Introduction of an Improved Laparoscopic Dual Channel and Uncut Reconstruction Surgical Technique: A Series of Four Case Reports and Review of Literature
Background; In these recent years, the incidence of tumors in the gastric region have gradually heightened and are continuing to be of great challenge in the field of surgical oncology. Various methods of gastrointestinal reconstructions have improved the quality of life of patients gastric tumors to produce some significant outcomes. Especially, the dual-channel anastomosis and uncut surgical reconstruction has enhanced and some remarkable outcomes of postoperative measures as in the patient’s nutritional tolerance rate and anti-reflux. Furthermore, other effects have been solved by this new surgical technique.
Case presentations; These series of four case reports are mainly focusing on a newly introduced improved surgical technique the laparoscopic double channel and uncut anastomotic reconstruction of four male patients who underwent this surgical reconstruction in our health centre, surgical oncology department of Lanzhou second university hospital, Lanzhou, Gansu province, PR of China. This technique and surgical reconstructions were performed by an experienced surgeon. Considering these four cases was of great evidence as this technique proved to be of great benefit and some novelty associated with it in managing tumors and lesions in mostly the upper third or proximal portion of the stomach.
Conclusion: Owing to the fact that the duodenal pathway is preserved, thus this novel surgical reconstruction technique is associated with some advantages such as better anti-reflux effects and lower occurrence of dumping syndromes as well as better nutritional absorption.
Abbreviations: DTR- Double Tract Reconstruction; GC- Gastric Cancer; Nil- No Complications; QoL- Quality of Lif
Keywords:COVID-19; Purpura; Hypersensitivity Vasculitis
The incidence of gastric cancer mortalities has heightened. The morbidity of gastric cancer is higher in Southeast Asian than in European and American regions [1]. This includes China, which accounts for approximately 40% of patients with gastric cancer around the world, and this number is increasing. Patients who undergo any form of gastrectomy surgery have a lesser food intake ability, malabsorption, reflux esophagitis and abdominal distention just to point out a few. For those who have undergone proximal gastrectomy the same applies as compared to the one who has not undergone any form, be it distal or total gastrectomy. In these recent years, many surgical reconstruction techniques for managing gastric cancer have been incorporated and utilized. The question which still remains unanswered by experts and experienced surgeons is which one of these methods is best and which one will be the best in solving tumors and lesions of the stomach more effectively? There is no standard reconstruction method [2]. Some literature have reported double tract reconstruction (DTR) methods and uncut reconstruction separately [2, 3]. In our department we have therefore utilized both the dual passage and uncut reconstruction simultaneously and improved it which we believe is novel and was used in managing four cases with gastric tumors and lesions particularly on the upper third of the gastric region or had proximal gastric located tumors. This novel improved technique performed in four cases were tumors mostly located on the upper one third of the gastric region, which meant that laparoscopic proximal double channel and uncut reconstruction surgical method was performed and used in all our cases. Minimally-invasive surgery especially laparoscopic gastrectomy is gaining increasing popularity for the management of gastric cancer (GC) [4]. Many reconstructions surgical methods have been utilized for the management of gastric malignant tumors, as mentioned earlier.
Therefore, these series of case reports are elucidating an introduction an improved technique of both the double passage and uncut surgical reconstructions. As far as English literature has been reviewed and is concerned nothing has been reported as a case report and introduction of both the improved laparoscopic double passage and uncut reconstruction technique at the same time. In fact, what has been reported is double tract reconstructions, uncut Roux-en-Y and others separately. A published manuscript from Shen J et al. ,2020 entitled ‘Digestive tract reconstruction options after laparoscopic gastrectomy for gastric cancer’ clearly illustrates these surgical methods [5].
Nonetheless, in our current situation we are introducing this technique which was performed in four patients the improved laparoscopic double passage/channel and uncut surgical reconstruction as from two years ago. The terms double or dual passage or channels are used interchangeably. Uncut refers to surgically not resecting, ligation part of the stomach and bowels. This technique had some well noted clinical advantages in these four cases such as the reduction of the number of jejunum stumps and reduction of the risk of gastrointestinal leakages. The use of uncut further reduced the backflow of input radon. At several anastomotic sites there were also no or less bleeding.
