Multidetector computed tomography in cases with emergency chest trauma
Chest traumas are a significant cause of mortality and morbidity. They commonly occur in the younger population and are the most common cause of death in people between 25 and 40 years of age. This article summarizes the place of MDCT in the diagnosis, examination technique and findings in injuries of the chest trauma patients.
Methods: Multidetector computed tomography (MDCT) is considered to be the most effective imaging method in this field. Its advantages include especially high speed and high geometric resolution at any plane. The method allows us to view large parts of the body with minimal motion artifacts and to create accurate multiplanar and three-dimensional (3D) reformations.
Results: MDCT allows us to view diagnosis significantly more accurate. One hundred and twelve patients are examined at the Emergency department. The injuries of the chest and intrathoracic organs are found. In 56 (50%) of all 112 patients in- cluded in our study, fractures of the ribs are the most common traumas. Also fracture of the scapula, sternum, extra pleural hematomas, pneumothorax, hemothorax, pulmonary contusions, laceration of trachea and bronchi, rupture of esophagus, diaphragmatic rupture and injuries of blood vessels are established
Conclusion: Because of its advantages MDCT has become the first-choice method in emergency chest trauma patients.
Keywords:Multidetector computed tomography, Blunt trauma, Penetrating trauma
In recent years has been observed major chest injuries withch represent a significant socioeconomic problem. They commonly occur in the younger population and are the most common cause of death in people between 25 and 40 years of age. Chest injuries occur in about 20 % of all trauma patients. In up to 80 % of cases they are associated with injuries of other body parts such as the head (69%), abdomen and pelvis (43%) and extremities’(52%) [1, 2]. Diagnostic imaging plays a key role in deciding the thera- peutic procedure’s [3]. Multidetector computed tomography (MDCT) considered to be the most effective imaging method in this field and therefore should be a part of the emergency department [4]. We trying to evaluate the place of MDCT in the diagnostic algorithm in major trauma patients.
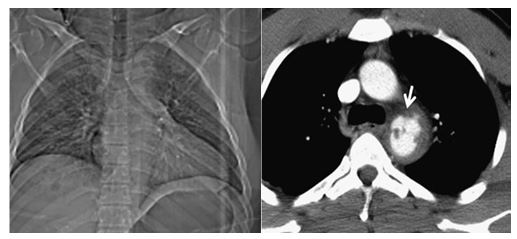
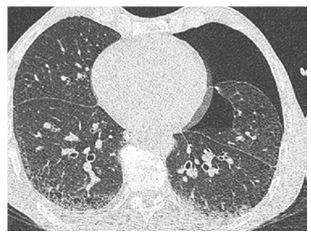
Clinical symptoms of chest trauma are diverse and often do not correlate with their severity. This is the reason why diagnostic imaging are the first procedures performed after admission to a emergency department. The simplest and fastest methods in- clude chest radiography and ultrasound. They can provide important information about the presence of serious injuries requiring an emergency intervention, such as tension pneumothorax, large hemothorax, hemoperitoneum and injuries of the abdominal organs. It is also very unreliable in detecting injuries of the heart and great vessels [5–8]. Compared to this, MDCT enables suffi- ciently accurate assessment of all compartments of the chest also reveals changes that are not detectable by other methods (Fig. 1).
Excellent spatial and temporal resolution is the main benefit. Because of the isotropic data field, it allows performing two-dimensional (2D) and three dimensional (3D) reformations in any plane and angle of view without loss of geometric resolution.
The choice of a diagnostic procedure depends on the patient’s condition and traumatic mechanism. In stable patients with no need of emergency intervention, the MDCT examination can be performed directly after admission to the emergency department and primary clinical examination. In the case of circulatory instability, the chest X-ray in supine position is usually performed as well as ultrasound examination to exclude findings that require an immediate intervention. If MDCT is a part of the emergency department it can be used as the primary imaging method
To minimize motion artifacts high examination speed should be used in traumas, and because of the need to perform reformations in other planes the highest resolution in the Z-axis should be used as well. Dose reduction is achieved the kilovolt value can be reduced to 80–100, and the mAs value can be decreased to 30–80 (Fig. 2) [6].
Application of contrast media is essential for the assessment of vascular structures and parenchymal organs and for detection of active bleeding. Therefore, we used a longer scanning delay (30–40 s.) compared with standard chest examinations. A mall amount of contrast material we used in case of suspected rupture of the esophagus. In this case water-soluble iodinated contrast medium (usually 5–10 % solution) was used. The slices reconstructed in three principal planes (axial, coronal and sagittal). We used thinner slices (1– 1.5 mm) reconstructed using a high-resolution kernel.
