Impact of Covid-19 on Bronx, New York
The Covid-19 pandemic is still a rapidly evolving situation that continues to affect individuals domestically and internationally. Since the first reported case in Wuhan, China in late 2019, millions of people across the world have contracted and succumbed to the illness. Indeed, New York City and in particular the Bronx has been severely affected. While all people are at risk of infection and fatality, elderly individuals, immunocompromised, and patients with chronic medical conditions are particularly susceptible. Although vaccination efforts are clearly successful to mitigate the spread of the disease, the delta variant seems to infect even the vaccinated population. The economic, public health, and psyco-social effects of the Covid-19 pandemic to-date have been enormous. Here-in, we examine the up-to-date epidemiology, viral biology, pathophysiology, treatments, vaccinations, variants, and future directions of the concerning Covid-19 global pandemic.
Keywords: Covid-19; Bronx; Epidemiology; Immunizations; Pathophysiology; Vaccinations; Pfizer; Moderna; JNJ; WHO; FDA
The first report of a new viral illness, later identified as Covid-19, occurred in November/December 2019 in Wuhan, China. Soon, cases of acute illness, with pneumonia like symptoms (fever, cough, chest pain), were developing across China. Due to the global surprise, and lack of widespread governmental restrictions on travel, cases spread rapidly across Europe and later the USA. The WHO declared a global pandemic in March 2020, and thereafter cases rose exponentially around the world with death toll also increasing. As of October 11, 2021, there have been at least a reported 219 million cases and 4.5 million deaths world-wide due to Covid-19.
Due to the high transmissibility of the Covid-19 virus, certain precautions needs to be taken. Specifically, people in more highly populated areas were at increased risk of infection, due to limited social distancing and also concern for increased pollution and less hygenic areas. While this initially included cities in 3rd world countries, this later included lower-socio-economic areas in first-world countries, including Bronx, New York.
The first reported case of an illness originating from a seafood market was noted in Wuhan, China in November 2019. Soon, people across China started experiencing pneumonia like symptoms: fever, cough, chest pain. The deadly disease was causing mass casualties across China, and Chinese authorities struggled to handle their domestic situation rapidly and also failed to accurately warn neighboring countries. Limitations on testing in China, and later pressure to misrepresent cases and fatalities resulted in a lack of awareness and caution from the beginning of the pandemic.
The WHO declared this disease as a global pandemic in March 2020, and cases and fatalities rose exponentially. Scientists, doctors and government officials rushed to identify the causative agent and to develop treatments. Via sequence based analysis a novel coronavirus, which later termed as Covid-19, was identified. While initially believed to have originated from a human reservoir, it was later believed that transmission occurred from animals to humans, with the original host most likely a bat. Subsequently, news developed that the virus likely originated from a lab in Wuhan, China, specifically the Wuhan Institute of Virology, and it was notable that lab workers were among the first infected individuals with pneumonia like symptoms who were treated at local hospitals, before the outbreak was identified later in December 2019.
Due to the highly contagious nature of the virus, including direct and airborne transmissibility, and also transmissibility in asymptomatic patients, abundant precautions were necessary. This included protocols for frequent hand-washing, social distancing at least 6 feet apart, self-quarantine for 14 days for virus exposure, and travel restrictions. Some countries withstood initial high Covid-19 cases and death tolls, but then instituted strict lock-downs and restrictions on social gatherings, which severely curtailed the spread of the virus. From early 2020, domestically within the USA, the federal government did not take a proactive approach to dealing with the rapidly progressing Covid-19 pandemic, and cases rose exponentially across the country. Specifically, limitations in USA for lock-downs, social distancing, self-quarantine, resources for testing and treatment development, negatively impacted the country’s economy and health.
To date, after more than 22 months from the first identified case of Covid-19 in Wuhan, China, at least a reported 219 million cases and 4.5 million deaths world-wide have occurred due to Covid-19. Within the USA, at least a reported 44.3 million cases and 0.71 million deaths have occurred. Given the limited resources initially for Covid-19 testing and treatment, more people than documented likely were infected with the virus and succumbed to the illness.
While the modern world copes with the harsh new reality of a global pandemic, previous human experience with pandemics illustrates even deadlier portions of history.
Notably, in 1170 AD RSV killed roughly 240,000 children. In the 18th century influenza virus outbreaks killed roughly 1 million individuals. In the 20th century the Spanish flu killed an estimated 20-40 million people. In 1957, the Asian flu killed roughly 2 million people. The coronavirus has caused human infections since 1960s. Covid-19 is the 3rd major outbreak of respiratory disease in 20 years related to coronavirus.
