Cystic Neck Masses – A Diagnostic and Management Challenge
Cervical metastasis is often the only presenting feature in patients with squamous cell carcinoma of the head and neck (HNSCC). These metastases frequently undergo cystic degeneration, and may be difficult to distinguish from other benign cystic squamous lesions of the head and neck. Fine needle aspiration for cytopathology (FNAC) is frequently performed, but the results obtained may not be conclusive. P16 immunohistochemistry may be carried out. However, the value of this test in differentiating between benign and malignant cystic lesions of the head and neck remains unclear.
Keywords: Cystic Neck Masses; P16 immunohistochemistry; HPV associated HNSCC
We discuss the case of a 41 year old gentleman referred to the one-stop clinic with a neck mass. An ultrasound scan and FNAC and subsequent excision biopsy showed a squamous lined cystic lymph node, with some focal positivity for cytoplasmic p16 staining. The pathology was potentially in keeping with a benign cystic lesion however a metastatic SCC could not be excluded.
Cervical metastasis is often the only presenting feature in patients with squamous cell carcinoma of the head and neck (HNSCC) [1]. These metastatic foci frequently undergo cystic degeneration, and may be difficult to distinguish from other benign cystic lymphoepithelial lesions of the head and neck [2]. Cervical metastates from primaries in the oropharynx have been shown to be more likely to undergo these cystic changes in comparison to squamous cell carcinoma from other head and neck sites [3-5].
During the investigative work up of these cases, fine needle aspiration for cytopathology (FNAC) may be performed. However, the results obtained are not always diagnostic. To increase the specificity of FNAC, immunohistochemistry for p16 is often performed, as p16 overexpression has been shown to act as a surrogate marker of Human Papilloma Virus (HPV) associated HNSCC [6] HPV, particularly subtype 16, has been shown to be a causative agent in a subset of HNSCC [7,8]. The majority of these HPV related carcinomas localise to the tonsil; which in turn is the most common site for primary tumour in the context of cystic metastasis [3,9]. Hence, previous studies have shown p16 positivity to thus correlate with oropharyngeal primary tumours [10].
Nonetheless, the value of this marker in the differentiation between benign and malignant cystic lesions of the head and neck remains unclear. A case series by Pai et al showed that p16 staining was negative in all aspirates of branchial cleft cysts sampled (n = 4), and positive in 36% of the aspirates from malignant SCC cysts (n = 11) [11]. In contrast, a series reported by Cao et al also evaluating p16 staining in aspirates from cystic neck lesions, reported that up to 42% of benign lymphoepithelial lesions (n = 12) and 19% of malignant squamous lesions (n = 16) were positive for p16 [2].
A 41 year old male patient was referred to the one-stop clinic with a two week history of a left sided neck mass. The patient did not report any aero-digestive symptoms or other systemic symptoms of note and was a non-smoker. There was no previous medical history of note, and the patient was not on any regular medications.
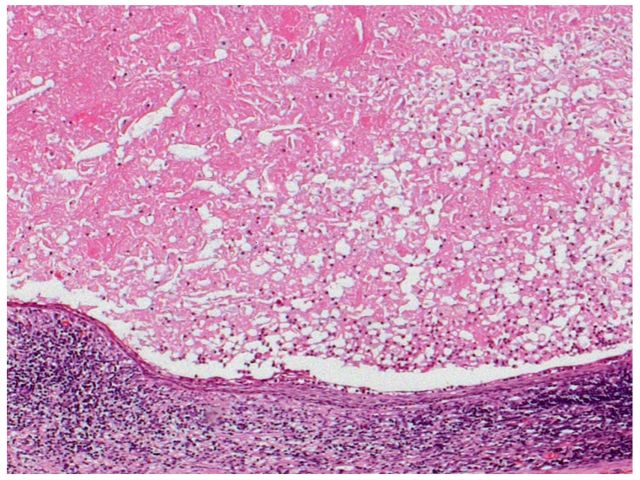
On examination a soft, cystic mass was present on the left side at level III; head and neck examination including flexible nasoendoscopy were unremarkable. An ultrasound scan of the patient’s neck revealed a single abnormal 2.3cm lymph node at level III, containing some focal areas of intranodal necrosis, consistent with features of a lymphoproliferative neoplasia or metastatic squamous cell carcinoma. FNA was undertaken and the results showed numerous degenerate, mildly atypical superficial squamous cells on a necrotic background. These features were also suspicious of a metastatic squamous cell carcinoma (Figure 1).
