Gangrenous Sigmoid Volvulus in a Complicated Pregnancy: An Alarming Obstetric and Surgical Stigmata
Sigmoid volvulus in pregnancy is a rare presentation, since 1885, only 104 cases have been documented. Due to pregnancy, especially in last trimester, any clinical presentation of acute abdomen is easily masked by the growing fetus. Rather then, delayed diagnosis results in perforation and gangrenous SV which is disastrous to both, mother and unborn child. It presents with either typical or atypical symptoms. Furthermore, avoidance of radiological studies and sticking to obstetrics ultrasonography ultimately make such cases more complicated. In this case, a 24 years old, hepatitis C pregnant woman, who presented with the pre-eclampsia in early 3rd trimester is being documented in developing countries like Pakistan for the first time. Due to physiological changes in pregnancy, other clinical conditions and unique presentation of the patient, her intestinal obstruction was clouded. A little delay might have threatened the patient’s life but frequent gut decompression followed by surgery saved her. This study reports a case of atypical presentation of Sigmoid volvulus in 3rd trimester, 24 years old pregnant woman with satisfactory outcomes.
Keywords: Sigmoid Volvulus; Gangrenous; Complicated Pregnancy; Atypical Presentation
Sigmoid volvulus (SV) in pregnancy is a rare presentation, since 1885, only 104 cases have been documented [1,2]. Rather than, delayed diagnosis results in perforation and gangrenous SV which is disastrous to both, mother (25%) and unborn child (6%) [3,4].
Its incidence in pregnancy ranges from 1: 1500 to 1: 66,431 and reports for 25% to 44% of cases of intestinal obstruction [5,6]. Its predisposing causes include redundant sigmoid colon with the narrow attachment of mesocolon, long pelvic mesocolon, intra-abdominal adhesions from previous surgeries, chronic constipation and high residue diet [7,8]. Due to pregnancy, especially in last trimester, any clinical presentation of acute abdomen is easily masked by the growing fetus. Therefore, symptoms of abdominal distention, severe intermittent pain, obstipation with or without nausea and vomiting and signs like abdominal tenderness, sluggish or exaggerated bowel sounds with empty rectum on digital rectal examination must be evaluated for SV in pregnant women. Furthermore, avoidance of radiological studies and sticking to obstetrics ultrasonography ultimately make such cases more complicated.
Here, we report a rare case of young multiparous HCV positive pregnant women with gestational age of 32+1 weeks, presented with non-specific/vague clinical pictures of SV, which was obscured by her complicated pregnancy. This study describes some non-specific features of SV in complicated pregnancy and emphasizes upon the prompt diagnosis.
A 24 years old pregnant woman, gravida 3, para 2, alive 2 at 32+1weeks of gestation, presented to the outpatient department of gynecology and obstetrics, Ayub Teaching Hospital, Abbottabad with a one-day history of abdominal distention (gravid uterus), pain lower abdomen, low back and epigastrium associated with nausea. She was hospitalized for observation of labour and pain management.
Patient conceived spontaneously, confirmed pregnancy by urine pregnancy test. She did not follow antenatal care-clinic however, she carried a normal pregnancy. Other history was not significant. Patient medical and the surgical course were also normal.
On examination, she looked pale and lethargic, but she was hemodynamically stable, normoglycemic and afebrile. Her abdomen was distended up to epigastrium, mildly tense and tender with everted umbilical. She denied per-vaginal bleeding, discharge, constipation or diarrhea. All other systemic examination was unremarkable. Fetal status was reassuring with FHR 144/min. USG Obstetric confirmed pregnancy of 32 weeks’ fetus with cephalic presentation.
She was HCV positive, and her hemoglobin was 5.9g/dL (12-16g/dL), which was normalized after multiple transfusion, white blood count was 11300 (4000-11000/cmm), platelet count was 134000 (150000-450000/cmm). Her PT was 19 sec (14sec), aPTT was 38sec (35sec) and ALT/SGPT was raised, i.e. 55.2U/l (upto31 U/l). Renal profile and the electrolytes were normal. Exposure to radiation was avoided and the patient was put on conservative management, but next day her blood pressure started raising (180/110mmHg). Proteinuria +2 i.e. 100-300mg/dL, and RBC 10-20/HPF (0-5/HPF) was found on urine routine examination. She was tried for induction of labor for about 14 hours, but her condition was deteriorating, and the fetus was in distress too. She, then, underwent an uncomplicated emergency low transverse cesarean delivery for pre-eclampsia. Intra-operatively, a gravid uterus with a single alive female as cephalic was accessed. Both tubes and ovaries were normal, amniotic fluid was clear and adequate with mild to moderate ascites. Baby weighted 2.3kg with an immediate cry, ABGAR scored 8/10 and 10/10 at first and fifth minutes. She was shifted to neonatal intensive care for further evaluation, which was normal.