Furthermore, this surgical reconstruction technique had a good anti-reflux effect and prevented the occurrence of dumping syndrome.
All these cases were performed by an experienced surgeon and expert from our health center. A detailed outline, brief summary of each of these four cases of gastric cancer and the reconstruction outcomes, discussions are covered in detail.
A forty-three-year-old male was admitted with history of gastrointestinal obstruction and pain sensation for more than 4 months around the upper abdominal region (i.e., gastric cardiac region). Had some difficulties in feeding and great loss of appetite.
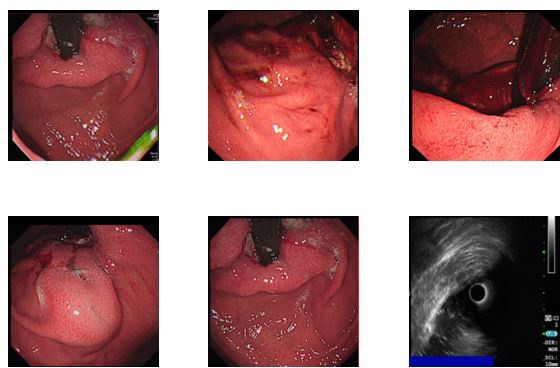
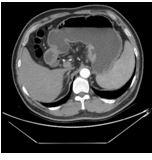
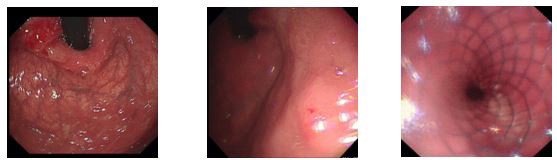
Physical Examination: stable vital signs, thoracic symmetry without deformity, bilateral tactile tremors were normal and symmetrical, and percussion double lung with good symmetry. On auscultation sounds were clear without wheezes; no dry and wet rales were heard. The heart rhythm was uniform, abnormal heart beats were not heard in the precardiac region. Tremors were felt in the stomach, the heart rate was 80 beats/min, percussion of the heart was normal, and no pathological murmur was heard in each valve area. The abdomen was soft, no rebound pain, muscle tension, abdominal wall without varicose veins, no abdominal gastrointestinal type and peristaltic waves, no hepatic and splenic masses, no abnormal masses, negative percussive mobile dullness, auscultation of bowel sounds normal, 3 times/min. There was no oedema on both lower extremities nor of the upper extremities. CT scan results from our health centre revealed; 1. No obvious abnormalities of the chest CT enhancement; 2. More considerations for gastric cardia cancer (T4N2). Ultrasound gastroscopy: gastric cancer Laparoscopic gastrectomy (Grade IV) was schedule to be performed, then finally after all investigations the chief surgeon and the team decided to perform dual channel and uncut surgical reconstruction. Postoperative pathological examination results suggested; (proximal stomach) of the cardia, poorly differentiated adenocarcinoma (Lauren type: mixed type). Figure 1a and b, shows an endoscopic, ultrasound and abdominal CT scan performed before the patient underwent surgery. The patient is now in a normal condition. He resumed normal diet and was discharged.
Cardiac malignancy, Hypertension and Adenocarcinoma were the final diagnoses and had to continue with some cycles of chemotherapy thereafter.
