Greater Trochanteric Pain Syndrome (Gtps) In Geriatric Patients: A Case Report
Greater trochanteric pain syndrome (GTPS) is related to abnormal hip biomechanics, predisposing to gluteal tendinopathies. Often concomitant osteo-articular conditions make the diagnosis difficult. GTPS occurs mainly in women, aged 40 to 60 years, but can also be seen in geriatric patients. We describe an 84-year-old, community-dwelling woman, hospitalised for exacerbation of low back pain, irradiating to the right hip, knee, and foot.
The diagnosis of GTPS was based upon a painful greater trochanteric region and painful adduction of the right hip, a positive single stance test, and ultrasound examination.
The patient was successfully treated by physical therapy, focusing on positioning and muscle strengthening, combined with pain relieve.
Keywords:Geriatric; Greater Trochanteric Pain Syndrome; GTPS
List of Abbreviations
BMI: Body Mass Index; FAC: Functional Ambulation Categories; FADDIR: Flexion Adduction Internal Rotation; GDS: Geriatric Depression Scale; GTPS: Greater Trochanteric Pain Syndrome; IM: Intramuscular; MMSE: Mini-Mental State Examination; MRI: Magnetic Resonance Imaging; NSAID: Non-steroidal anti-inflammatory drug; SPPB: Short Physical Performance Battery; ITB: Iliotibial Band
An 84-year-old, independent, community dwelling woman was referred to the emergency department for back pain that irradiated to her right hip, knee, and foot, increasing when moving her leg. As the pain responded insufficiently to oral Tramadol and Corticosteroids IM (type and dose unknown), she could not remain at home and was hospitalised on the geriatric ward. The pain had started in the right knee, three months earlier, without any trauma and had worsened since one week, mainly as low back pain, making any movement difficult. She was in good general health, but mentioned an ischemic cardiopathy (six years earlier she had received two coronary bypasses and four stents); there were no other remarkable problems in her medical history. She took polypharmacy: Spironolactone/Altizide 25 mg/15 mg/day; Acetylsalisylic acid 80 mg/day; Clopidogrel 75 mg/day; Mebeverine 135 mg 2/day; Bisoprolol 2,5 mg/day; Pantoprazole 40 mg/day; Lorazepam 1 mg/day; Rivaroxaban 20 mg/day; Simvastatine 20 mg/day.
Upon admission, a comprehensive geriatric assessment indicated a pre-frail status (Fried frailty criteria 2/5), with a Barthel index of 80/100, a Lawton score of 11/14, a FAC scale of 3, and a SPPB of 5/12. She had no major cognitive problems (MMSE-score 25/30), nor depression (GDS-scale 4/15).
Her BMI was 30 (76.5 kg; 1.60 m). Flexion and extension movements in standing position were negative for discogenic pain. The mobilisation of knees and hips was fluent, except for a painful adduction of the right hip. The FADDIR provocative manoeuvre was painful. The palpation of the right greater trochanteric region was painful, but there were no clear signs of inflammation. The single leg stance test (for 30 seconds) was positive, and the emergence of trochanteric pain during this period indicated tendinopathy of the medial M. Gluteus. The general examination revealed no other remarkable abnormalities.
Laboratory tests revealed a slight inflammation (CRP 14.6 mg/L; white blood cell count 7900/mm³), slight anaemia (hemoglobinemia 10.6 g/L), and a moderately decreased creatinine clearance (Cockcroft-Gault formula: 46 mL/min).
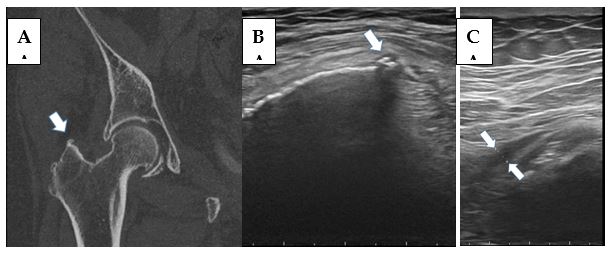
A CT-scan revealed degenerative lesions of the lower lumbar vertebrae, and enthesophytosis of the right greater trochanteric region (Figure 1, A). Ultrasound examination showed a tendinopathy of the M. gluteus medius tendon (Figure 1, B), and a fluid filled and thickened trochanteric bursa with evidence of inflammation (Figure 1, C), thus confirming the diagnosis of Greater Trochanteric Pain Syndrome (GTPS).
