Feticide with Intracardiac Potassium Chloride to Reduce Risk of Hemorrhage in Medical Termination of Pregnancy
Objective: This is retrospective study to see the effect of feticide with intracardiac potassium chloride (KCL) to reduce the risk of hemorrhage in termination of pregnancy (TOP) with placenta previa, caesarian scar pregnancy and large fibroids distorting uterine anatomy.
Materials and Methods: Fetal cardiac asystole was achieved under ultrasound guidance using free hand technique, in eight patients who required termination of pregnancy because of multiple congenital malformations (4), history of intake of abortifacient drugs (1), premature rupture of membranes (1) with placenta previa, live caesarian scar pregnancy (1) and large fibroid in lower uterine segment (1).
Results: None of the patients has significant hemorrhage during termination of pregnancy and no blood transfusion was given. No maternal complication occurred with fetal intracardiac KCL.
Conclusion: Intracardiac KCL is safe to be used for feticide to reduce the risk of hemorrhage prior to TOP in placenta previa, caesarian scar pregnancy and large fibroids.
Keywords: Potassium Chloride; Pregnancy; Feticide; Fibroid; Scar Pregnancy; Hemorrhage
Medical termination of pregnancy in second trimester can lead to increased risk of hemorrhage in presence of various conditions like placenta previa which is the most common cause of obstetric hemorrhage [1]. Caesarian scar pregnancy is one of the rare ectopic pregnancies where implantation occurs at the caesarian scar. It can be life threatening because of risk of hemorrhage and risk of uterine rupture Significant hemorrhage and incomplete evacuation can also occur if uterine anatomy is grossly distorted by multiple fibroids or fibroids in cervix and lower uterine segment [2,3].
The technique of intracardiac KCL to induce fetal demise is well established [4]. KCL injected directly into the left ventricle induces asystole, and it is a safe and effective method of termination of pregnancy. Intracardiac KCL is frequently used for fetal reduction in multiple pregnancies. Its use to induce fetal demise to reduce hemorrhage in medical termination of pregnancy is not very frequent. Intracardiac KCL causes feticide and reduces the uteroplacental blood flow, thereby decreasing the rate of hemorrhage due to placenta previa, caesarian scar pregnancy and in cases of fibroids; it is easy to evacuate the macerated fetus. Only few case reports are available in the literature where it is used to reduce the risk of hemorrhage in placenta previa, scar pregnancy and fibroids where medical termination of pregnancy (TOP) is required for various reasons.
In this article, our first experience with the use of intracardiac KCL in such cases is aimed to present from a tertiary center.
This was a retrospective study of the women referred to a tertiary care hospital in North India from 2008 to 2016, who required medical termination of pregnancy but there was increased risk of associated hemorrhage either because of placenta previa or caesarian scar pregnancy or had large fibroid in lower uterine segment distorting the anatomy. These patients were referred to department of radiodiagnosis for intracardiac KCL to induce fetal demise to reduce risk of hemorrhage before termination of pregnancy. Written, informed consent was obtained from all these for intracardiac injection of KCL and legal termination of pregnancy. A detailed ultrasound examination was performed in order to note the fetal lie, presentation and placental site. The procedure of feticide was performed under all aseptic conditions under direct ultrasound guidance using a free-hand technique, without maternal sedation or anesthesia. Spinal needle of 20G was inserted into left ventricle of the fetal heart via transabdominal route. Needle position was confirmed by aspiration of fetal blood and strong KCL 15% (20mM/10ml) was injected using 2ml syringe in aliquots of 0.2ml till asystole was achieved. If asystole occurred during injection of KCL, further injection was stopped. Fetal heart was observed for 2minutes to assure permanent asystole. Doppler ultrasound mode was also used to ensure cardiac asystole. Repeat ultrasound was done after 30minutes to confirm fetal demise. Then the patients were observed in wards for spontaneous expulsion or termination of pregnancy was done.
The definition of cost in health care is not easily defined. There are many aspects of cost—from charges by facilities, reimbursement from insurance, and the actual cost of providing a specific service. The direct cost of ovarian cancer is largely unknown. As quality and cost are actively being scrutinized, we wanted to look at the direct detailed cost of care for a patient suffering from ovarian cancer. In order to achieve a finite study period, we evaluated the cost associated with the last 10 consecutive ovarian cancer patients who died from their disease. We examined every aspect of cost associated with their treatment from diagnosis to death. Our objective is to shed light on the components and drivers of costs for the treatment of ovarian cancer from the perspective of the hospital and physician.