A 61-years old- male, was admitted due to “vomiting blood and passing of black stools for a week”. The medical history was as follows:
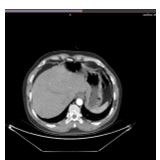
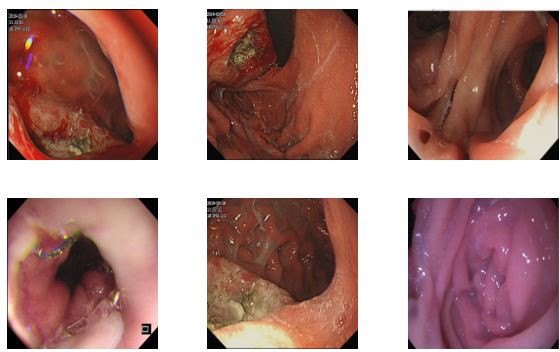
Had obvious induction of vomiting blood twice a week before admission. It was dark red, about 40ml, and had black stools for 1 week. There were tarry stools, which turned normal afterwards, with dizziness, fatigue, nausea, vomiting, and no headache, dizziness, chest tightness, no breathing difficulties, no sweating, fever, no chest pain and shoulder and back radiation pain, no cough, sputum, syncope and transient black jaw, no breathing pain and other discomforts. Furthermore, before admission to our health centre, he first went to Minle City People’s Hospital, blood haematological and chemistry results after admission; white blood cells 10.58*10^9/L red blood cells 5.7*10^12/L haemoglobin 189g/L biochemical: uric acid 486umol/L potassium 6.5mmol/L urea 19.8mmol/L. Plain chest radiograph: No signs of Chronic Obstructive Pulmonary disease (COPD). Gastroscopy tips; ulcer-like lesions of the body (to be examined for biopsy) chronic atrophic gastritis (mild sinus) and erosion. Medical Examination; low-grade intraepithelial neoplasia of “gastric body”. “Body of the stomach” chronic ulcers. Consultation in the pathology department of our health centre;(stomach mucosa) chronic inflammation of the mucosa, dysplasia in the interstitial glands, suspected to be cancerous tissues. There were no obvious abnormalities on the upper abdominal ultrasound. Prescribed symptomatic treatment such as acid suppression and fluid replacement (specific drug dose, unknown). Now the patient underwent further diagnostic evaluations and treatment, and then he was to be referred to our outpatient department, with a diagnosis of “Ulcerative gastric cancer”. Since the course of the disease, he had good cognitive functions, good sleep, normal bowel movements, and had lost 2 kilograms in the past month. 10 years of hypertension, 3 years of chronic enteritis, and 3 years of pulmonary heart disease. Further physical examinations for the patient were performed; Electronic gastroduodenal endoscopy, diagnostic opinion; Cardiac Ca Chronic atrophic gastritis (C2) with erosion. Endoscopic biopsy (a part of gastroscopy), diagnosis; unreported, diagnostic opinion; (cardia) moderate and poorly differentiated adenocarcinoma. Immunohistochemical staining; cancer cells showed Her-2 (3+), CKp (+), CK8/18 (+), CD56 (-), CgA (-), CD20 (-), Syn (-), Ki67 positive cell count was 40%.
Surgery was planned to be performed under general anaesthesia the following day. Patient’s relatives were informed of the surgery-related risks and complications, such as bleeding, anastomotic leakage, and infection. The patient and his family members expressed their knowledge and consented for surgery. Figures 2a and b, are showing some investigations performed for this patient.
Electronic gastroduodenal endoscopy, CT chest and abdomen, suggested diagnosis opinion: Cardiac Cancer with Chronic atrophic gastritis (C2) with an erosion. Endoscopic biopsy (a part of gastroscopy), diagnosis: unreported, diagnostic opinion: (cardia) moderate and poorly differentiated adenocarcinoma.
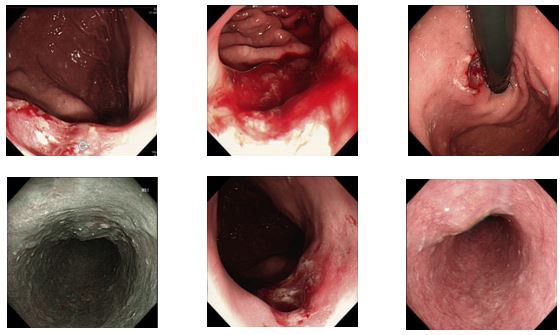
A 51 -year-old- male patient admitted to our health centre due to “upper abdominal pain and discomfort after food substance ingestion for more than 4 months and passing of black stools for 1 week”. Medical history was as follows; complained of pain and abdominal discomforts of the upper left quadrant after food consumption, no chills, high fever, no nausea, vomiting, no chest tightness, shortness of breath, no diarrhoea, loose stools, no dizziness, headache and other discomforts, no attention, no special diagnosis and treatment, appeared 1 week before admission blackish stools, no hematemesis, no cough, sputum, no haemoptysis and other marked discomforts, in order to seek further treatment, in our health centre, underwent electronic gastroscopy which showed; some ulcerative lesions of the gastric cardia (considered Cancer), chronic atrophic gastritis ( Sinus mild), pathological biopsy results were yet ready at the time, and the outpatient clinic accepted it as a “gastric ulcer”. During the course of the disease, the patient was well oriented and had good mental status, able to eat and sleep, black stools, and urinate as normally without abnormalities detected. There was no significant recent weight gain or loss. Previous physical fitness, denying history of chronic diseases such as hypertension and diabetes, denying history of trauma and surgery, denying history of food and drug allergies.
