Intra Parotid Facial Nerve Schwannoma in a 10-Year-Old Child: A Rare Finding
Schwannomas are slow-growing, benign neoplasms originating from schwann cells. Facial nerve schwannomas are rare, with a prevalence of 0.15-0.8% and they typically occur in the intra-temporal path of the facial nerve. Involvement of the extratemporal portion of the facial nerve is less common. These neoplasms can develop at any age, but peak in incidence between the 3rd and 6th decades. Intraparotid schwannomas in children is very rare and to the best of our knowledge, only four pediatric cases have been reported worldwide to date. We report a fifth case of a facial nerve schwannoma in a 10-year-old boy who underwent surgical excision of the mass with preservation of the facial nerve function.
Keywords: Intra Parotid Facial Nerve; Schwannoma; Child
Benign schwannomas are slow growing encapsulated tumor arising from the sheath of Schwann cell. They most commonly occur in the intratemporal part of the nerve [1]. Extra temporal facial nerve schwannomas are extremely rare, accounting for approximately 9-10% of all facial nerve schwannomas [2]. Intraparotid schwannomas in children are very rare and to the best of our knowledge, only four pediatric cases have been reported worldwide to date [3-6]. In this report, we presented a fifth case of pediatric intraparotid facial nerve schwannoma.
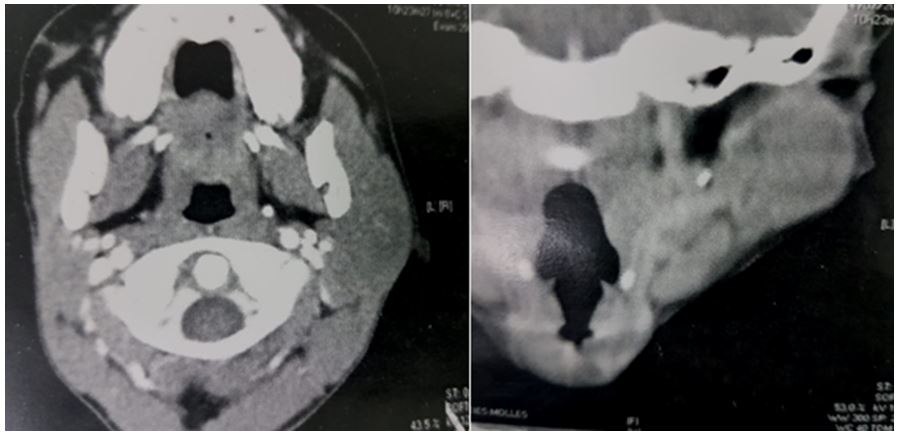
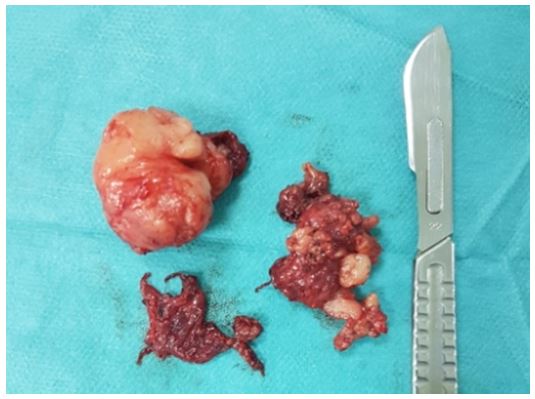
A 10-year-old boy with no medical, surgical or remarkable family histories, presented with a slow- growing, painless mass of three years evolution in the left parotidic region. Physical examination revealed a well-defined, approximately 3 cm/ 2 cm sized, smooth, mobile mass (Figure 1). Facial and other cranial nerve examinations revealed no abnormalities. Parotid ultrasound showed a 2.88/2.34 cm mass with a hypoechoic pattern, well-defined margins, and homogenous echogenicity with acoustic enhancement originating from the superficial parotid lobe (Figure 2). CT scan showed a well‑defined mass of the left parotid, lobulated, homogenous, with mild enhancement in the center and multiple small lymph nodes (Figure 3). Results of the routine blood investigations were normal. Total conservative parotidectomy was done. Modified Blair incision was made, skin flaps were raised and well encapsulated mass was visible. The trunk and main branches of the facial nerve were preserved. The mass was dissected and removed without difficulty, and was classified as type A, according to Marchioni et al., (Figure 4).
