Cervical Spinal Cord Compression by A Plexiform Nodule in Neurofibromatosis Type 1 Treated Surgically by Posterolateral Approach: About A Case with Post Traumatic Revelation
Neurofibromatosis type 1 or Recklinghausen’s disease is an autosomal dominant disease. Its diagnosis is made in the presence of 2 of the following signs: at least six café-au-lait spots of more than 5 mm in their greatest diameter in pre-pubertal individuals, and of more than 15 mm in pubescent individuals, at least two neurofibromas (benign non-cancerous tumors) of any type or one plexi-shaped neurofibroma, axillary or inguinal lentigines (freckles), one optic glioma, two Lisch nodules. Nodular neurofibroma can develop in the spinal canal and cause spinal cord compression. Spinal cord compression may or may not be symptomatic. We report the case of a 25-year-old patient, received in a sudden onset tetra paresis, after falling from the top of a tree. He presented with type 1 neurofibromatosis with a plexiform nodule under the median cervical dural next to C2, diagnosed on MRI. He had been treated surgically via a posterolateral approach with complete resection and electrocoagulation of the plexiform pedicle. A vertebral vascular injury was noted intraoperatively. He had recovered well from his deficit, despite the occurrence of sepsis, complicating an infection of the surgical wound.
Keywords: Neurofibromatosis Type 1, Brutal Tetra Paresis; Spinal Cord Compression; Surgery
Neurofibromatosis type 1 (NF1) or Von Recklinghausen disease is the most common neurogenic disease affecting adults and children. It is inherited autosomally dominant [1]. Its diagnosis is made on the basis of the presence in a patient, of the association of at least two of the following: Six coffee-au-lait spots of more than 5mm in the large diameter in the prepubertal subject, and more than 15 mm in pubescent subjects; two or more neurofibromas or one plexiform neurofibroma; axillary or inguinal lentigines; optic gliomas; at least Lisch nodules; a characteristic bone lesion; cortical thinning of the long bones with or without pseudarthrosis [2]. The plexiform neurofibroma can develop in the spinal canal and cause spinal cord compression [3]. The lesion may be asymptomatic and does not always need treatment. It can be symptomatic with neurological deficit requiring surgical resection [3, 4].
We report the clinical case of a 25-year-old patient, carrier of neurofibromatosis type 1 and having presented sudden onset tetra paresis, after a fall from the top of a tree. His trauma had decompensated his pre-existing spinal cord compression, due to a plexi-shaped nodule. His surgical treatment had allowed complete neurological recovery.
He is a 25-year-old man, single, tree feller. The diagnosis of neurofibromatosis had been made in him since the age of 13 and he had undergone the excision of a dorsal nodule. He had no other specific background.
After having stayed for five months, in a peripheral hospital, for treatment of functional impotence of four limbs, without improvement, he was referred to the Laquintinie hospital in Douala. The onset of his illness dates back to 5 months, following a fall from the top of a tree nearly 8 meters high, with landing on the left hemibody. Sudden functional impotence of the four limbs followed, for which he had consulted in the referring hospital.
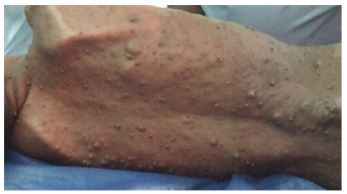
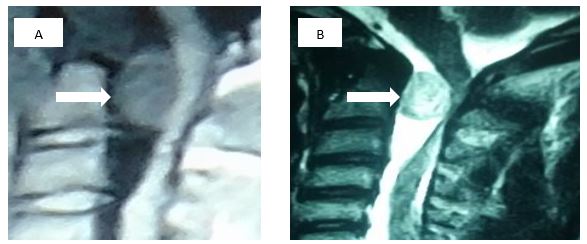
On admission to the referral hospital, he presented with tetraparesis in the form of cramps and tingling leading to functional impotence of the limbs, especially the lower limbs, with difficulty in walking. On physical examination, the patient was conscious with a Glasgow score of 15/15. He presented with multiple “café au lait” spots with several plexi-shaped cutaneous nodules (Figure 1) and lentigine lesions in the axillary (Figure 2) and inguinal folds, tetraparesis with spastic hypertonia. Motor strength in the lower limbs was rated 3/5 on the left and 4/5 on the right, with a positive Hermit’s sign. No damage to the pairs of cranial nerves was noted. Babinski’s sign was positive in both feet. All the osteo tendon reflexes were lively. The rest of the exam was unremarkable. A cervical MRI was performed and showed, in T1 and T2 sequence, an anterior spinal extra-medullary intracanal mass with level C2 spinal cord compression (Figure 3).