Postoperatively (POD), patient’s abdomen was still distended, and initial complaints persisted. Whereas, her bowel sounds were positive and was passing stools. On 2nd POD, she was consulted by surgeons of the same hospital and started with IV-fluids, antibiotics, analgesic, infusion paracetamol, glycerin suppositories. On 3rd POD, no improvement in patient condition was noted. Her abdominal distention became severe. The digital rectal examination was done and hard impacted stool was manually evacuated.
With nasogastric tube, 900ml-greenish colored gastric fluid was aspirated. Ascitic tap was negative. With nasogastric and flatus tube decompression, patient abdominal distention was reduced, and she was clinically improved.
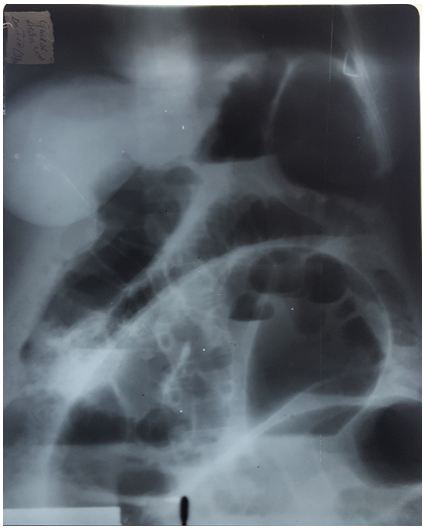
Next day, she followed some investigation. X-ray-erect abdomen showed large dilated gut with air-fluid levels, and omega sign (Figure 1). Mild to moderate free fluid in abdomen and pelvis with septations was found on ultrasound abdomen. Omega sign, dilated bowel loops (7cm), the fluid-filled lumen in lower abdomen and pelvis strongly suggested intestinal obstruction, i.e. sigmoid volvulus with peritonitis. Her serum urea begun to raise, 139mg/dL (12-25mg/dl), creatinine 10.6mg/dL (upto 1.2mg/dL) and WBC 20,000 (4000-11000/cmm). Her neutrophil % raised from 86.8% to 95.7%.
An emergency exploratory laparotomy with Hartman’s procedure was performed for the gangrenous gut, rectal stamp closure with silk 2/0. Per-operative findings were gangrenous SV with multiple perforations, lower 1/3rd of descending colon and upper 1/3rd of rectum were gangrenous and 1.5 liters of fecal tinged black foul smelling fluid was drained. Patient’s abdominal cavity was washed with 9-liter normal saline (0.9%Nacl) (Figure 2). Postoperatively, the patient was managed for deranged liver function and renal profile in the intensive surgical unit for two days. After significant improvement and workup of hepatitis C, she was discharged with home medications and frequent follow-up.
Gangrenous sigmoid volvulus in 24 years old, chronic hepatitis C pregnant woman, who presented with an atypical clinical picture and complicated pregnancy in earlier 3rd trimester is being documented in developing countries like Pakistan for the first time. Due to physiological changes in pregnancy, other clinical conditions and unique presentation of the patient, her intestinal obstruction was masked. Although, the baby was delivered, yet, a little more delay might have threatened the life of the mother.
The incidence of SV shows geographic variability. In western countries, its annual incidence is 1.7-5.7/100,000 adults, and in Asia, it is 24-60/100,00 with slight female predominance. Its mean age of presentation is the 7th decade [9-11].
It accounts for 25%-44% of all cases of intestinal obstruction during pregnancy and mostly occurred during 3rd trimester, but cases in early pregnancy and puerperium have also been reported [4,12,13]. In our case, it happened at 32+1 weeks of gestational age.
In recent studies, the overall mortality is 5%. It is mostly found in hospitalized, debilitated or obstipated, users of high fiber diet. SV is frequently associated with neuropsychiatric diseases, diabetes mellitus, and Chagas disease [2]. Our patient was physically active, neither-constipated nor other mentioned factors were reported.
During pregnancy, the enlarging uterus causes displacement, compression, and shifting of sigmoid and its mesentery and subsequent rotation of extra-pelvic segment over its fixation site of the mesentery, so that it becomes obstructed at some or other point of late pregnancy, forming volvulus [6].