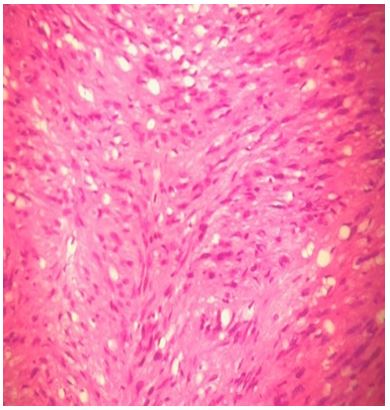
Histopathological examination confirmed the diagnosis of a benign schwannoma. Microscopically, the tumor consisted of palisading spindle cells with immunohistochemical expression of the S-100 (Figure 5). Facial nerve functions were normal after the operation and no recurrence was encountered within a ten month follow-up.
Schwannomas are slow-growing, benign neuroectodermal neoplasms originating from schwann cells. Such neoplasms can develop at any age, but peak in incidence between the 3rd and 6th decades [1]. Intraparotid schwannomas, are very rare in childhood, to the best of our knowledge, only four pediatric cases have been reported worldwide to date [3-6]. Table 1 shows the characteristics of those four reported pediatric cases.
The clinical manifestations of intra parotid facial nerve schwannomas are not specific. The most common clinical presentation is a slow-growing painless parotid mass mimicking pleomorphic adenoma. In four reported pediatric patients, the main clinical presentation is a painless parotid mass.
The radiological diagnosis of intra parotid facial nerve schwannoma is difficult. Marchioni et al. conclude that there are no definitive radiological features for intra-parotid facial nerve schwannoma [7].
Generally, a schwannoma appears as a yellow or pink encapsulated mass with distinct borders, which is in close association with the facial nerve [8].
Marchioniet al. suggested a classification of intra-parotid facial nerve schwannomas according to its position on the facial nerve. There are 4 types of intraparotid facial nerve schwannoma. Type a tumors can be removed without sacrificing the facial nerve. Type B tumors can be resected with partial sacrifice of the peripheral branches of facial nerve or their distal divisions. Type C tumors require sacrificing the main trunk of the facial nerve for their resection, while Type D tumors require sacrificing the trunk and its main divisions to be resected [9].
Management of an intra-parotid facial nerve schwannoma is challenging and still controversial, because diagnosis is made intra -operatively.
Ciufelli et al. proposed a decision-making algorithm based on pre-operative facial nerve function and intra-operative findings [9]. In the case of type A or B neoplasm, or in the case of a pre-operative facial nerve House–Brackmann (HB) grade IV or worse, the recommended treatment is tumor resection and reconstruction of the nerve defects if it’s necessary. In the case of preoperative HB grade III or better and type C or D tumors, patients would undergo intra-operative biopsy to rule out malignancy and Conservative treatment and follow-up could be adopted.
Histopathologic examination shows the presence of biphasic tissue architecture: hypercellular pattern with Verocay bodies (Antoni type A) or a hypocellular pattern with foam cells (Antoni type B). However, both patterns could be seen in a tumor at different regions [7]. Immunostaining for S-100 is required to establish the neural origin of the tumor, and smooth muscle actin (SMA) to rule out a leiomyoma [10]. The prognosis of schwannomas is excellent if surgical excision is complete.
Intra parotid facial nerve schwannomas in children are very rare and are mainly diagnosed postoperatively by histopathological examination. Facial nerve schwannoma should be considered in children with slowly growing mass in the parotid gland.
The authors have no conflicts of interest to disclose.