Hemi-Abdominal Myoclonus: A Case Report
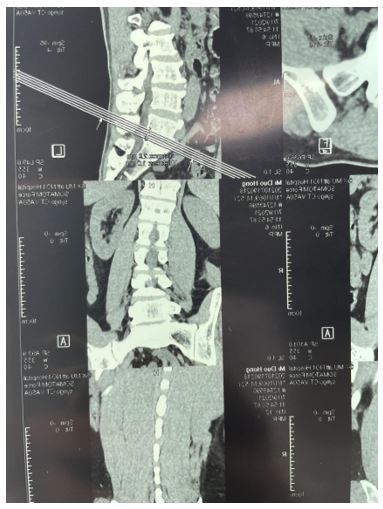
Spinal myoclonus is a kind of involuntary contraction of limbs or trunk muscles as the main performance, mainly divided into propriospinal myoclonus(PSM) and spinal segmental myoclonus(SSM). The pathogenesis of this movement disorder mainly includes spinal cord infection, trauma, spinal anesthesia, myelopathy, myelomyelination, syringomyelia, vitamin B12 deficiency and so on. A 52-year-old man was diagnosed with myoclonus myoclonus in hemiplinus of lumbar disc herniation accompanied by involuntary repetitive movements in the right side of the lumbar spine involving adjacent muscle groups. Lumbar CT revealed disc compression of the left L5/S1 nerve root. However, the involuntary movement of his lower back did not relieve after discectomy under general anesthesia. We report for the first time a case of spinal segmental myoclonus following lumbar disc herniation.
Keywords: Spinal Segmental Myoclonus; Abdominal Myoclonus; Video Electroencephalogram; Spinal Myoclonus
Myoclonus is a hyperkinetic movement disorder characterized by sudden, brief, involuntary jerks, and while most cases require symptomatic treatment, whenever possible, treating the underlying cause should be the primary goal[1]. Myoclonus is a sudden and transient convulsion caused by involuntary muscle activity, which can be divided into physiological, organic, epileptic and symptomatic[2]. Often, spinal myoclonus is caused by disorders of the spinal cord, such as tumors, infections, degenerative diseases, trauma, or spinal cord compression, including spinal and epidural anesthesia, but also spinal myoclonus[3]. Myoclonus can be divided into propriospinal myoclonus(PSM) and spinal segmental myoclonus(SSM).SSM is characterized by synchronous and unilateral convulsions involving local segments of the body, while PSM is defined as the presence of axial muscle flexion and extension convulsions involving the limb[4]. Segmental myoclonus is an involuntary, transient rhythmic contraction of a group of muscles provided by one or more consecutive segments in the brain stem or spine (spinal segmental myoclonus). [5]We present a case of myoclonus in which no structural lesion was found on magnetic resonance imaging (MRI), which supports the diagnosis of SSM.
We present a case of spinal cord myoclonus in which no structural lesion was found in magnetic resonance imaging (MRI) and review some possible pathophysiological mechanisms.
A 52-year-old man had a 9-month history of spontaneous involuntary repetitive movements of the right lumbar muscle. The campaign began in March 2021 as an occasional event.However, one year earlier, the patient presented with symptoms of low back pain accompanied by numbness in the left lower limb. In July 2021, the patient received lumbar disc surgery under general anesthesia. The operation went smoothly, and the patient had no side effects caused by anesthesia.After surgery, the numbness of the patient’s left lower limb was improved, but the involuntary movement of the right waist was not alleviated, and gradually worsened. According to him, this involuntary movement continued after he was awake and was with him for every second of his waking hours, and no gesture could relieve it.
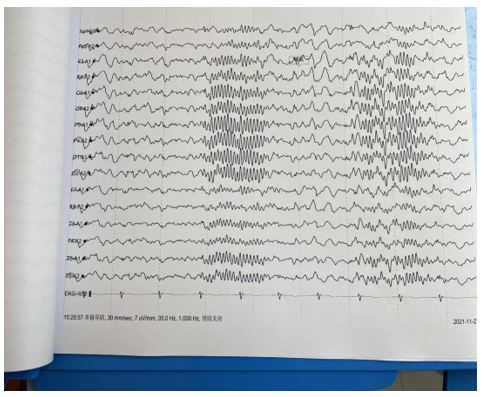
The patient had no family history of epilepsy or myoclonus, had not taken any known drugs that might induce myoclonus, and had no history of spinal cord injury or infection. Neurological examination suggested an asymmetrical lumbar spasm. Myoclonus is continuous, periodic, and irregular, and disappears completely after sleep. It is enhanced in supine position and attenuated in lateral position, without any prodrome, and is not dominated by consciousness, and persists at any time of the day. The characteristics and frequency of myoclonus were not affected by distraction movements and were not accompanied by other neurological symptoms. All laboratory tests were normal, including blood routine, C-reactive protein, erythrocyte sedimentation rate, D-2 aggregates, coagulation function, creatinine, transaminase, free triiodothyronine and free thyroxine, thyroid stimulating hormone, iron studies, and blood lipids; HIV, Treponema pallidum antibody, hepatitis B surface antigen; Anti-streptococcal hemolysin O, rheumatoid factor; Serum B12 and tumor markers. Cerebrospinal fluid biochemical examination, cerebrospinal fluid bacteriology examination and cerebrospinal fluid syphilis examination were not abnormal. Eeg was normal, and MRI of brain, cervical vertebra, thoracic vertebra and lumbar vertebra was not abnormal. Babinski reflexes not elicited, biceps brachii and triceps brachii reflexes of both upper limbs (++), meningeal reflex (++), and knee reflex (+++). Preoperative MRI showed no evidence of spinal cord compression. The patient refused to undergo EMG examination. Video EEG showed that 9-10 Hz, low and medium amplitude alpha waves were seen in bilateral occipital areas when awake and quiet with eyes closed, bilaterally symmetrical, alpha waves were adjusted, and adjustment and amplitude modulation were poor. Sleep: sleep wave: sleep waveforms in stages I, II, III and IV can be seen, and the amplitude of the sleep spindle is symmetrical on both sides. Attack period: During the video EEG detection, the patient has abdominal muscle spasm. During the whole attack process, the patient is conscious and can answer questions consciously,we did not conduct a further surface EMG recordings.When the abdominal muscle spasm occurs, no definite pathological wave is observed in the EEG during the same period, and the abdominal muscle spasm after falling asleep disappear.According to the patient’s symptoms and auxiliary examination, we diagnosed spinal segmental myoclonus, and gave clonazepam 0.5mg, once a day, baclofen tablet 10mg, once a day combined with physical therapy to significantly improve the movement disorder.