Chest wall injuries are very common. Fractures reflect the intensity and direction of forces during trauma. However, the extent of a chest wall injury does not have to correlate with the injuries of the intrathoracic organs. This is evident especially in children and young adults with a flexible skeleton in whom severe visceral traumas may occur despite there being no fractures.
The total number and percentages are not equal to the total number of patients because one patient has several types of injuries.
The PD catheter was implanted surgically, paramedian, subumbilical under general anesthesia.
In 56 (50%) of all 112 patients included in our study, fractures of the ribs are the most common chest wall traumas. They in fact are usually not clinically significant. MDCT determine the number of fractures, their location and degree of dislocation more accurately than X-rays. Contrary to X-rays, it is also able to detect fractures of the rib cartilages [3, 5]..
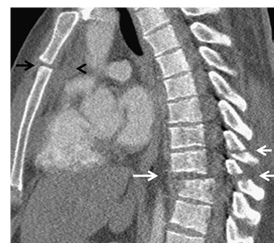
In eleven (9.82%) of the cases a fracture of the scapula was established. . It is usually caused by strong direct impact or the large axial forces. In up to 40 % of cases, it is associated with pulmonary contusion, pneumothorax or hemothorax [10,11]. The areas of the scapular body and neck are mostly affected (Figure: 3).
Sternal fractures occur in 9 (8.03%) of cases. They are usually caused by direct impact of the anterior chest wall (typically impact with the steering wheel). Anterior dislocation is more common and clinically less severe. Posterior dislocations may be associated with major vascular traumas [13]. In the MDCT examination we can find blood collection separated from the lungs and pleural cavity by a thin strip of fat (Figure: 4) [14]
In forty-five (40.17%) of patients extra pleural hematomas are caused by injury of the intercostal artery. They occur relatively rarely because of the chest wall injury or a complication of interventions (drainage, insertion of the central venous catheter). Blood accu- mulates between the parietal pleura and endothoracic fascia. In the MDCT examination we find blood collection separated from the lungs and pleural cavity by a strip of fat (Fig. 5) [14].
In 35(31.25%) of all cases a pneumothorax accompanies blunt and penetrating chest trauma. It is the second most common finding after rib fractures. It is caused by direct injury to the pleura, but also by a rupture of the alveoli accompanied by increased pressure in the airways. On CT it is manifested as a collection of gas in the pleural cavity. In chest Xray examinations performed in the supine position, it is often manifested very discretely, and it cannot be seen at all (Fig. 6) [15,16].
The clinical significance of pneumothorax depends not only on its size at the time of initial examination, but also on its develop- ment over time. In 5(4.46%) of the patient’s tension pneumothorax is a serious, life-threatening condition requiring immediate drainage. It is often clinically diagnosed before MDCT. Its basic symptoms include an increase of the volume of the affected hemi- thorax, shift of the mediastinum to the healthy side, and compression of the mediastinal vessels (mainly veins), heart and depres- sion of the diaphragmatic arch (Fig. 7).
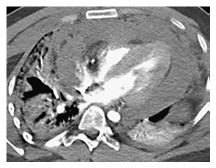
In 39(34.82%) of all cases with hemothorax, bleeding into the pleural cavity is most caused by laceration of the pulmonary paren- chyma and pleural injury. In these cases, bleeding is usually slowly progressive and limited. In 12(10.71%) of cases the injury to an artery (usually intercostal), bleeding progresses rapidly and requires surgical therapy. MDCT is an unrivalled method for the diagnosis of pleural fluid. Blood has a higher density than water. The density of liquid blood is between 30 and 50 HU, and the density of blood clots is 50–90 HU. Hematomas can sometimes have a layered structure (Fig. 8).
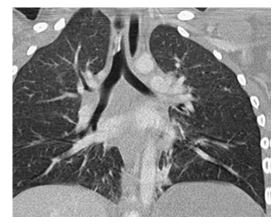
Injury of the lung parenchyma includes pulmonary contusion, laceration, torsion and herniation. These conditions can be complicated by atelectasis, aspiration pneumonia or acute respiratory distress syndrome (ARDS) [6]. Lung trauma is a reason for surgical treatment in 32(28.57%) of the patients. This is indicated in cases of injury of the major blood vessels, signs of active bleeding, large hematomas, or hemodynamic instability.
Pulmonary contusions were found in 79 (70.53%) of all 112 cases and is the most common trauma of the lung parenchyma. It can be detected on the X-ray image with up to a 6- h delay. On the other hand, CT is very sensitive to contusion changes, and it can detect them earlier and more accurately and allows their quantification, which is important in the determination of further treat- ment. In contusions exceeding 20–30 % of the total lung volume, mechanical ventilation is indicated to prevent the development of complications, especially acute respiratory distress syndrome [17,18].
