Decreased Radiation Exposure Using Navigated Minimally Invasive Transforaminal Lumbar Interbody Fusion Compared To Fluoroscopy
Minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) has been celebrated as a technique for decreasing patient’s post-operative pain, decreased blood loss in the OR and shorter hospital stays. It has come under criticism recently due to the perception that the radiation exposure to the patient, surgeon and operating room staff are increased in comparison to its open counterpart. This study assesses radiation exposure between the fully navigated versus conventional fluoroscopic MIS TLIF techniques using the C-arm and K-wires.
Methods: Retrospective chart review was completed for the senior author’s 1 and 2 level MIS TLIFs performed consecutively from 2004 to 2014. The surgeries from 2004 to 2006 were performed with fluoroscopy, and the surgeries from 2006 to 2014 were performed only using neuronavigation. Radiation exposure was recorded at the end of each case by the radiology department.
Results: Over this time period, 391 single level and 200 2 level navigated MIS TLIFs were performed. Over the same period, 71 single level and 26 2 level MIS TLIFs were performed using conventional fluoroscopy. The total radiation dosing per procedure was 86.4 mGy for one level and 89.2 mGy for 2 level neuronavigated TLIF. For conventional fluoroscopy, there was 121.8 mGy for single level and 182.1 mGy for 2 level TLIF. Both single and 2 level MIS TLIFs met statistical differences in radiation dosing to the patient.
Conclusion: Fully navigated MIS TLIF provides a viable alternative to the conventional MIS TLIF with decreased radiation exposure to the OR staff, surgeon and patient.
Keywords: MIS TLIF; Radiation; Stereotactic-Navigation
Minimally invasive spine techniques have gained widespread popularity and acceptance in the recent years due to minimizing soft tissue dissection, shorter hospital stay, and shorter recovery period [1-3]. Historically these procedures have been have been done with conventional fluoroscopy using Kirchner wires (K-wires). The technique was first described by Foley, et al., and is largely imaging dependent for screw placement sometimes using high amounts of fluoroscopy time to ensure safe placement of the hardware as anatomic landmarks cannot be used with this technique [4]. In recent years, there is an increasing awareness of the high amount of radiation dosing that occurs in the OR to surgeons, OR staff and patients. It has become a goal of surgeons to find techniques that decrease the cumulative radiation exposure to all individuals in the OR setting [5].
At our institution, the routine use of intraoperative navigation for placement of pedicle screws and grafts began in 2005 for both open and MIS procedures. Using these fully navigated techniques for both screws and interbody grafts, allows the surgeon and operating room staff to leave the room during the 3D image acquisition and stand behind a lead wall during localization, so the dose is negligible. In addition, it allows the surgeon to forgo the use of lead shielding while operating, increasing surgeon comfort. These techniques also allow the bed to be placed at optimal height for operating-negating the need for elevated steps-and allows the surgeon to stand in the location of his or her choosing without having to work around the C-arm.
In addition to increasing surgeon comfort, while decreasing radiation exposure to the surgeon and OR staff, navigation provides the added benefit of allowing better visualization of the bony anatomy in both the very obese and osteopenic patients. It has been well studied that increasing Body Mass Index (BMI) leads to increasing radiation exposure due to the need to increase the amount of boost used in the C-arm, as well as increasing the number of acquisitions, for the surgeon to be comfortable with the often-times obscured anatomy [6]. In our patient population, the average BMI is greater than 35. Thus, navigation allows 3D visualization without having to move the C-arm back and forth between AP and lateral increasing the speed of the procedure, while having the added benefit of allowing the surgeon intraoperatively to check the exact position of the screws and grafts before closing.
This study looks to compare the radiation dosing between conventional fluoroscopic guided MIS TLIFs and fully navigated MIS TLIFs to surgeon, OR staff and patients.
