Nasal Septum Perforation due to Cocaine Abuse
Introduction: Differences in the effect of cocaine based on the route of administration have been an interest of researchers and clinicians for the past few decades. Intranasal administration of the powder form of cocaine (cocaine hydrochloride) was most popular.
Perforation of the nasal septum is an uncommon condition, When it occurs its cause is most often idiopathic or traumatic. Nasal septum perforation may also be the presenting sign of drug addiction. In this article, we describe a case of nasal septal perforation secondary to cocaine intranasal abuse. We also briefly review other common causes of perforation of the nasal septum.
Case Report: This report describes the case of a 56-year-old man who was addicted to cocaine while 10 years and who presented with perforation of the nasal septum.
The patient reported that he had always snorted through the right nostril. There was no history of trauma and no somatic or psychiatric troubles.
In an endoscopic examination a large septal perforation accompanied by excessive necrotic tissues in the nasal space was obvious.
Conclusion: Patient history and assurance regarding illegal drug consumption and abuse is a key point for fast and accurate diagnosis. The pathophysiology of drug-induced sinunasal disease differential diagnoses, treatment are discussed.
Keywords: Cocaine Hydrochloride; Intranasal Administration; Perforation
Cocaine is an alkaloid, which was originally used by South American Indians as a stimulant. It was introduced to medicine by Köller in the 1880s as a local anaesthetic. More recently, its stimulant effects have led to its use as a recreational drug resulting in social, economic and physical harm [1].
Differences in the effect of cocaine based on the route of administration have been an interest of researchers and clinicians for the past few decades. Intranasal administration of the powder form of cocaine (cocaine hydrochloride) was most popular [2].
Perforation of the nasal septum is an uncommon condition; Classically, this type of necrosis has been linked to cocaine intranasal use [3]. When it occurs, its cause is most often idiopathic or traumatic. Nasal septum perforation may also be the presenting sign of drug addiction or a potentially life-threatening or serious systemic illness, even in an asymptomatic patient [1,4-7]. In this article, we describe a case of nasal septal perforation secondary to cocaine intranasal abuse. We also briefly review other common causes of perforation of the nasal septum.
A 56-year-old man presented with nasal congestion, and nasal obstruction. The symptoms were reported to have started only 5 months earlier. he gave a ten years history of nasal cocaine usage, initially at a frequency of two to three times a month but developing into a daily habit.
The patient reported that he had always snorted through the right nostril. There was no history of trauma and no somatic or psychiatric troubles.
On examination her nasal cavities were filled with necrotic debris and extremely sensitive to touch, no deformity in the form of nose was observed. The soft palate, hard palate, tonsils and posterior oropharyngeal wall were normal.
In an endoscopic examination a large septal perforation accompanied by excessive necrotic tissues in the nasal space was obvious (Figure 1 and 2).
Multiple biopsies of the nose and palate were taken and showed necrosis and ulceration with signs of inflammation but no evidence for vacuities or granulomatosis.
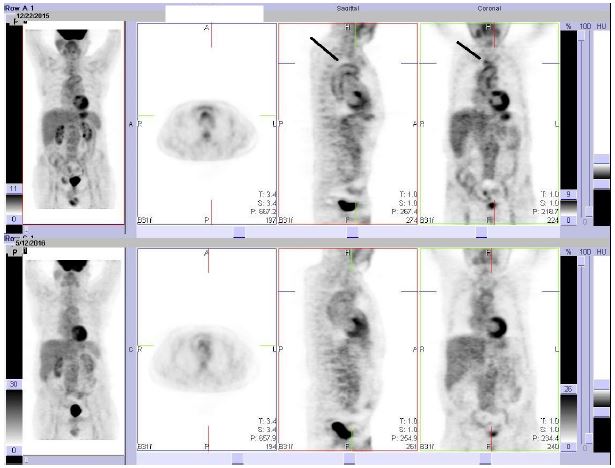
A CT scan of the paranasal sinus showed necrosis of the nasal septum (Figure 3).
Intranasal drug abuse appears to be a growing trend. In addition to cocaine, insufflation of heroin and other opioids, stimulants, benzodiazepines, has been reported [8-10]. Among heroin abusers, insufflation has become a popular method of drug administration, with rates of injection of heroin declining dramatically [11,12]. This shift toward intranasal administration may be due in part to increasing awareness of HIV among drug abusers [13,14].
Erosion of the soft palate and nasal turbinates are more recently reported complications of intranasal prescription narcotic abuse [15].
Xerostomia and septal perforation were discernible in the patient in this case.
Though palatal perforations and destructive orofacial lesions are uncommonly seen in abusers of drugs other than cocaine, clinicians should be aware that a variety of causative agents and pathologic conditions may be associated with this clinical presentation [16-18].
Cocaine induces vasoconstriction and might cause necrosis in the mucosae and surrounding tissues (cartilaginous and osseous). Frequent contact induces nasal septal destruction, choanae, paranasal sinus walls and palatine [13,19].
Ulcerative lesions affecting the midface were considered for differential diagnosis including traumatic, infectious and neoplasic, such as Wegener´s granulomatosis, nasal NK/T cell lymphoma and mucormycosis. Though unfrequent rhinoscleroma and other lymphomas must be also considerer [13]. In 2 of the 3 previously reported cases of destructive lesions resulting from intranasal prescription narcotic abuse, patients were found to have invasive fungal rhinosinusitis [20,21]. This finding is absent in our case and is somewhat surprising, because invasive fungal rhinosinusitis is typically exclusive to immune-compromised individuals [22].
Patient history and assurance regarding illegal drug consumption and abuse is a key point for fast and accurate diagnosis. Furthermore, each attempt to clarify the drug type and route of consumption leads to prevention of this unwanted complication [23]. We can conclude that intranasal cocaine abuse can induce necrosis and focal ischemia that causes secondary mucosa and midfacial bone destruction, and must be differentiated from aggressive neoplasias, inflammatory or infectious processes.