The CT findings depend on the severity of parenchymal affection. Simultaneously, parenchymal lacerations can occur (Fig. 9). The peripheral areas of the lung are affected, and the distribution does not respect boundaries of the lobes and segments [6].
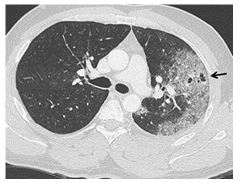
Lung laceration occurs in 64(57.14%) penetrating injuries because of direct shearing forces. At present we can find it relatively commonly because of the broad use of CT in traumatized patients. X-ray examination is usually negative because of superposition of simultaneously occurring contusion changes. If a laceration reaches the pleural cavity, it can cause pneumothorax or hemotho- rax. Laceration closed in the parenchyma has the appearance of a thin-walled, spherical, oval, or tubular cavity containing air, blood, or their combination (Fig. 10). There are usually contusion changes around it. When they are absorbed the laceration, which does not contain air, can mimic a pulmonary node [6].
Lung torsion in 21 (18.75%) of patients is a rare, life-threatening complication of pulmonary surgery or trauma. In rare cases it can occur spontaneously. It affects the whole lung or a lobe [19]. On CT the torsion is manifested as an abnormal position of the lung or its lobe with condensation and obstruction of the airways or distortion and abnormal position of the bronchi and blood vessels [20].
Like torsion in 34(30.35%) patients occurs a lung herniation in a rare complication of chest injuries. It occurs at the site of a defect of the chest wall with a significant increase in intrathoracic pressure. The chest wall defects are caused by multiple fractures of the ribs or by stern- and costoclavicular dislocation. If parenchymal tearing occurs at the same time, the herniation may be associated with pneumothorax and hemothorax [21].
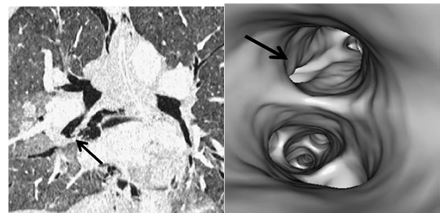
In 59(52.67%) of the patient’s laceration of the trachea and bronchi is caused by two mechanisms—by increasing the intraluminal pressure with a closed vocal slot due to a sudden compression of the chest or by compression of the main bronchi against the spine. A tracheobronchial trauma is often difficult to find. In addition to thin slices in the axial plane and multiplanar reformations, the 3D visualization of the bronchial tree (using virtual bronchoscopy or the volume-rendering technique) can be helpful for detection of the rupture (Fig. 11) [22]. A defect in the wall of the airways with leakage of air into the surrounding area is a direct sign of the airway trauma. Other symptoms, such as pneumomediastinum, subcutaneous emphysema in the neck and chest, pneumothorax and hemothorax, are nonspecific and more commonly have other causes [23].
Rupture of the esophagus is presented in 13(11.60%) patients as a part of a blunt or penetrating chest trauma. Most often, it occurs in the cervical and upper mediastinal part. It is usually caused by bone fragments from the injury of adjacent sections of the spine. The CT findings include thickening of the esophageal wall, pneumomediastinum and paraoesophageal fluid collections. [24,25].
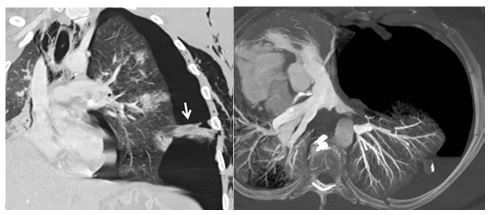
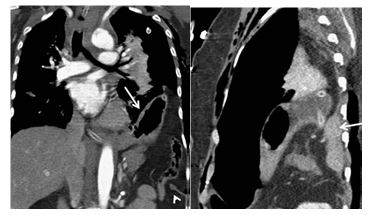
Diaphragmatic rupture occurs in 7(6.25%) of patients hospitalized with a major trauma [26]. It is a frequently overlooked injury, but it is clinically very serious. Laceration in the right side is more difficult to detect. Sensitivity of the initial X-ray examination is low, 17 % and 27–60 % on the right and left side, respectively [27]. Compared to this, MDCT reaches a sensitivity of 50–83 % and 78–100 % in the right and left side, respectively. Evaluation of multiplanar reformations in the coronal and sagittal plane is very important for making the diagnosis. The CT signs of a diaphragmatic rupture include discontinuity of the diaphragm with thickening at the edge of the defect, herniation of the abdominal organs into the chest, strangulation of the organs at their passage through the diaphragmatic defect (collar sign) and location of herniated abdominal organs in the dorsal part of the thorax where they are in contact with the chest wall (dependent viscera sign) (Fig. 12). Diaphragmatic injuries are often associated with injuries of the spleen, liver, lungs, and rib fractures.