Indiana University Institutional review board approval was obtained for this study. A retrospective review was performed for all 1 and 2 level MIS TLIF procedures from January 2004 to January 2014. Records of each patient’s surgery and approach are listed in the office records. The operative reports and intra-operative fluoroscopy reports were reviewed to evaluate C-arm versus navigation technique and radiation exposure to patients. From 2004 to 2006, MIS TLIFs were performed using the classic Foley technique incorporating K-wires and fluoroscopy and thereafter all were done with navigation. All surgeries were performed by the senior author (J.P.M), who is a fellowship-trained spine surgeon. The four categories of 1 and 2 level MIS TLIFs using fluoroscopy and navigation were then compared using Chi-squared statistical analysis to assess for significance in any differences found.
For the traditional technique using fluoroscopy, a GE 9900 Elite C arm was used. This fully navigated TLIF is described using original Medtronic O-arm imaging, Sextant or Voyager percutaneous screw systems, and METRx tubular retractor system (Medtronic; Memphis, TN). The posterior superior iliac spine is palpated and the percutaneous pin is placed into the iliac spine in a medial to lateral trajectory, then the reference arc is attached. Following this, the 3-dimenstional image is obtained with the surgeon standing behind a lead wall for the localization films, and the rest of the OR staff standing outside of the room minimizing radiation exposure during this step.
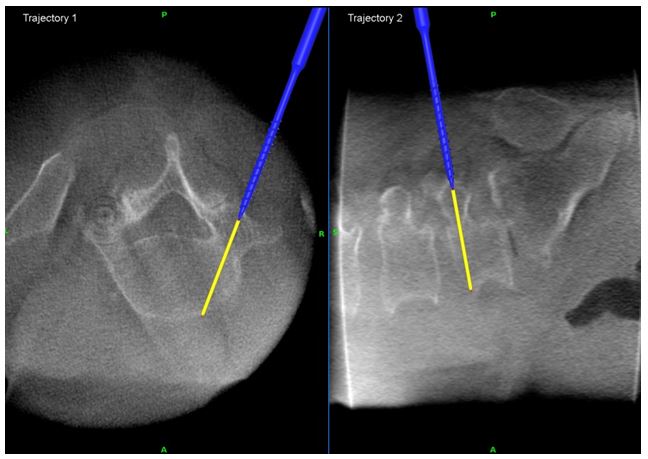
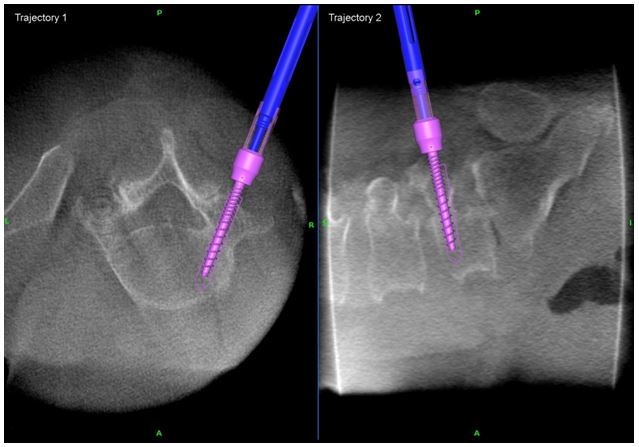
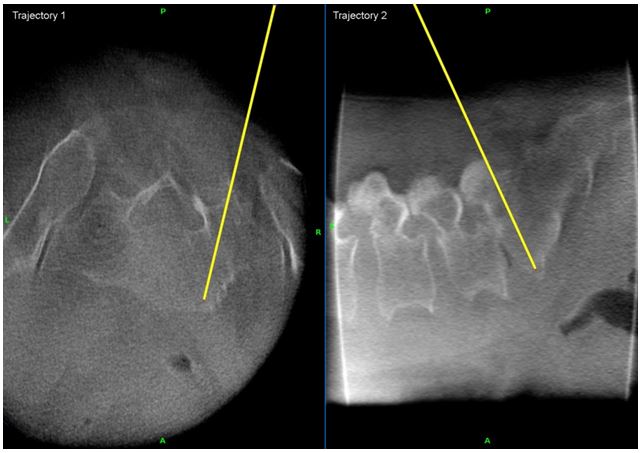
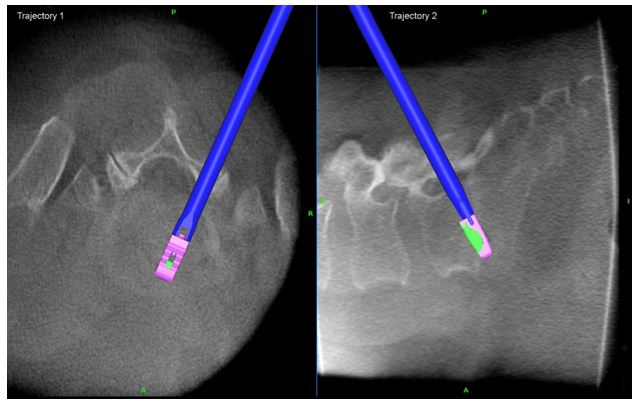
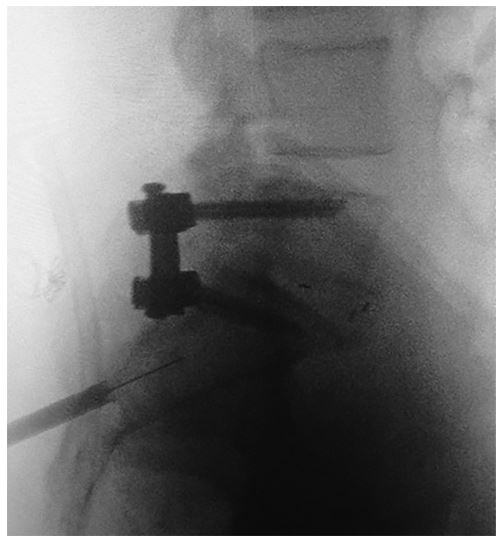