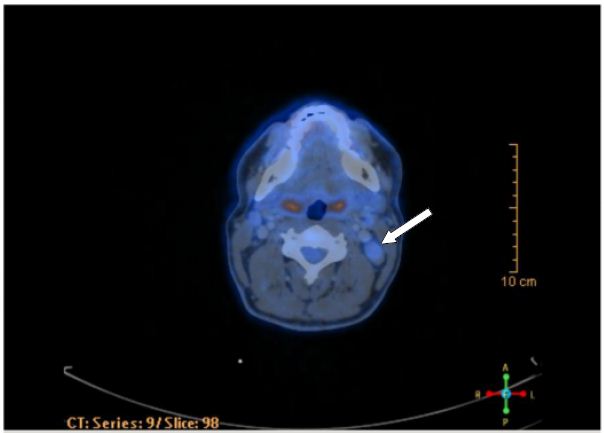
In light of his normal clinical examination, the patient underwent an urgent CT scan of the neck and whole body PET-CT scan to investigate for an underlying primary tumour. This did not identify any significant metabolic activity within the suspected lymph node, and confirmed it to be largely necrotic. There was also no other primary site of disease demonstrated (Figure 2-3).
The patient underwent an excision biopsy of the suspected lymph node and the pathology from this confirmed a squamous lined cystic lymph node, with no cellular atypia of the squamous cells or within the lymphoid component.
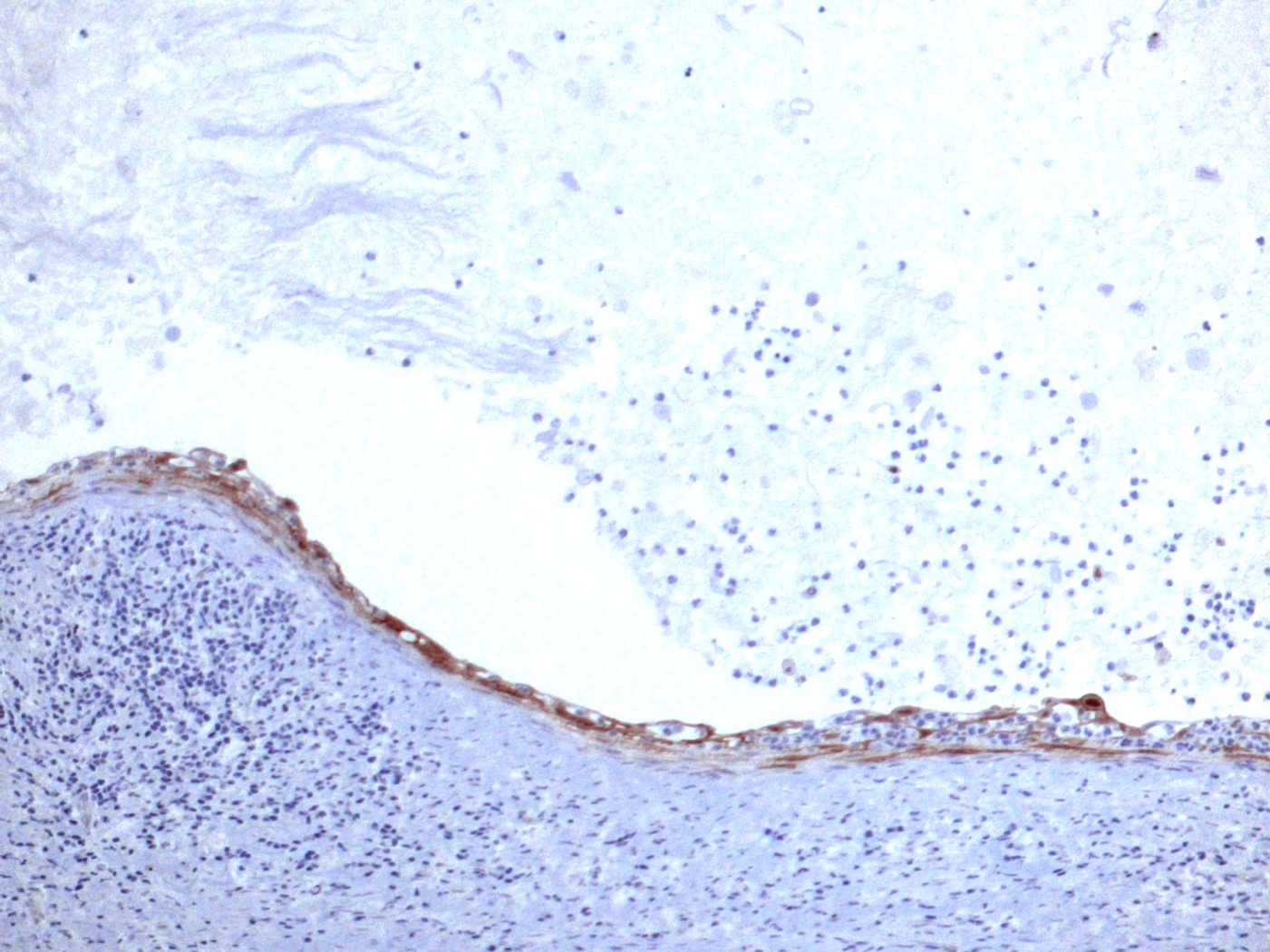
A stain for p16 demonstrated some focal positivity in the superficial squamous cells, which was of uncertain significance (Figure 4). The features were consistent with a lymphoepithelial brachial cleft cyst. However, in light the previous radiological findings and consideration of the patient’s age group, a well differentiated cystic metastatic squamous cell carcinoma could still not be excluded.
The case was discussed at a multi-disciplinary meeting and it was agreed to offer the patient one of two options. The first of these was reassurance of the results obtained so far, with regular close surveillance. The alternative option was a bilateral tonsillectomy and multiple biopsies from high risk primary sites, in particular the oropharyngeal region, as this subset of HNSCC can typically lead to metastatic cystic lesions. They are also the area’s most commonly associated with HPV related HNSCC subtype. After discussion with the patient, he was keen to proceed with further biopsies, for a definitive diagnosis. He underwent bilateral tonsillectomy, with biopsies from the post cricoid, left pyriform fossa, left tongue base and the post nasal space. The histopathology results from all these specimens were normal, with no evidence of dysplasia or invasive squamous cell carcinoma.
Distinguishing between benign lymphoepithelial cysts and malignant cystic metastasis in the head and neck can be challenging. The investigative work up should include imaging to review of any underlying primary malignancy in the head and neck, and to also asses for the presence of branchial anomalies.