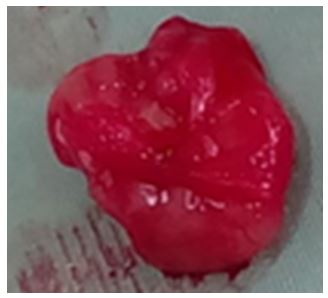
The patient had been treated surgically via a posterolateral approach in order to better control the tumour, the spinal cord and the cerebrospinal fluid (CSF). Peroperatively, a mass 3 cm in large diameter (Figure 4) was found , intracanal, subdural and extramedullary plexiform, on the anterior face of the spinal cord, with an implantation base on the dura- mother. This mass had been completely resected with coagulation of the plexiform pedicle. The intraoperative incident was the occurrence of a wound in the right vertebral artery, but repaired. The postoperative course was marked by E. coli sepsis on an infection of the surgical wound on the second postoperative day. This infection had been well treated with antibiotics for ten days with a good evolution. Physiotherapy had been initiated from the fifteenth postoperative day, after healing of his wound. The patient was at home on the thirtieth postoperative day, walking with a cane. He had completely recovered from his neurological deficit on the forty-fifth postoperative day and was walking without a cane, going about his business freely.
The skin lesions observed in our patient were those classically described in the literature [1, 3]. The age of presentation of neurofibromatosis type 1 is between the first decade and the seventh decade of life (2 ends of life) [3, 5]. Neurofibromatosis type 1 (NF1) is a genetic disease resulting from mutations in the tumor suppressor gene NF1, which encodes neurofibromin; The causative gene, NF1, located on chromosome 17, [6,7] Legius syndrome , also called NF1-like, is an autosomal dominant genetic disease, a RASopathy with most overlap with NF1. It is characterized by six or more café au lait spots similar to NF1 with or without skin freckles. It results from a mutation in the heterozygous gene in SPRED1, located on chromosome 15 [8]. In the absence of genetic testing, the difference between the two diseases is difficult to establish. This test was not possible in our context.
The diagnosis of neurofibromatosis was made in our patient at the age of 13 by analysis of the skin biopsy specimen and on the basis of signs of cervical spinal cord compression which had suddenly set in following a fall from the top of his chest. a tree, at the age of 25. Although the age of diagnosis of the disease is close to that described by JR Leonard et al. [5], the installation mode is brutal contrary to the work of Taleb FS et al. [8] who describe the onset of a myelopathy that gradually sets in following slow spinal cord compression by the plexi nodules forming neurofibromatosis. Tetra paresis, which is the inaugural sign in our patient, is the main clinical presentation of cervical spinal cord compression by plexiform nodules in Recklinghausen ‘s disease [2, 5]. Jeffrey Gold et al, however, operated on a child with a large; This compression is symptomatic in 1.6% of patients [9].
The plexiform nodules are intradural, extramedullary in 72%, extradural in 14%, and intramedullary in 1% [2]. Surgical treatment by laminectomy via the posterior approach is described as the main way of approaching symptomatic intra-canal compressions of plexiform nodules of neurofibrofibromatosis [2, 4, 5]. This laminectomy is associated with instrumentation to avoid kyphosis in the work of Garg et al [3]. In the anteromedial compression of the spinal cord, as in the case of our patient, the spinal cord being compressed by the nodule, its mobilization in search of the pedicle of the nodule can lead to spinal cord contusion and cause an aggravation of the neurological deficit; the anterolateral approach allows direct access to the plexiform nodule, control of its implantation base, cerebrospinal fluid and spinal cord [9, 10]. This pathway had been used and had led to a gradual and rapid recovery from the neurological deficit. The intraoperative incident was the injury to the right vertebral artery which had been well controlled. Our clinical case has certain limitations, namely : vertebral angiography, if available, is indicated in the preoperative assessment to better guide the surgical approach [10, 11]. This examination, although important, was not available for our patient. Sepsis, following infection of the surgical wound by an enterobacteria (Escherichia coli), described in our patient, was linked to insufficient intraoperative and postoperative asepsis.
Chromosomal examinations to confirm neurofibromatosis Type 1 were not requested, due to the insufficient technical platform.
We presented a case of sudden onset tetra paresis in a patient diagnosed with neurofibromatosis 12 years previously. His medullary compression by the plexi nodule formed under dural and extra medullary median anterior, until then asymptomatic, had been able to be treated surgically by first posterolateral approach with a complete recovery of his inaugural tetra paresis after forty-five days. However, performing an arteriography before surgery could have prevented the occurrence of a vertebral vascular injury. Per and post-operative asepsis remains a major challenge in our context. His trauma had decompensated his pre-existing spinal cord compression, due to a plexi-shaped nodule, diagnosed on MRI.
Case support: Fondop
Writing of the article: Fondop, Atyam
Critical review: Atemkem, Amougou, Banga, Dogmo, Ndouma, Fuentes
Conflict of Interest: the authors declare no conflict of interest for the publication of this case
Ethical Considerations: The patient has given written consent for the publication of this case