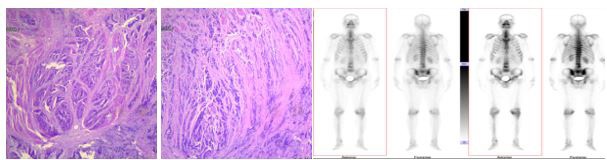
Electronic gastroscopy in our health centre showed: ulcerative lesions of the gastric cardia (considering Cancer) and chronic atrophic gastritis (mild sinus). Chief surgeons and team members after doing ward rounds discovered that post admission, the patient’s condition significantly improved as relevant examinations confirmed a diagnosis of gastric malignant tumour. However, the patient was scheduled and had to undergo surgery. An explanation to the patient’s relatives that the patient may have other unpredictable risks such as gastrointestinal bleeding, perforation, infection, intestinal fistula, incisional hernia, deep vein thrombosis, pulmonary embolism and other related surgical complications was done. During the perioperative period, the family members were informed about the new improved surgical technique to be done, understood and agreed to consent for surgical treatment. (Figure 3. a, b and c) also shows some Computer Tomography (CT) scan chest and abdominal, endoscopic examination, some pathological results and Positron Emission Tomography (PET) examinations for the patient.
A 57 -year old- male patient was admitted to the health centre due to “an upper abdominal pain for more than 5 months”.
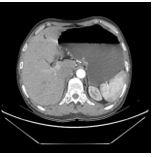
Examination results; no yellow pigmentation of the skin and mucous membranes and sclera of the whole body, flat abdomen, no intestinal abnormalities and peristaltic waves active, no abdominal varicose veins, normal spleen, full abdomen without masses, upper abdomen with mild tenderness, no rebound pain and muscle tension, Murphy’s sign negative, bowel sounds normal. There was no oedema in both lower extremities. Gastroscopic investigations; gastric bulge(inflammation). Biopsy results; revealed an adenocarcinoma. CT; 1. calcification of the left upper lobe. 2. The right thyroid lobe lesions, benign lesions were considered, combined with an ultrasonographic examination. 3. The stomach wall thickened on the sides of the small curvature of the stomach, and the surrounding lymph nodes increased. Considered gastric Cancer (preliminary evaluation of T2N1M0). 4. Liver VI Segment hamartoma; calcium deposition in both kidneys, left kidney cyst.
Dual passage and uncut reconstruction surgery were the one to be performed. Postoperative pathological examination report; (cardia) neuroendocrine carcinoma (NECG3), the tumour size measured 4×3.5×1cm, cancer tissue invaded the full thickness of the stomach wall, and there was no definite abnormalities of the nerves and vessels; there was no cancer in the upper and lower margins.
Group 6 lymph nodes (0/2), large curved lymph nodes (0/4), small curved lymph nodes (0/2), group 1 lymph nodes (0/0), group 2 lymph nodes (0/0), Group 3 lymph nodes (0/3), Group 4 lymph nodes (0/2), Group 5 lymph nodes (0/0), Group 7 lymph nodes (0/6), Group 11 lymph nodes (0/0), Lymph nodes in group 11b (0/0) and lymph nodes in group 13 (0/0) showed no cancer metastasis.
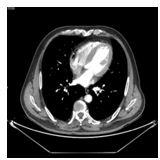
Immunohistochemical staining: cancer cells showed CKP (+), CK8/18 (+), Syn (+), LMP-1 (-), C-erbB-2 (0), PMS-2 (-), MLH- 1 (+), MSH-6 (+), MSH-2 (+), the number of Ki-67 positive cells were 65%. The patient’s general condition had improved. He resumed his normal dietary intake and was discharged. Some of the investigations which were performed on this patient are shown, abdominal and chest CT, endoscopic examinations with some metal stents figures 4a and b.