In this case, the clinical manifestations and electrophysiological characteristics of abnormal lumbar movement are consistent with the diagnosis of myoclonus, especially myoclonus in the spinal cord.The special feature of this case is that it occurred after the lumbar disc herniation, which completely involved half of the waist, and no significant relief was observed after surgery.The patient’s lumbar disc herniation initially manifested as pain in the lower back and gradually affected his daily life.Since the surgery was suspected to be related to a central nervous system injury, we reviewed MRI of the spine and found no significant changes. Normal spinal imaging rules out direct spinal cord injury during lumbar puncture.Myoclonus may also be caused by spinal anesthesia.[6] However, the patient underwent surgery under general anesthesia and her myoclonic symptoms did not progress. In conclusion, we propose that spinal segmental myoclonus is an exclusive diagnosis.
Degenerative spinal diseases such as disc herniation, spondylosis and spinal stenosis are not generally considered to have a causal relationship with movement disorders. However, in rare cases, patients with degenerative spinal cord disease secondary to nerve root or spinal cord compression may develop dyspraxia and may also develop degenerative disc disease following spinal surgery.Although the incidence of movement disorders associated with spinal surgery was determined to be 0.17%.[7]There have been previous cases of spinal myoclonus treated by disc decompression[8, 9],However, the correlation between spinal degeneration and dyskinesia is unclear.[7]Myoclonus, usually involving 1 or 2 adjacent spinal cord segments, has a specific resistance to supravertebral effects. In contrast, the propriospinal system is a slow-conducting intraspinal channel that connects multiple segmental levels, usually starting in the mid-thoracic segment and then traveling up and down to the spinal cord, causing recurring irregularities in the trunk, neck, hips, and knees Spastic flexion and extension clonus.[3, 4]It has also been suggested that SSM is caused by the loss of interneuronal inhibition in the spinal cord leading to the over excitation of anterior horn cells, which leads to the spontaneous repeated discharge of local segmental anterior horn cells.[10]
In our case, the patient did not have a specific responsible lesion, which involved the internal oblique and transverse abdominis muscles and spread to surrounding segments. Myoclonoclonus is rhythmic, occurs during awakening and disappears after sleep. Clonazepam treatment is effective, so segmental myoclonoclonus is the most likely diagnosis. PSM is related to the slow conduction of spinal cord main body pathway, and the spastic signal sent from the spinal cord central point to the relevant sarcomere is relatively delayed and the conduction is slow. PSM seems to be excluded due to the absence of aura sensation and the deterioration of wakefulness - sleep transition. Considering the muscles involved, we wanted further examination, but the patient refused to undergo an EMG of the paraspinal muscles, Therefore, we cannot define metameric levels in more detail.
At present, there is no exact diagnostic criteria for SSM in the world. In conclusion, we propose that myoclonus myoclonus is an exclusive diagnosis that can be based primarily on the patient’s clinical manifestations and auxiliary examination results. ①Clinical manifestations: sudden involuntary contraction of the innervated muscles of the affected segment of the spinal cord or/and its adjacent segments. ②EMG showed that the adjacent spinal cord segments’ dominant muscle groups emitted synchronous electrical activity. ③ MRI of spinal cord: if myelopathy is confirmed, SSM can be diagnosed. For the treatment of SSM, the currently known SSM treatment methods are drug therapy and physical therapy [10, 11]. The first-line drugs for treatment are clonazepam and diazepam; Second-line drugs include: valproic acid, levetiracetam, botox injection; And other drugs: bubenazine, sodium oxybutyrate. The above drugs are best combined with γ -tyrosine or glutamate and vitamin B6 use, can enhance the efficacy.In addition, physical therapy has achieved good results in spinal myoclonic spasm, which can be relieved by local massage. After one month of treatment with clonazepam, sodium valproate tablets, baclofen tablets, pregabalin, local acupuncture and massage, the patient’s symptoms of convulsion in the right side of the waist were significantly improved. We will follow up his recovery for a long time.

.JPG)
.JPG)
.JPG)
.JPG)