The navigation instruments are registered against the reference arc with care not to displace the arc from its position, and the skin incision is planned using the navigation as seen in Figure 1. A finger is utilized to dilate a pathway through the muscle, so there is less injury to the muscle when passing the instruments down to the pedicle entry point. The navigated awl-tip tap, along with a tissue protector, is used to tap screw trajectory as well as measure screw length as seen in Figure 2. On the side contralateral to the decompression and interbody work, the screws are placed immediately after the pedicle is tapped, using the image guided screwdriver. The screw is simply passed down the dilated tract in the paraspinal musculature and the tip of the screw drops into the previously tapped hole. This is confirmed both by feel and by seeing it match the saved trajectory on the stealth station. For the screws that will be placed on the ipsilateral side, after the decompression has been completed, in place of K-wires, plans of tapped trajectories are saved on the navigation as shown in Figure 3 and described by Gianaris, et al. The decompression is performed with the operating microscope and 22 mm tubular retractor using a combination of kerrisons and the drill [7]. Once the disc has been removed and the endplates have been prepared for arthrodesis, the rhBMP-2 and local autograft is inserted into the disc space and pushed to the contralateral side with pituitary forceps. Use of rhBMP-2 in the disc space is an off label use of rhBMP-2 but recent studies have suggested that it can increase fusion rate with a low complication profile [8]. The TLIF graft is then inserted under navigation showing lateral to medial trajectory as well as depth as shown in Figure 4. The tubular retractor is then removed, and the screws are then placed into the previously tapped pedicles, using the saved trajectories. The rods are passed down through the Voyager extenders into the screw heads. Compression is then applied and the set screws are tightened into the final position. The screw and graft positions are checked using an O-arm acquisition in similar fashion as the first spin while the surgeon and staff step out of the room. Figure 5 shows the final result.