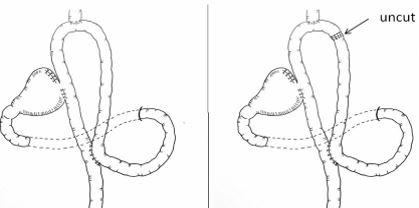
Four cases underwent this new improved surgical technique. The whole operative procedure on average takes three to four hours. The upper one third of the stomach (proximal) is surgically removed depending on the exact location of the tumour and some anastomotic techniques are ultimately preformed. For our cases mostly the tumors and lesions were located along the gastric cardia some along the gastric body from the stomach fundus and others on the lesser curvature. However, all the operations performed were laparoscopic one third proximal gastrectomy with some anastomoses, construction of some double or dual passages and uncut, are illustrated in figure 5. The uncut depicts that no surgical cutting was done only anastomoses of the remnant distal stomach, portion of the oesophagus, duodenum and jejunum were anastomosed. Figure 6, is a straight-cut closure which closes the jejunum-jejunum common opening to a dual channel.
Post aesthetic medication administration and patient assuming supine position, preparation of the skin on the abdominal surgical site and draping is done, first, 10 mm incision by two centimetres incisions are made below the umbilicus. Placing a 10 mm Trocar, and using a camera to detect some intra-abdominal lesions and tumors. Switching to fluorescence laparoscopic mode, to see the fluorescent staining of the stomach wall of the small curve side, the upper border of the staining of about 10cm from the cardia, and the lower border of about 20cm from the pylorus is also carried out. Then checking and verification of the lymph nodes in the abdominal cavity, common hepatic artery, splenic artery, and abdominal aorta enlargement is also done. When laparoscopic exploration is performed, that is when the double passage and uncut surgical reconstruction is done. Cutting of the gastrocolic ligament at the upper edge of the transverse colon, separation of the anterior lobe of the transverse colon, separation of the upward to the lower edge of the pancreas, separation of the pancreatic capsule to the upper edge of the pancreas, excision of the left side of the omentum to the flexure of the colon, and clearing of the lymph nodes of the large curved side of the stomach , reaching the splenic hilar to the left, and dissection of the splenic hilar lymph nodes are all performed during surgery. Cutting off the left gastro perivascular vessels and short gastric veins, and the continuation to the dissipation to the bottom of the stomach, keeping the right gastric arteriovenous veins in the pancreaticoduodenal arteriovenous veins, and removal of the small curved side lymph nodes three is also achieved during the process. The left gastric artery and the left gastric vein are then cut and ligated, respectively, and the lymph nodes and fatty tissues at the root of the left gastric artery are removed. The irrigation of the lymph nodes of the cardia is also done at this stage. The stomach is cut with a laparoscopic incision cutter 5 cm from the lower edge of the tumors.
Continuation of the dissipation to the cardia near the small curved side, finding of the flexor ligament and the beginning of the jejunum, cutting of the jejunum with a linear incision with the utilization of the laparoscopic jejunum at 30 cm from the flexor ligament, and lifting the distal end 3 cm below the oesophageal dentate line using a 3-0 absorbable suture and the construction an oesophageal jejunum anastomosis, cutting the stomach 3cm at the upper edge of the local tumour with a linear cutter, and performing a residual gastric jejunostomy at 25cm below the local oesophageal jejunostomy opening, local residual gastric jejunostomy is done. Anastomosis of the proximal jejunum to the distal side of the jejunum was performed at a 15 cm anatomical point and a double channel is once more re-established, each anastomosis is examined, and the anastomosis is reinforced with a 3-0 barbed suture. Uncut closure is performed at an input loop about 10 cm from the oesophageal jejunum anastomosis. A small incision is made to remove the proximal part of the stomach and the proximal part of the omentum and local lymph nodes. Checking that there is no active bleeding in the operative field is also crucial.
Parameters and findings for each case were recorded before, during and after surgery summarized in table 1.
