Nephropathy Associated With Prolong Lithium Administration
Lithium carbonate is often used for treatment of bipolar disorder, but caries various side effects affecting kidney function such as polyuria, impaired renal concentrating ability, impaired urinary acidification, and chronic tubule-interstitial nephropathy. Additionally, while the renal nephropathy due to prolong lithium therapy with minimal change disease has been well reported in the literature, focal segmental glomeruloseclerosis (FSGS) after discontinuation of lithium therapy has not been commonly described. We report a case from a 54 year-old obese male patient with past medical history of diabetes mellitus and bipolar affective disorder with treatment of lithium for 10 years presented with recent worsening of proteinuria and serum creatinine. Renal biopsy revealed tubule-interstitial disease, glomerulosclerosis and FSGS after discontinuation of lithium therapy. The report outlines the importance of early detection of nephropathy associated with long-term lithium administration is important to prevent progression to end-stage renal disease, and need for more research work in this area.
Keywords: Lithium; focal segmental glomeruloseclerosis; proteinuria; chronic kidney disease
Lithium carbonate is a carbonate salt of lithium and has anti-manic effects. It is commonly prescribed to treat bipolar disorder. Along with the benefits of decreasing symptoms of manic episode, it is frequently associated with toxicity mainly affecting kidney function. Acute and chronic toxicity on kidney function have been described after lithium administration. Because lithium therapy for bipolar disorder requires a long term administration, chronic kidney toxicity are more commonly reported. Lithium induced chronic kidney toxicity disturbs all compartments of kidney, more often affects tubulo-interstitium and glomerular compartment. Common nephropathy associated with chronic lithium administration is nephrogenic diabetes insipidus, presenting as polyuria and polydipsia, due to impaired renal concentrating ability and impaired urinary acidification [1-3]. Other chronic renal diseases associated with prolong lithium administration are chronic changes as tubular atrophy and interstitial fibrosis as well as glomerulopathy, both usually are diagnosed by kidney biopsy [4,5]. In general patients with Lithium-induced glomerulopathy present with proteinuria in various amounts, some reach nephrotic range, and are non-immune complex mediated glomerulopathy. Many reports regarding glomerulopathy associated with chronic lithium toxicity nephropathy are minimal change disease [6-9]. Only a few of focal segmental glomerulosclerosis (FSGS) have been reported in the literature [10-12]. In this report we describe a case of kidney biopsy in a patient presented with proteinuria after long-term administration of lithium carbonates for bipolar disorder and the FSGS was detected after discontinuation of lithium therapy [13]. All other features of lithium nephropathy including progression of tubular atrophy and interstitial fibrosis, and global glomerulosclerosis, as well as multiple cysts formation are revealed in this patient’s kidney biopsy.
The patient was a 54 year-old male with significant past medical history of diabetes mellitus, hypertension and bipolar affective disorder. The bipolar affective disorder was diagnosed when he was 22 year-old and was treated with lithium carbonate in maintenance dose of 300 mg t.i.d. In several acute episodes, the dose was increased to 600 mg t.i.d until the symptoms were controlled. The bipolar disorder was in full remission when he was 32 year-old, approximately 10 years after lithium carbonate administration. Other medical history included hypertension and chronic obstructive pulmonary disease, as well as subclinical hypothyroidism.
The patient was found to have proteinuria (3+) on urine analysis and elevated serum creatinine (1.85 mg%). He was referred to nephrology to further evaluation.
Physical examination revealed obese male (weight: 298 lbs, BMI 41.58 kg/m2).
Mouth/Throat: No oropharyngeal exudate.
Eyes: Conjunctivae was normal. Pupils were equal, round, and reactive to light. No scleral icterus.
Neck: No thyromegaly was present.
Cardiovascular: Normal rate, regular rhythm and normal heart sounds. No murmur heard.
Pulmonary/Chest: Breath sounds normal. He had no wheezes. He had no rales.
Abdominal: He exhibited no distension and no mass. There was no tenderness. Obese abdomen.
Musculoskeletal: He exhibited no edema.
Lymphadenopathy: He had no cervical adenopathy.
Neurological: He was alert and oriented to person, place, and time. No cranial nerve deficit.