The initial pain treatment with paracetamol (1 g, 3 times a day) and Tramadol (50 mg, twice a day) was insufficient and had to be switched to Oxycodon (5 mg, every 4 hours). Finally, she was successfully treated with a single local infiltration of methylprednisolone/lidocaine (40/10 mg), physical therapy (focusing on positioning and strengthening of hip abduction), and Tramadol (50 mg, twice a day). The visual analogue pain scale improved from 8/10 to 1/10. She could be dismissed after five days, without any assistive device, but with referral for further physical therapy for additional exercising and instructions to decrease the load on the affected tendons and to avoid activities that may cause further tendon damage. Weight reduction was also strongly recommended.
GTPS is characterized by pain at, or around the greater trochanter. In most instances, GTPS is due to a M. gluteus medius or M. gluteus minimus tendinopathy, with variable involvement of the regional bursae [1]. The gluteus medius and minimus muscles are involved in abduction and exorotation of the leg, making GTPS an analogue to the rotator cuff tendinopathy of the shoulder. It is hypothesised that abnormal hip biomechanics predispose to the development of gluteal tendinopathies [2]. The aetiology proposed for the tendinopathy is multifactorial with both intrinsic and extrinsic components [1]. Intrinsic risk factors for GTPS include female gender (possibly related to the broader configuration of the pelvis) and obesity, both present in our patient; other intrinsic risk factors are spine (e.g. scoliosis) or limb abnormalities (e.g. difference in length, articular pathology); among the extrinsic risk factors are training errors, sedentary lifestyle, repetitive activities, and medication (e.g. oral corticosteroids, contraception) [1,3,4]. An overload tendinopathy can occur when hip abduction and pelvic stabilization are challenged, as during running, stair climbing, and standing on one leg.
GTPS is frequent and has a yearly incidence of 1.8 per 1000 patients [7]. In primary care setting, GTPS is a common cause of pain in the region of the hip and occurs in up to 45 % of patients complaining of low back pain [5]. GTPS is mainly seen between 40 and 60 years of age [2]. The general decrease of physical activities in older adults probably explains why GTPS becomes less frequent after the age of 60 years [6]. GTPS is a frequently overlooked diagnosis, as pain can be localized by the patient from the lower back to the hip and knee, and, as in the present case, even to the foot, thus mimicking ischiatic or radicular pain. In the differential diagnosis, acetabular labral tear, stress fractures, dislocation, contusion, avascular necrosis, and ligament strain can be mentioned.
GTPS is mainly a clinical diagnosis, based on history and physical examination, including the single leg stance test (standing for 30 seconds on the painful leg will provoke pain at the greater trochanter) [8]. Imaging of the spine and legs will exclude other pathologies [9]. MRI has a high sensitivity but a low specificity for diagnosing GTPS [1]. Ultrasound examination of the hip region will generally lead to the correct diagnosis [9].
The optimal management of GTPS remains unclear [2]. It has to be emphasized that GTPS is generally a self-limited condition [8,10,11]. The approach should focus on preventing disability, certainly in the geriatric patient, and on symptom relieve [12,13,14]. The physiotherapist has a major role, working with adapted exercise (isometric loading of the leg muscles) and activity modification (such as avoiding stair climbing). For pain relief NSAIDs can be used, if necessary supplemented with a local glucocorticoid injection. In our patient, we preferred to use opioid based pain treatment, as we feared complications of an NSAID treatment, since her renal function was reduced. Local glucocorticoid injection is generally well supported; it gives a rapid relieve that can last for several months. There are no clear guidelines for posology or frequency of administration. Recurrence is common and weakening of the tendon can be a long-term side effect [11]. The approach should also focus on associated comorbidities, like obesity, as in our patient [12,13,14].
A conservative approach will have a success rate of more than 90% [11]. On the other hand, after five years, at least 29% still will suffer from trochanteric pain [15]. The option for surgery is not well documented; it has to be reserved for GTPS failing to respond to conservative measures [10,11]. Endoscopic trochanteric bursectomy, iliotibial band or gluteal tendon repair can be considered as surgical interventions [7]. A review of the literature reveals no evidence-based protocol for the management of GTPS.
Although GTPS is most frequent from 40 to 60 years-of-age, it can also be seen in a geriatric population. The diagnosis is often overlooked as GTPS can mimic other conditions. Tenderness of the greater trochanteric region to palpation is the key physical finding. The optimal management of GTPS is based on pain relieve, physical therapy, and activity modification.
Author Contributions: All authors contributed to the assembly of the information, the preparation and the discussion of the manuscript. JG, SL and TM wrote the paper and IB, SR and TS revised it. All authors have read and agreed to the published version of the manuscript
Funding: We received no external funding
Informed Consent Statement: The patient gave her written informed consent
Acknowledgments: We thank Dieter Duhamel, physiotherapist at UZ Brussels, for his expertise.
Conflicts of Interest: The authors declare no conflict of interest.