The outcome of SV in pregnancy is deduced from the duration of symptoms, gestational age, parities and other co-morbid conditions. From 1985 to 2018, 31 cases have been reported with duration of symptoms (mean=53.45 hours-min=10 and max=150 hours), gestational age (mean=29.4weeks-min=16 and max=37 weeks) and 27 cases with 3rd trimester. At 24 hours’ duration of presentation, total seven cases (both mother and infant) survived. Similarly, mothers and new-born babies of five cases at 48 hours, three cases at 72 and one case at each, 28, 71, 120 and 150 hours remained healthy. However, the mean value of 52.26 hours represents a cutoff time for taking prompt action like surgery or even a GI decompression may be a savior. It’s obvious from this record that earlier the patient gets treated and/or operated, more chances of her and infant to be to alive [1,3-5,12-16].
Our case presented at 32+1 weeks and was operated for SV at the 7th day of admission i.e. total 192 ± hours of initial sign and symptoms. Instead of perforation and gangrenous gut, our patient survived.
Clinically, sigmoid volvulus is presented either as typical-with sudden onset abdominal pain, distention, obstipation and leukocytosis or as atypical- with vomiting, nausea, intolerance to oral intake and hypo or hyperkinetic bowel sounds. Some studies reported recurrent lower abdominal pain with insidious onset in younger patients [4,7,8,13,16]. Our case had a mixed picture of both, typical and atypical features, along with pain epigastrium and low back pain.
These non-specific signs and symptoms in pregnancy are due to the same visceral innervation of female reproductive organs and adnexa and that of the terminal ileum, sigmoid, colon, and rectum. Due to this, the spot diagnosis of SV in pregnant women is always clouded [17]. Likewise, in our case, along with superimposition of HELLP syndrome-like condition and pre-eclampsia, the growing uterus, and atypical presentation of patient concealed the diagnosis of SV. Therefore, she underwent two separate surgeries at different times. Kelsey E. Ward reported a similar case of 19 years old primigravida presented with labour pain [17].
Presentation of sigmoid volvulus with pre-eclampsia and HCV positive 3rd-trimester pregnant woman is not yet being documented therefore we cannot provide any literature over here. Regardless of surgical or laparoscopically intervention, Halabi WJ declared that the mortality of patient with SV is strongly associated with bowel gangrene, peritonitis, coagulopathy, chronic cardiac or pulmonary disease, ≥70 years old, and kidney disease as strong predictors of mortality. Luckily, despite, gangrenous sigmoid, and peritonitis, our patient, survived [10]. This might be due to younger age, a caesarian delivery or frequent gastrointestinal decompression.
Literature suggests the best prognosis for management of SV within 24 hours of initial complaints, but patients with gangrenous gut and perforation had a very poor prognosis. This statement is totally negated by our case [2,10]. The initial diagnostic modality is still considered the plain radiograph which is strongly avoided in early pregnancy. Whereas laboratory and clinical findings always conceal the actual disease in pregnancy, therefore, abdominal and pelvis ultrasonography or precisely speaking, an MRI must be considered immediately for such confusing clinical presentation [2,10,13,15,16].
Due to pregnancy, primarily, the diagnosis, and secondly the management of such acute cases are difficult to deal with. Serbi F, in full-term pregnancy, first treated an acute condition conservatively, and then performed postpartum surgery. If the injury is away from the gravid uterus, then it’s better to go with non-surgical management. Otherwise, appropriate surgical intervention for saving mother life is very important [18].
We propose a hypothesis that if a 3rd trimester young pregnant women present with acute history of nausea, vomiting of the biliary contents, pain epigastrium, lower abdomen plus low back, abdominal distention and leukocytosis, then she may have intestinal obstruction especially sigmoid volvulus. Moreover, if she developed peritonitis and does not undergoes repeated GI decompression, then she has a high risk of morbidity and mortality. Furthermore, to rule out SV, such patient must be the considered as priority candidate for detailed ultrasound abdomen and pelvis along with MRI.
Sigmoid volvulus is a high index of suspicion, an acute and alarming condition of intestinal obstruction with a wide range of clinical presentation, especially in pregnancy. Due to physiological changes during pregnancy, the same origin of visceral innervation, avoidance or limitation of investigative techniques and other co-morbid conditions make it difficult to diagnose a SV as early as one can. Ultimately, raising the risk of mortality and morbidity of the maternal and unborn child. In short, any pregnant 3rd-trimester woman ought to be considered as high suspicion for acute abdomen especially SV when she presents with nausea, vomiting, pain epigastrium, low abdomen with abdominal distention and leukocytosis. Furthermore, the classical triad of SV must be modified to include aforementioned picture with or without constipation and must not be confused due to gravid uterus.