Giant Liver Abscess Following Transarterial Chemoembolization
Liver abscess is a rare yet highly mortal complication of transarterial chemoembolization. We present a 69 years old man with hepatocellular carcinoma that developed a giant liver abscess after transarterial chemoembolization. Clinical improvement was successfully achieved after treatment with percutaneous drainage and antibiotics. This case highlights the importance of an initial broad differential diagnosis in order to a rise early suspicion and treatment of this condition with a particularly unspecific presentation. A literature review is presented as there are no standardized therapeutic protocols concerning the approach of giant liver abscesses.
Keywords: Liver abscess; Hepatocelullar Carcinoma; Transarterial Chemoembolization
Despite recent developments in diagnostic imaging, liver abscess remains a challenging diagnosis in need of high clinical suspicion due to nonspecific symptoms. It can be classified into 3 main etiologies: infectious, malignant and iatrogenic [1]. The incidence of hepatic abscesses as a complication of transarterial chemoembolization (TACE) is between 0 and 1.4% [1] with approximately 50% of mortality [2] as the diagnosis is often late, usually 2-90 days after the procedure [1].
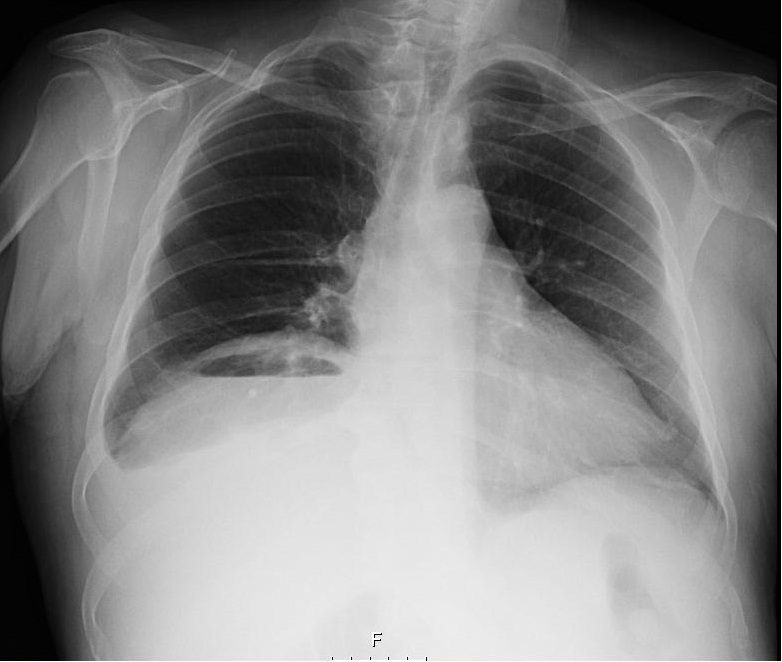
We present a 69 years old man admitted with a month history of fever and myalgia. Past medical history of type 2 diabetes mellitus, hypertension, chronic kidney disease in hemodialysis, hepatocellular carcinoma and non-cirrhotic liver due to alcohol abuse. Two months prior, the hepatic nodule in segment VII was treated by transarterial chemoembolization (TACE). On admission, he was obnubilated, blood pressure was 165/69 mmHg, 71 bpm, tympanic temperature of 38.3ºC and a normal abdominal examination. Laboratory evaluation revealed a hemoglobin level of 8.6 g/dL, white cell count 8500/L, C-reactive protein (CRP) 14.3 mg/dL, AST 42 U/L, ALT 47 U/L, GGT 302 U/L, ALP 259 U/L, total bilirubin 0.43 mg/dL, albumin 2.9 g/dL and INR 1.23. Chest X-ray disclosed air level under the right haemidiaphragm (Figure 1). CT scan showed a large intra-hepatic abscess (19x14.5x13 cm) in the right lobe with gas inside (Figure 2). Patient started meropenem and percutaneous drainage of the abscess was performed with 890 ml of purulent fluid drained. Blood and pus sample had negative cultures. After 4 weeks of antibiotics the patient showed full clinical and laboratory recovery. Follow-up CT revealed substantial improvement of the abscess, allowing for tube removal and patient discharge.
TACE is a minimal invasive procedure to treat inoperable malignancies and liver metastasis [1]. This procedure induces tumor necrosis but also in surrounding liver tissue, predisposing to abscess formation and decreased immunity [2]. Hepatic abscess complicating TACE can be challenging to diagnose given the subtle presentation and non-specific findings [2]. The incidence of hepatic abscesses as a complication of TACE is between 0 and 1.4% [2] with approximately 50% of mortality [3] as the diagnosis is often late, usually 2-90 days after the procedure [2]. The most common symptoms are fever and malaise. Although laboratory findings are also unspecific, almost all cases reveal altered hepatic enzymes and elevated CRP [4]. Some risk factors are known to increase mortality, such as male gender, malignancy, diabetes, sepsis and multi-organ failure, liver cirrhosis, liver abscess rupture and the presence of a large abscess (>5cm) [2]. Of note, our patient had almost all of these risk factors.
From all types of liver abscesses, solitary abscess evolving the right lobe are the most frequent ones. However, the presence of gas is only seen in about 17% of cases [2]. This feature could be identified as gas collection under the diaphragm in plain radiography [5]. The main differential diagnosis is with pneumoperitoneum and abscess formation.
Liver abscess treatment is far from being consensual, particularly in what concerns large (>5cm) and giant abscesses (>10 cm) [6]. Zhao-Qing Du., et al. suggested that the association of percutaneous drainage with antibiotic should be attempted in giant abscesses as it is related with a shorter hospital stay. Also it has the same curative ratio as surgical drainage with fewer complications, as illustrated in our case.
In conclusion, we present one of the rare etiologies that mimic pneumoperitoneum, where the presence of sub diaphragmatic air can lead to a challenging differential diagnosis. We emphasize the need for a timely diagnosis, in a disease that although rare has a high mortality, particularly due to unspecific clinical presentation.