extraspinal part, the patient had no preoperative neurological deficit. Imaging diagnostic modalities like USG and MRI offer great help in identifying the tumor and its correlations with surrounding vascular structures, muscles and nerves. Previously, to prevent the recurrence of tumors, radical dissection including the neuroprogenitor cells was performed. Even in cases in which recovery was achieved following the nerve transplantation or primary anastomosis, preservation of the neurological function was not to be expected. Most of the neuroprogenitor fibers do not run through schwannoma and they pass over the tumor capsule. Most schwannomas are encapsulated. In cases where the nerve fibers surround the surface of tumors, the intracapsular enucleation can be performed while preserving the nerve fibers of C6 [1,4]. According to the study by Valentino, et al. intracapsular enucleation while preserving the nerve fibers preserved its function by more than 30% when compared to tumor resection with primary anastomsosis [5].
According to Zbären, et al. there was no significant difference in the recurrence rate between the total tumor resection including nerve fibers and the intracapsular enucleation. In cases where partial removal of the tumor was performed, however, the recurrence rate has been reported to rise [6].
According to Yamane K, et al. permanent motor deficits were the result of resecting functioning relevant nerve roots that is C5-C8 [7]. The rate of permanent sensory deficit was 67% after C5-C8 nerve root resection. Dumbbell tumours were associated with the need for total or ventral nerve root transection as well as with a high incidence of tumour recurrence. The incidence of permanent neurological deficit was significantly higher in patients undergoing C5-8 nerve root resection. In our first case, excision of the mass was done by preserving the phrenic nerve trunk of C5 dissected, perineurium of tumour incised and dissected then tumour separated from inferior end upwards preserving C6. In another case we found that swelling was dumbbell shaped which was successfully removed with intracapsular dissection through neck incision along with intervertebral part doing laminectomy. Postoperatively no neurological deficit was noticed. Microscopically, schwannomas are encapsulated, solid or cystic tumors. They can be composed of two cellular zones: Antony type A, densely arranged with spindle-shaped Schwann cells and areas of palisading nuclei,Verocay bodies and Antony B, characterized by a hypo cellular arrangement and a large quantity of myxoid tissue.
Extracranial schwannomas in the head and neck region are rare neoplasm. Diagnosis is established by imaging studies such as magnetic resonance imaging or computed tomography, while FNAC is used to rule out other condition. Histopathology gives definitive diagnosis. The accepted treatment for these tumors is surgical resection with preservation of the neural pathway.