Early Vitamin K Deficiency- A Rare Presentation
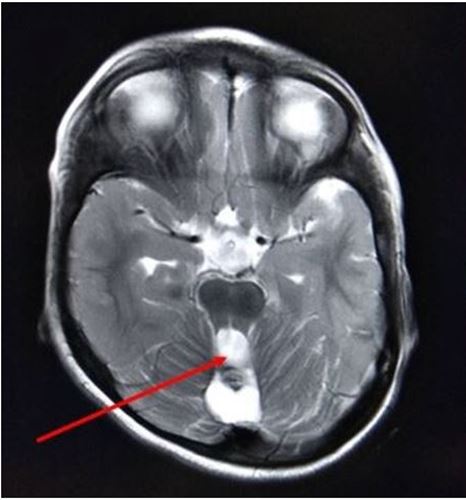
Background: Early Vitamin K deficiency (EVKD) bleeding is most commonly due to maternal medications. Case Characteristics: A 3-year-old girl with a history of mother being treated with Anti-Tubercular therapy during pregnancy had bleeding due to EVKD during the early neonatal period & presented with cerebellar ataxia. MRI was suggestive of midline hemorrhage involving the cerebellum and vermis. Message: Infants prone to EVKD bleeding should receive Vitamin K at birth.
Keywords: Cerebellar Ataxia; Early Vitamin K Deficiency Bleeding; Anti-Tubercular Drugs
Vitamin k is an anti-hemorrhagic factor that is needed for the synthesis of functional forms of factor II, VII, IX, and X in the liver. Once activated in the blood, they become available to take part in the coagulation process, a complex series of events that results in the conversion of fibrinogen to fibrin and the formation of a hemostatic plug. The consequence of vitamin k deficiency results into a hypocoagulable state, however, the hemostatic system can function adequately at low-factor concentrations but as the deficiency progresses, a point will reach when the procoagulatory mechanisms fail and bleeding occurs. Newborns have only 20–50% of adult coagulation activity. Lack of vitamin K administration at birth, exclusive breastfeeding, chronic diarrhea and prolonged use of antibiotics make them more prone to Vitamin K deficiency bleeding (VKDB) [1]. VKDB is a well-known entity and presents in 3 different clinical forms: early, classical and late. Classical VKDB develops mainly as gastrointestinal hemorrhage from day 2 to 7, and late VKDB develops as mainly intracranial hemorrhage from 2 weeks to 6 months. Compared with classical and late VKDB, early neonatal VKDB causes mainly internal hemorrhage within 24 h after birth along with a higher mortality rate compared to classical and late VKDB [3].
A 3-year-old girl first by birth order, born of a non-consanguineous marriage was noticed to have difficulty in balancing while walking and slurred speech since 2 years of age. The child started sitting at 12 months, months suggesting a motor developmental delay. On examination, she had staccato speech, hypotonia, dysmetria, and ataxic gait. Magnetic resonance imaging (MRI) brain revealed multiloculated fluid intensity cystic areas involving the superior cerebellar vermis and hippocampus with hemosiderin staining the wall of the cysts suggestive of a sequela of hemorrhage (Figure 1).
Her mother was diagnosed with pulmonary tuberculosis in the third trimester and was started on anti-tuberculosis treatment with Isoniazid, Rifampicin, and Ethambutol. Antenatal ultrasounds at 38 weeks gestation were normal with no intracranial pathology noted. The child was born full term by lower segment cesarean section, cried immediately after birth but developed seizures and required mechanical ventilation within 12 hrs of delivery. Investigations revealed prolonged prothrombin time (52s), partial thromboplastin time (60s) and INR of 4.2 which corrected to normal after injecting 1 mg intramuscular (IM) Vitamin K. Ultrasound of the brain performed on day 5 of life suggested a hypoechoic lesion with mild peripheral vascularity in the cerebellum measuring 1.5 cm in all dimensions. An MRI brain on day 5 confirmed midline hemorrhage involving the cerebellum and vermis measuring 2.1 × 1.6 × 1.2 cms in dimension (Figure 2). The child was treated with phenytoin and phenobarbital for seizure control.
Transplacental transfer of vitamin K is very limited during pregnancy, as is the storage of vitamin K in the neonatal liver, all of which makes the newborn infant uniquely vulnerable to hemorrhagic disorders unless exogenous vitamin K is given immediately after birth [2]. Classically, vitamin K deficiency bleeding is observed in infants who have not received prophylactic vitamin K at birth, with an incidence ranging from 0.25 to 1.7 cases per 100 births. Today, it is the standard of care around the world to provide vitamin K supplementation to the newborn with a single intramuscular dose (range, 0.5–1 mg) within 1 hour of birth. VKDB can be due to idiopathic cause or secondary causes. In secondary VKDB, there is an underlying cause, usually an undiagnosed disease such as hereditary hepatobiliary/ malabsorptive disease (e.g: - biliary atresia, alpha-1-antitrypsin deficiency, cystic fibrosis) or the effect of drugs that have been given to mother or infant. Bleeding commonly occurs in the umbilicus, gastrointestinal (GI) tract, skin, epistaxis, surgical sites (ie, circumcision) and, uncommonly, in the brain [4]. Early VKDB is almost always associated with maternal medications that interfere with vitamin K metabolism such as anticonvulsants (phenytoin, barbiturates, carbamazepine), antitubercular drugs (rifampin and isoniazid), antibiotics (cephalosporins) and vitamin K antagonists (warfarin and coumarin) [5]. The incidence of early VKDB in neonates of mothers taking these medications without vitamin K supplementation varies from 6% to 12% [5]. Although Intracranial Haemorrhage occurs most often in late VKDB (50-75%), it may occur in 20-25% of cases of early VKDB [6]. Common signs and symptoms in VKDB newborns with ICH are convulsions (80%), feeding intolerance and poor sucking (50%), irritability (40%) vomiting (47%) and fever (40%) [7]. The prognosis in patients with ICH due to VKDB depends on early diagnosis, rapid and adequate corrections of coagulation defect, and the general condition of the patient, including factors such as the presence of anemia and rapid surgical intervention [3]. Fresh frozen plasma (FFP) can be given to patients with normal hemoglobin level, with severe ICH as it contains all blood-clotting factors. Intravenous injection of vitamin k in the treatment of VKDB results in significant reversal of the hemostatic defect within minutes and its prompt use may obviate the need to administer plasma products [1]. In a study done by Zidan et al., despite early surgical evaluation, the mortality rate was high along with neurological complication. We present a unique case of a 3-year-old child who presented with seizures during the early neonatal period secondary to early VKDB in the cerebellum and later developed cerebellar ataxia and motor delay due to a remnant cyst formed in the superior cerebellar vermis. Infants predisposed to manifest early VKDB as evidenced by maternal intake of medications mentioned above should receive vitamin K, 1 mg IM at birth and they may be delivered by cesarean section to avoid the trauma of vaginal delivery [8,9].
RM, PD, SK, AP made substantial contributions to the design of the work by going through the history and physical of the patients along with the interpretation of past medical records. All the radiological interpretations were done by AC. The draft was prepared by PD, AP whereas RM, AC and SK revised it for important intellectual content. After approval from all the authors, the case report was ready for final submission.
The complete case report was prepared at the Department of Pediatrics, Nanavati super specialty hospital.
The authors have none to declare.