From January 2004 to January 2014, 688 MIS TLIF’s were performed. During this same time period, 391 single level and 200 2 level fully navigated MIS TLIFs were performed, and 71 single level and 26 2 level conventional MIS TLIFs were completed. All MIS procedures were done by one senior fellowship-trained surgeon (J.P.M). The different patient populations were compared by Chi-squared test with significance being assessed at p values of <0.05.
There were no significant differences in patient demographics. Patients were largely categorized into four groups: single and 2 level MIS TLIFs using neuronavigation and single and 2 level conventional MIS TLIFs. Ages ranged from 35–74 and 41–81 years in single and 2 level navigation groups, respectively and 24-87 and 36-70 years in the single and 2 level conventional groups, respectively. Mean ages were 56.3, 59.4, 57.7 and 54.3, respectively, for the different surgery types. BMIs for all four groups were above 35. This data is shown in Table 1.
The radiation doses were compared between the navigated and conventional TLIFs. The amount of fluoroscopy shooting time was calculated per surgery as well as the emitted radiation dosing that we keep on file at our institution. The total radiation dosing per procedure for the navigation group was 86.4 mGy for one level MIS and 89.2 mGy for 2 level surgeries. For conventional MIS TLIFs, dosing was 121.8 mGy for single level and 182.1 for 2 levels. Chi-squared testing was done with a p value of less than 0.05, and when comparing single level TLIFs to each other and 2 level TLIFs to each other, the compared groups reached statistical differences to patient radiation dosing. This is demonstrated in Table 2. The radiation dosing for the fully navigated MIS TLIF represents 2 O-arm acquisitions with the stated dosing relating to the settings on the O-arm that were used. It does go without saying that dosage to surgeon and OR staff is negligible with the fully navigated technique where at the very least the surgeon and the scrub receive high doses of radiation during the conventional technique.
It should be acknowledged that in this study, the technique for placing percutaneous screws utilizing fluoroscopy has evolved in the past 10 years and there are techniques that utilize less fluoroscopic time for this procedure [9]. Still, the repeated radiation dosing to the OR staff and surgeon is something that cannot be minimized with flouroscopy, and the use of spinal navigation with the appropriate safety precautions, makes this radiation exposure negligible.
Although most proponents of the MIS TLIF will acknowledge that navigation decreases radiation to the OR staff and surgeon, the prevailing thought is that this is at the expense of increased radiation to the patient. This study is the first comparing the radiation dosing of these two procedures, and the findings show that radiation to the patient is actually decreased. Furthermore, in many of the patients such as the elderly with their decreased bone mineral density or obese patients, in whom using minimally invasive techniques may be best suited, fluoroscopic techniques can be very challenging, leading to even longer fluoroscopic times with increasing boost usage. This makes the difference in radiation dosing even more pronounced.
Operating room safety is of utmost importance to both the patient and providers, and other centers have looked at or proposed studies to better evaluate this. Kim, et al., looked at radiation exposure with fluoroscopy vs navigation in a cadaveric study of 18 TLIF’s and found decreased radiation [10]. Although our study is retrospective review, other centers have proposed prospective randomized trial designs to evaluate the differences in radiation exposure [11]. Our study helps confirm the significant decrease is radiation to both patient and OR staff.
It is also important to note that while the radiation dose increased 66% when going from a 1 level procedure to a 2-level procedure utilizing the fluoroscopic technique, there was no change in radiation dose to the patient in the navigation group.
The fully navigated minimally invasive TLIF provides all of the already established advantages afforded by minimally invasive surgery including less blood loss, lower infection rate, and shorter hospital stays while providing the benefit of decreased radiation to the surgeon and OR staff. Furthermore, radiation dose to the patient in a minimally invasive TLIF is less when utilizing spinal navigation, when compared to the fluoroscopic based technique. The fully navigated nature of the MIS TLIF in this study, affords decreased radiation dosing to the patient, surgeon and OR staff, while allowing the surgeon to operate without lead at a comfortable bed height.
Dr. Mobasser is a consultant and receives royalties from Medtronic. He also receives royalties from Innomed, Inc.