Trauma of the large chest vessels represents in about 45(40.17%) of all major trauma patients, but its incidence is probably underestimated. Although relatively infrequent, it is the second most common cause of death after head injuries [30,31]. The aorta is the most affected vessel. Rarely, we can see injuries of the aortic branches, internal thoracic artery, or major mediastinal veins. In the case of a blunt trauma, there are three traumatic mechanisms leading to the trauma—deceleration, torsion and increased intraluminal pressure. Findings on the X-ray examination are usually nonspecific and do not allow to differentiate trauma of the large vessels from other less serious conditions with similar X-ray findings, as described above. [5]. If this type of trauma is suspected, MDCT is currently the first-choice method. Its sensitivity and specificity are almost 100 %. Angiography is indicated only in cases of doubt and for navigation of the interventional procedures [32].
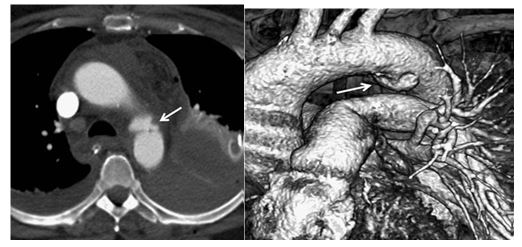
Mortality of untreated aortic trauma exceeds 95 % [33]; Those who come to the hospital have a 70 % chance of survival if the trauma is quickly diagnosed and treated [34,35]. Treatment is either surgical or radio interventional (endovascular stent graft- ing). The most common site of injury (approximately 90 %) is the isthmus, which represents the transition between the relatively mobile arch and fixed descending part. A complete wall rupture (transection) usually results in immediate death. Direct signs of aortic trauma are pseudoaneurysm (Fig. 13), direct extravasation of contrast medium into the mediastinum, intimal flap, irregu- lar contour or mural thrombus.
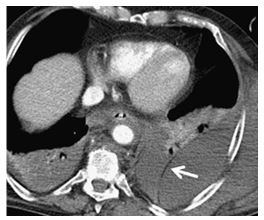
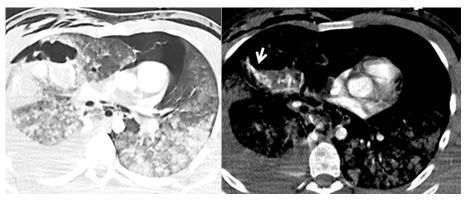
In 28(25%) of patient’s injuries of other blood vessels, such as the internal thoracic artery, branches of the aortic arch, pulmonary artery, or mediastinal veins, are less common than aortic trauma, but their severity is similar. In case of bleeding from the internal thoracic artery, a hematoma occurs in the anterior mediastinum, and it may compress the right ventricle. Injury of the branches of the aortic arch occurs most frequently in the traction mechanism in case of abnormal extension of the neck or pulling of the arm. It is manifested by occlusion, dissection of the affected artery or extravasation of contrast material into the hematoma, which is typically located in the upper part of the mediastinum.
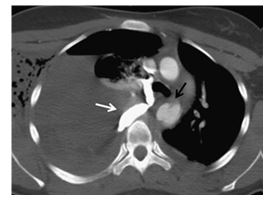
Rare injuries of the venous structures are manifested as hematoma with extravasation of contrast medium (Fig. 14). The mecha- nism is like injuries of the arteries. Injury of the vena cava superior can spread to the right atrium as well [36,37].
Contusion is the most common heart injury in 32(28.54%) of our cases affecting preferably the right ventricle. It is generally ra- diologically silent and causes arrhythmia or other electrocardiographic changes. Because of its very high mortality, cardiac rupture is rarely diagnosed by imaging methods [38]. Diagnosis of hemopericardium using X-ray examination is extremely problematic. The finding can be negative even in cases of cardiac tamponade. In contrast, the CT examination as well as ultrasound is a highly sensitive method. Cardiac tamponade is manifested by flattening and a reduction of the cardiac parts (Fig. 15) [41]. More rarely, we can see pneumopericardium, which, if large, may also result in cardiac tamponade [42]. Herniation of the heart is a serious complication of traumatic rupture of the pericardium [43].
Our experience and literature report suggest that imaging methods are an integral part of the diagnostic algorithm in major chest traumas. MDCT is the main component. It shows traumatic changes quickly, accurately, and clearly, and allows their classification. Therefore, a traumatic radiologist becomes a member of the team making decisions about the therapeutic process.