Hence, while pandemics do occur, due to viral mutagenesis and biological changes, human and governmental preparedness and tracking are paramount to preventing and treating such acute changes.
Coronavirus is a ss (+) RNA 26-32 kb virus with components including a spike protein, membrane protein, E protein, nucleoprotein, and RNA. Different variants of coronavirus have slightly different structures, including variations of membrane proteins, the spike protein, and RNA genome. The cause of the current global pandemic, is due to the Covid-19 variant, which is deadlier than previous coronaviruses: SARS-CoV and MERS-CoV.
While Covid-19 is highly contagious, it is also highly infective, similar in infectivity to RSV and influenza A/B. Specifically, coronavirus can enter host cells via involvement of receptors on surface of host cell, and entry via pH and receptor-mediated endocytosis. The Covid-19 variant specifically uses the S glycoprotein to bind to the ACE2 receptors on the surface of host cells. Intense infection is primarily due to hyper-activation of T cells.
Pandemics typically arise when novel strains infect humans and promote human-to-human transmission before humans develop appreciable immunity to fight against these strains. Specifically, the influenza virus pandemic was due to a gradual antigenic drift of two distinct surface antigens: hemoagglutinin HA and neuraminidase NA. Swine Flu, a pandemic in 2009 was due to triple virus re-assortment.
Due to the high airborne transmissibility of the virus, acute respiratory tract infections are the most common disease for affected individuals. Due to direct viral entry into host cells via specific membrane proteins, multiples tissues types can be affected, including nervous system, vascular endothelium, and respiratory system. Within the nervous system, oligodendrocytes are the most likely to be affected. [1]
Upon presentation, patients will likely experience respiratory illness and may have fatigue, dyspnea, myalgia, headache, nausea, anorexia, dizziness, and confusion. [2] Some patients may also have sepsis, hyperpyrexia, hypoxia, hypercoagulability and critical illness.3 Additionally, other patients may experience neurological symptoms including stroke, anosmia, and peripheral weakness; in some patients, neurological symptoms could be the first manifestation of Covid-19. [3]
Modes of neurological infection include direct infection, which is rare, and para-infectious. One study found that in 214 patients with confirmed covid-19 infection, 36.4% experienced neurological manifestations. [1] During a pandemic neurological effects may be overlooked. [1]
Due to an overwhelming number of cases and deaths domestically and internationally, there was a strong drive to produce treatments as quickly as possible. Roughly [1] year after the first reported case of Covid-19 in Wuhan, China; vaccinations were available for domestic use Notably, [3] different vaccines were approved for emergency use authorization: Moderna, Pfizer, and Johnson and Johnson. Moderna and Pfizer are two shot vaccinations with nearly equivalent efficacy, while Johnson and Johnson is a single shot vaccine.
Upon the transition to the new federal government under President Biden; there was a stronger national emphasis on vaccinations. This included vaccines being rolled-out to many hospitals nationwide, and vaccinations clinics at many government and local centers. While at first there was a priority on vaccination of front-line medical workers and those with severe medical conditions; later there was a concerted effort to vaccinate as many people including children. As of October 13 2021; all individuals greater than 12 years of age may receive a Covid-19 vaccine.
While the risk of infection and possible hospitalization has been significantly reduced by administering vaccines domestically and sharing vaccines with other countries; there is new concern of variants. [4] Specifically, currently there is concern in regards to the delta variant, which includes risk of transmissibility, and reduced chance of effectiveness of vaccination or antibody treatments. Other variants being monitored include the alpha, beta, gamma variants, and Omnicron variants.
Based on presenting symptoms and clinical status, health-care providers have a wide-range of treatment options at their disposal. For patients who present to an outpatient setting and have concerning symptoms a nasal swab can be conducted and based on testing results can determine recommendations for conservative management, out-patient treatment, or inpatient management. For those patients who are asymptomatic but are in need for healthcare procedures including scheduled surgeries, colonoscopies, etc. then Covid-19 antigen testing can also be performed.
For patients who have been admitted to the hospital, initial patient management steps include documentation and assessment of clinical status, patient stabilizing measures including airway protection, oxygen as needed and maintaining hydration status. For patients who experience clinical worsening, additional medications including remdesivir are treatment options.