Surgery remains the only mainstay of treatment for curative gastric cancer, while perioperative and adjuvant chemotherapy, as well as chemoradiation, can improve outcomes of resect able gastric cancer with extended lymph node dissection. More than half of radically resected gastric cancer patients relapse locally or with distant metastases, or receive the diagnosis of gastric cancer when a tumour is disseminated; therefore, median survival rarely exceeds 12 months, and 5-years survival is less than 10% [6]. For our cases we have introduced and improved the double passage and uncut reconstruction which were both utilized simultaneously. Nevertheless, some literature reports uncut separately of the Roux-en-Y surgical technique. Moreover, a method of the digestive tract reconstruction called “Roux-en-Y anastomosis” was first proposed in 1988. It has been a research hotspot for years since then [3]. Furthermore, some literature only states the double tract reconstruction as a single entity without the uncut in which the double tract reconstruction is just another term for dual channel or double passage as used in our own work. Nonetheless, proximal gastrectomy was mainly performed in patients with early GC in the upper-third of the stomach to preserve the physiological function of the remnant stomach [7, 8]. Many reconstructive procedures have been reported, including esophagogastrostomy, jejunal interposition [9], jejunal pouch interposition [67], and Double Tract Reconstruction (DTR) [10, 11]. In addition, according to our knowledge after thorough literature search and review no single case report has been published or reported introducing an improved laparoscopic double channel and uncut reconstruction surgical method both performed at the same time intraoperatively. Either one of them that is double channel or uncut has been published separately as literature reviews or research work. Therefore, we have introduced this surgical reconstruction method the improved dual channel and uncut at the simultaneously. Post this surgical procedure we also found out that similar to other previous studies of either laparoscopic double gastrectomy alone and uncut reconstruction surgical methods, we had similar merits and advantages as compared to those of other authors. For instance, these surgical laparoscopic gastrectomy reconstructions either double passage reconstruction or uncut after patients having undergone either surgery; Reflux esophagitis can be theoretically reduced due to the interposition of the 10- to 15-cm jejunum between the remnant stomach and oesophagus [12]. On the contrary, other studies have reported that DTR has advantages in haemoglobin change and vitamin B12 deficiency compared with laparoscopic total gastrectomy [13-15], which also concurs with our own surgical laparoscopic double channel and uncut procedure’s findings.
Having performed surgery with regards to our improved new laparoscopic dual channel and uncut reconstruction its advantages observed and noted from patients were; a reduction in a number of jejunum stumps and a reduced risk of gastrointestinal leakage. The use of uncut further reduced the backflow of input radon. The double passage and uncut reconstruction technique have a good anti-reflux effect and prevents the occurrence of dumping syndrome. Furthermore, the duodenal pathway is preserved, which is helpful for the recovery of neuro-endocrine function of the digestive tract. In addition, continuity of the anatomic structure of the gastro-duodenum is reserved for the patient for future endoscopic treatment of biliary tract complications if they develop.
There are significant and remarkable advantages in improving patients’ vitamin B12 and haemoglobin levels.
In conclusion, our improved laparoscopic reconstruction double passage and uncut has proved to be of great benefit for these four-cases as they almost presented with similar characteristics post-operatively. Furthermore, patient’s quality of life (QoL) as in nutritional status is improved, has some good anti-reflux effects and some reduced risk of gastrointestinal leakages.
This surgical technique is still to be carried out on more patients to even further verify its efficacy in the future. It should be however made mention that our study has some limitations, for instance our cases were only for but remarkable outcomes were obtained in these subjects. Furthermore, the efficacy of our technique would be more fascinating had we also utilized robotic surgery.
Not applicable.
Written informed consent for publication of their clinical details and/or clinical images was obtained from patients
Data sharing is not applicable for this article as no datasets were generated or analysed during the case reports.
The authors declare that they have no competing interests
EPM is the first author of this manuscript and Professor HC is the corresponding author. ZM, ZDF, HYL, BM, YY, JZD and JYZ assisted with patients’ medical histories, clinical investigations, performance of surgeries, data analysis and arrangement of examination reports as well as figure arrangement. All authors read and approved the final manuscript.
We would like to send our heartfelt gratitude for support provided by the Lanzhou University Second Hospital Surgical oncology, department, team and staff members.