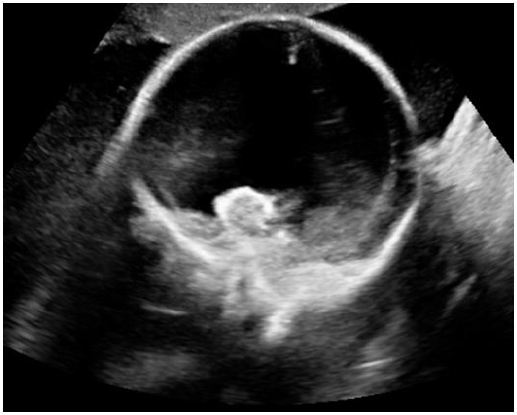
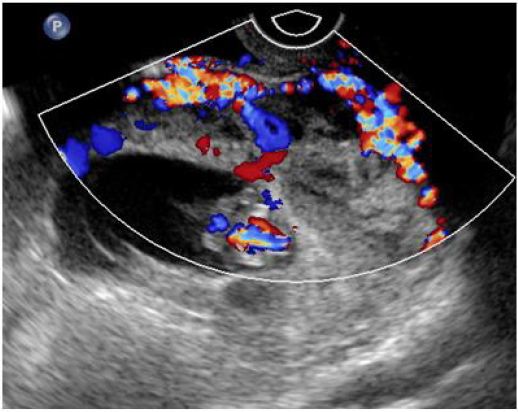
During this study eight women underwent fetal demise before medical TOP. Various indications for TOP were; severe fetal malformations (4), patient having taken abortifacient drugs (2), live caesarian scar pregnancy (1), premature rupture of membranes (1) (Figure 1A,Figure 1B). The indications for intracardiac KCL for fetal demise before TOP were; Placenta previa (6), large fibroid in lower uterine segment (1) and live scar pregnancy (1). Most common indication for medical TOP was severe fetal malformations (50%) and most common indication for intracardiac KCL was placenta previa (75%). Severe malformations were malformations that were not compatible with life; holoprosencephaly, renal agenesis, multiple abnormalities and anencephaly. Indications for TOP and KCL injection are listed in Table 1.
Median gestational age at the time of KCL injection was 18+2 weeks (range 10+4 weeks to 19 weeks). Average doze of intracardiac KCL into left ventricle to achieve asystole was 1.8ml with range of 0.5ml to 3ml. Complete asystole was achieved in all the patients within less than two minutes and Doppler ultrasound showed no color flow in umbilical cord and fetal heart. No patient requited insertion of needle second time. Entire procedure, from insertion of needle to withdrawal of needle, took less than 5 minutes. There was no maternal complication with fetal KCL injection.
Medical TOP was done after fetal demise in 4 patients, spontaneous expulsion of the macerated fetus occurred in 2 patients, suction evacuation was done in one patient of scar pregnancy, and in one patient with large fibroid hysterotomy with myomectomy for fibroid was done. None of the patients required blood transfusion.
The Intracardiac potassium chloride (KCL) was first described as a method for inducing fetal demise in 1988 and has since grown in use to induce feticide before an abortion, by either intracardiac or umbilical vein administration [5]. Fetal demise is induced before an abortion procedure for multiple reasons but it is most commonly used for fetal reduction in multiple gestations [6]. There are very few studies and case reports where fetal demise is induced with intracardiac KCL before medical TOP to reduce the risk of hemorrhage either because of placenta previa or ectopic pregnancy at scar site or due to large fibroids distorting the uterine anatomy [7-10]. We used intracardiac injection of KCL in left ventricle to induce fetal demise which was achieved in less than 2 minutes followed by termination of pregnancy. None of the patients required blood transfusion and none of the patients had any complication.
In our experience an average of 1.8cc of intracardiac KCL was required to achieve cardiac asystole which is less as compared to other studies. This is because the gestational age was less (10+4 weeks to 19 weeks) in our study as compared to a study by Sfakianaki et al. (range, 15.4-24.9 weeks) where on an average 10 mL of strong KCl was required to reliably achieve fetal cardiac asystole [11]. According to Bhide, et al. an average 10 ml of 15% KCL is required to achieve cardiac asystole effectively however 20 ml of strong KCL can be safely used by intracardiac route safely [12].
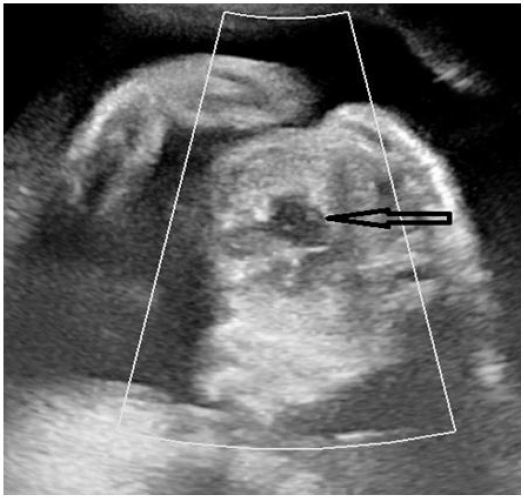
Placenta previa is one of the most important causes of obstetric hemorrhage. Its frequency in the second trimester is approximately 5% at 16 weeks [13]. Significant hemorrhage occurs during TOP when there is associated placenta previa [10]. Significant hemorrhage is when blood transfusion is required. Fetal asystole reduces uteroplacental blood flow thus the risk of hemorrhage. In our study 75% patient had placenta previa associated with complicated pregnancy out of which 50% patient had severe congenital malformations, one (25%) patient had history of intake of abortifacient drugs in first trimester and one (25%) patient had premature rupture of membranes before 19 weeks. Ruano, et al., reported significant number of hemorrhagic complications when termination of pregnancy was done without prior feticide in patients with placenta previa and rate of haemorrhage decreased significantly when feticide was done before termination of pregnancy [10] (Figure 2A,Figure 2B). In our study none of the patients required blood transfusion during termination of pregnancy because of induction fetal demise before TOP.
