Diffuse Dermal Angiomatosis of the Breast: Two Case Reports and Literature
Objective: Diffuse angiomatosis is characterized by diffuse proliferation of benign endothelial cells in the dermis. Although it was previously believed that the lower limbs were the most frequent site of presentation, it now seems that the disease occurs most commonly in the breast. A number of treatment approaches have been used, although none appears to be effective in managing this condition.
Case report: We present two cases of diffuse dermal angiomatosis of the breast in middle-aged, smokers women who had large, pendulous breasts. Definitive treatment used in the two cases presented here were both smoking cessation and surgery.
Conclusion: Findings suggest that smoking cessation and surgical management brings about the most favorable results, although further studies are required to confirm this hypothesis.
Keywords: Breast; Reactive angioendotheliomatosis; Smoking habit
Diffuse dermal angiomatosis of the breast, a type of reactive angioendotheliomatosis, is a rare condition, and one that appears to be most frequently located in the breast rather than the lower limbs [1]. Clinical presentation involves poorly circumscribed plaques or ulceration of the breasts without associated scarring, and painful lesions with prominent vessels surrounding them [2-4]. The number of lesions can range from a few to many. Several predisposing factors have been described, though the most important are large, pendulous breasts and smoking habit.
A 61-year-old woman with a relevant past history consisting of obesity (BMI: 37), dyslipidemia treated with simvastatin, and depression treated with fluoxetine and lorazepam. Relevant gynecologic and obstetric history included a previous Cesarean section. She reported no alcohol intake, although she smoked 10 cigarettes a day. One year prior, the patient began to manifest telangiectatic vascular proliferation in the left breast covering an area of 5 cm in diameter in the superomedial area, which developed ulceration and bleeding. In the 4 to 5 months after this ulceration and bleeding resolved, she developed the same lesions in the left breast, which also ulcerated on a number of occasions. Both breasts were abnormally large in size (Figure 1).
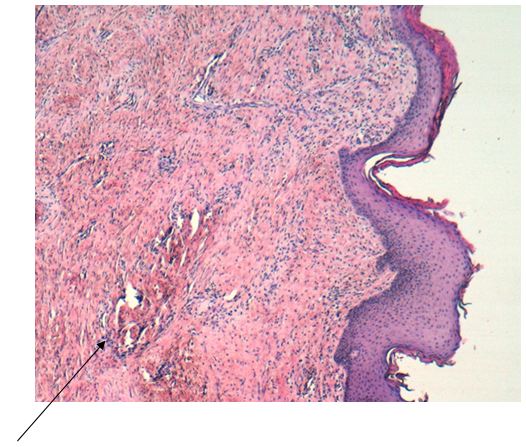
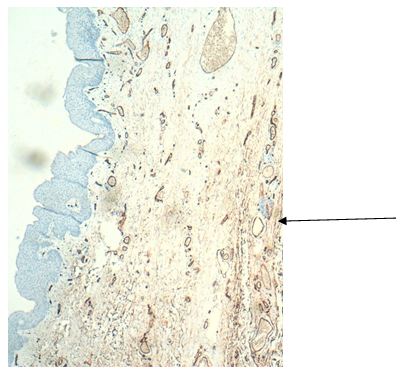
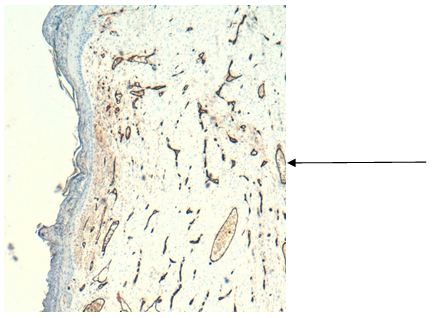
A skin biopsy was performed of the affected area, revealing reactive vascular proliferation in the dermis. Immunohistochemistry for estrogen receptors, HHV8, WT1, and C-myc was negative in whole samples (Figure 2,3 and 4). Therefore, in light of the patient’s medical history, physical examination of both breasts, and the findings of the skin biopsy, a diagnosis of diffuse dermal angiomatosis of the breast was reached.
We screened for presence of an occult malignancy by carrying out chest radiography, abdominal ultrasonography, tests for tumor markers, and mammography and ultrasound scan of both breasts, all of which produced negative results. In order to rule out veno-occlusive disease and hypercoagulability, a broad screening for thrombophilia and auto-immune disease was performed, though the only finding was mild hyperhomocysteinemia, and CT-angiography ruled out obstruction of the supra-aortic trunk.