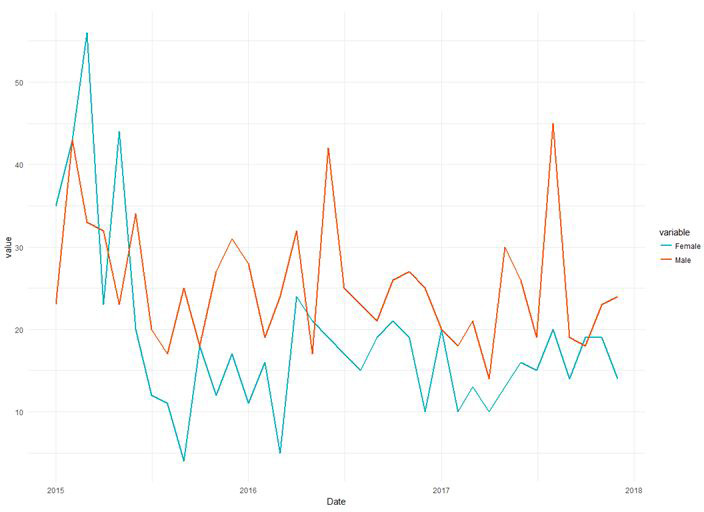
Covid-19 was first observed in the NYC population around mid-February 2020. The 1st confirmed lab case of Covid-19 in NYC was Feb. 29, 2020. The initial 3 months of the pandemic led to a rapid acceleration phase, also known as the 1st surge. In New York City, between February 29 – June 1, 2020 there were greater than 203,000 laboratory confirmed cases. Limited health-care capacity, including limited testing, social distancing, and public health precautions led to high rate of cases and fatalities. Indeed, initial wave in NYC mostly affected elderly individuals, males, those with underlying medical conditions, those residing in poorer neighborhoods, and those affected with racial and ethnic minority populations.
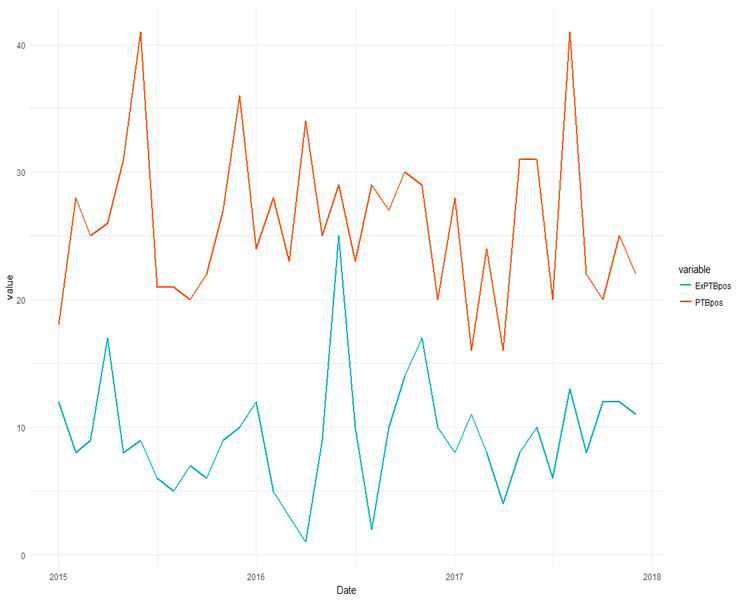
Specifically, within the Bronx, residents were affected by overcrowding, many essential workers, and high rates of chronic health conditions such as asthma and diabetes. Additionally, the Bronx had fewer hospital beds than other areas of NYC, including Manhattan. This has led to the increased diffusion of Covid-19 in the Bronx and greater NYC area. Specifically, the Bronx has had the highest death tool in all the boroughs of NYC, the Bronx has the lowest vaccination rate within NYC with only 36% of Bronx residents fully vaccinated as of June 2021.
To address this disparities, New York State offered subsidized healthcare enrollment between February – Nov. 2020. While as of January 26, 2021 vaccination rate against Covid-19 was 5% of New York City; it has now changed as of October 11, 2021 that fully vaccinated status includes 56.1% of adolescents aged 12-17; 73% of adults aged 18-64 years; 88.4% of adults aged 65 years or older.
It was estimated that due to Covid-19 pandemic NYC hospitals would experience 20-25 billion in losses with new expenses until April 2021. As of October 11, 2021 NYC accounts for 2.4% of US cases and 4.7% of US deaths.
As more health-care providers and the general population obtain vaccines, there is not only a reduced likelihood of individuals contracting the virus, but also increased chance of establishing herd immunity. As of October 11, 2021 a significant portion of the domestic USA population have already received full vaccination status; however, there are increased cases of delta-variant breakthrough infections. Currently, there is authorization for Covid-19 booster shots to treat immunocompromised individuals, patients who are elderly, and those with debilitating medications conditions. Evidence is currently being reviewed for the use of booster population for the general public.
Additionally, it will be important to maintain health-care precautions: frequent hand-washing, social distancing, mask wearing, and self-isolation with exposure. Future therapy also includes new medical treatments such as Pfizer’s Paxlovid.