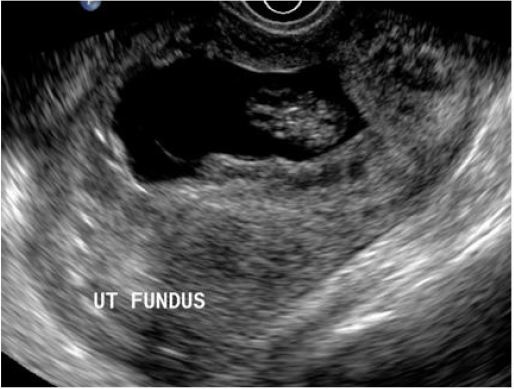
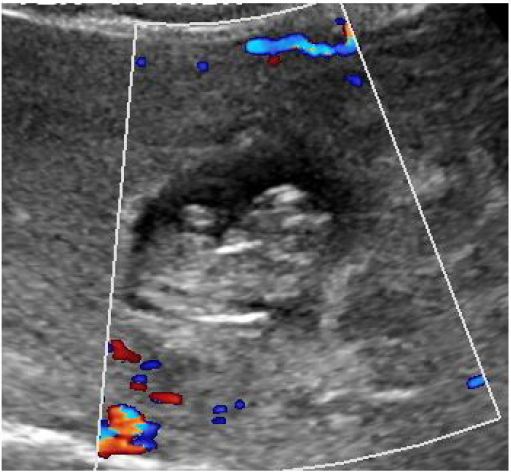
Cesarean scar pregnancy is a rare form of ectopic implanted in the myometrium at the site of a previous Cesarean section scar which is challenging to diagnose and have higher risk of bleeding and uterine rupture. It is life threatening condition [2]. Incidence of Cesarean scar pregnancy is 1:2216 of all pregnancies [14]. With limited experience of Cesarean scar pregnancies, it is difficult to decide on optimal management in individual cases [15]. The choice of management includes transvaginal surgical evacuation, laparoscopic removal, laparotomy, medical treatment with local injection of methotrexate or feticides [14,16]. We injected live scar pregnancy of 10+4 weeks with intracardiac KCL to reduce the blood flow and thus risk of hemorrhage. This was followed by transvaginal suction and evacuation in our patient without any significant hemorrhage (Figure 3A,Figure 3B). There are case reports where the live scar pregnancy was injected with KCL and methotrexate to reduce the blood flow before termination [9]. Uterine artery embolization has also been used in previous studies to manage scar pregnancy but uterine artery embolization is more invasive procedure than intracardiac KCL [17].
Large or multiple fibroids can distort the uterine anatomy and can complicate TOP especially if they are located in lower uterine segment or cervix [3]. Our patient 18weeks pregnant, had large 21x15x 19cm fibroid in lower uterine segment and termination of pregnancy was required because of intake of abortifacient drugs. Intracardiac KCL was used to induce fetal demise which was followed by hysterotomy with myomectomy for fibroid. No blood transfusion was required during surgery. There are few case reports where intracardiac KCL and intramuscular methotrexate were used to induce fetal demise before TOP in patients with large fibroid distorting the anatomy [8].
Various methods of feticide have been used in past like cardiac puncture and exsanguinations, air embolization, hysterotomy, fetoscopic cord ligation and tansection, intrafunic steel coil placement etc which are more invasive and no longer used. Injection of sclerotic agents have also been described in few case reports but are difficult techniques and not very effective. Various pharmacological agents like hypertonic saline and digoxin are also used. Hypertonic saline injection is accociated with disseminated intravascular coagulation. Intra-amniotic or intrafetal digoxin injection is used quite frequently [18].
This study was done on small number of patients which is the main limitation of this study. Larger studies are required to validate the use of intracardiac KCL to induce fetal demise before TOP in placenta previa, large fibroids and caesarian scar pregnancy.
In conclusion the feticide with intracardiac KCL is a safe procedure and reduces the risk of hemorrhage before TOP in placenta previa, scar pregnancy and large fibroids.