Fine need aspiration for cytopathology is often carried out but may not always be diagnostic. The role of p16 immunohistochemistry remains unclear. This marker has been shown to act as a surrogate marker for HPV related HNSCC [6], and this SCC subtype is typically found in the oropharynx region. It has been reported that SCCs from the oropharyngeal region are the most common primary sites for cystic type metastasis in the head and neck [3,9], hence the intuitive value of p16 staining in these cases. However, case series and reviews to date have provided confounding evidence regarding the value of p16 staining in differentiating between benign lymphoepithelial cysts and metastatic cystic lesion, thus limiting its diagnostic use [2,11].
It has also been suggested that p16 overexpression in the head and neck may thus not always be directly related to HPV infection and DNA integration (with or without potential conversion to SCC). In tonsillar tissue p16 staining is greatest in the areas involved in antigen filtering, namely the reticulated epithelium of the tonsillar crypts [12,13]. Various studies have commented on the histological similarities between lymphoepithelial cysts and tonsillar crypt epithelium [14-16], leading to the postulation that the former may develop from an embryolgically displaced latter or even from dislodged crypt epithelium during bouts of tonsillitis [16,17]. The presence of p16 overexpression in benign lymphoepithelial cysts may thus be accounted for if this suggested relationship is considered valid.
As a result of the potential difficulty in distinguishing between benign lymphoepithelial cysts and malignant cystic metastasis in the head and neck, these patients may pose a significant diagnostic and management challenge. Such patients should be discussed within a multi-disciplinary environment and a detailed discussion of the options available should be discussed with the patient. The options of a ‘watchful waiting’ policy, with close observation and regular full ENT assessment, compared with surgery for a definitive diagnosis, should be considered in the context of each patient individually.