The patient was encouraged to lose weight and discontinue her smoking habit and was prescribed enoxaparin 30 mg every 12 hours, acetylsalicylic acid 100 mg once daily, and folic acid 5 mg daily for regulation of mild hyperhomocysteinemia. However, due to progressive worsening under the aforementioned therapy, the patient was treated with oral isotretinoin 20 mg/day, after which the dose was increased to 40 mg daily. The patient began the treatment without showing signs of side effects of isotretinoin. Following treatment with isotretinoin and total cessation of her smoking habit, the patient presented partial improvement of the lesions with a decrease of the vascular pattern. As a result, reduction mammoplasty was performed to achieve total resolution, but the lesions recurred after the surgery (Figure 5 and 6).
A 50-year-old female patient presented to our department. Her relevant medical and surgical history included hemorrhoids, for which she had undergone surgery 10 years prior. She reported no intake of alcohol, although she was a smoker. A physical examination revealed megalomastia in both breasts and an erythematous lesion in the upper outer quadrant of the left breast measuring 1 cm containing a small orifice through which a transparent fluid oozed. All of these signs and symptoms were indicative of diffuse angiomatosis of the breast. The results of an ultrasound scan revealed the lesion to be BI RADS category 2.The patient was instructed to discontinue her smoking habit and was administered antibiotic therapy. Later a surgical excision of the lesion was performed; through circular incisions on the skin the affected area was removed, leaving a margin of 1mm.
Diffuse dermal angiomatosis of the breast is a rare type of reactive angioendotheliomatosis [1]. Although it was previously believed that the lower limbs were the most frequent site of presentation, it now seems that the disease occurs most commonly in the breast with bilateral presentation [1]. Indeed, the literature contains several cases of the disease with this pattern [1-8]. Histopathologically, the disease is characterized by diffuse proliferation of benign endothelial cells in the dermis, which are immunohistochemically positive for CD31, CD34, and SMA- α, and negative for HHV-8 [1,5,6]. The histopathological differential diagnosis should include acroangiodermatitis, Kaposi sarcoma, and low-grade angiosarcoma [1,5]. Clinical presentation is varied, though in most cases consists of poorly circumscribed plaques or ulceration of the breasts that do not scar, are painful, and have prominent vessels surrounding the lesions [2-4]. There is often a leakage of fluids in the area of ulceration, causing discoloration of clothing [4].
A number of predisposing factors have been described, including middle age, tobacco consumption, obesity, abnormally large breasts, heart disease, veno-occlusive disease, gestational hypertension, trauma, calciphylaxis, diabetes mellitus, and hyper coagulable states such as antiphospholipid syndrome [1-5,7].
Regarding pathogenesis, the aforementioned risk factors promote prolonged ischemia in the tissues, thereby favoring the appearance of endothelial growth factors and causing the proliferation of new blood vessels [2,3,5,7,9]. Additionally, as this area is rich in fatty acids, repeated trauma may give rise to angiogenesis [2].
Currently, treatment consists of smoking cessation and, where present, monitoring of cardiovascular risk factors such as hypertension and dyslipidemia [5]. A number of treatments have been administered such as isotretinoin, oral steroids, acetylsalicylic acid and pentoxifylline, although the results have been inconsistent [2,4]. The literature contains reports of cases treated with isotretinoin; in many cases, however, this approach has not been totally effective [1,2,4,7]. The antiangiogenic effects of isotretinoin may explain the improvements seen in the symptoms [2].
In one reported case, the disease resolved when the patient received a stent as treatment of left subclavian artery occlusion , and in other cases, the disease has resolved with surgical excision of the affected area and with reduction mammoplasty or mastectomy [1,3,4,6,7,9]. Indeed, it is recommended to discuss possible surgical treatment of diffuse angiomatosis of the breast with reduction mammoplasty for patients in whom medical therapy has failed, while mastectomy should be the last resort following failure of more conservative options [4]. The different treatments and their outcomes retrieved from the literature are presented in (Table 1). In the first case described in this report, treatment consisting of smoking cessation and medical therapy with anticoagulants and isotretinoin was not entirely effective, after which reduction mammoplasty was performed to achieve complete resolution. On the other hand, treatment consisted of smoking cessation and excision of the affected area of the breast.
Diffuse dermal angiomatosis of the breast is probably more frequent than once believed. Accurate diagnosis is important to achieve correct treatment. For this reason, proper study of the patient’s symptoms, past medical history, smoking and alcohol intake, and physical examination are also important. Studies must also be performed to detect possible hypercoagulability and screen for veno-occlusive disease. It is also important to recommend that the patient discontinue their smoking habit.