Skin: Skin was dry.
Psychiatric: He had a normal mood and affect.
Protein in 24-hr urine collection was 310 mg/24hr. No white and red blood cells were detected. Specific gravity was 1.005 and pH 6.5. Other lab findings included blood urea nitrogen: 36 mg/dL; creatinine: 1.85 mg/dL. Serum sodium138 mmol/L, potassium: 5.5 mmol/L, serum calcium is 9.5 mg/dL; serum albumin: 3.6 gm/dL; total protein: 7.2 gm/dL; His hemoglobin and hematocrit were 10.4 gm/dL and 31.1% respectively. Two years later, the patient’s serum creatinine was worsening up to 2.55 mg% from the baseline 1.85 mg% and proteinuria increased 630 mg/24 hr. in 6 months.
An elevated serum creatinine combined with proteinuria indicated chronic kidney disease with glomerulopathy for this patient. Possible underlying causes included diabetic mellitus, obesity associated glomerulopathy and lithium associated glomerulopathy, such as minimal change disease or focal and segmental glomerulosclerosis. Therefore, a CT-guided core needle biopsy was performed to address above issue.
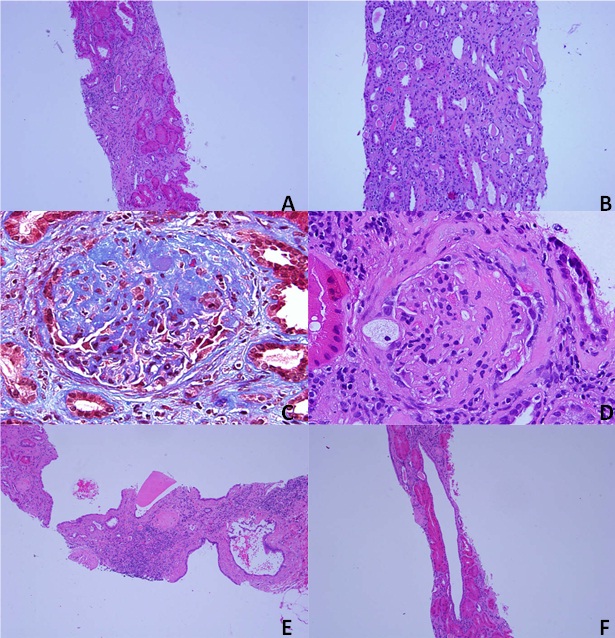
On light microscopy, sections stained with H&E, PAS and silver methenamine reveal 2 portions of renal cortico-medullary tissues, both with capsule. On serial sections, at least 12 glomeruli were present, but 4 of which were globally sclerotic. The remaining glomeruli were normocellular. Two glomeruli showed segmental sclerosis, 1 associated with foam cells and hyalinosis, another showed adhesion to Bowman’s capsule. The tubular atrophy and interstitial fibrosis were moderate, overall tubular losses were 25-35% of sampled the renal cortex. Non-specific lymphocytic interstitial inflammation was seen in areas of tubular atrophy and interstitial fibrosis. In addition, multiple simple cysts with single epithelial lining were also seen. Arteries up to intra-lobular caliber were present and showed mild intimal fibrosis. No active arteritis was present.
No immune complex was identified by immunofluorescence study. On electron Microscopy, the glomerular basement membranes showed normal trilaminar structure and normal thickness. There was diffuse podocyte foot processes effacement with focal microvillus changes. No electron dense immune deposit or tubule-reticular inclusion was identified. In summary, significant finding in kidney biopsy was focal and segmental glomerulosclerosis along with global glomerulosclerosis (4/12, 33.3%) on background of moderate tubular atrophy and interstitial fibrosis (25-35%). In addition, multiple simple cysts were seen in both renal cortex and medulla. Clinically the patient did not have any uremia or volume overload. Discussed with patient he was advanced chronic kidney disease and progression to dialysis possible. He should keep blood pressure and lipids well controlled. Also advised to follow diet to reduce weight.
In kidney, lithium exerts its actions by competition of magnesium, so the function of magnesium-dependent G proteins, such as vasopressin-sensitive adenylyl cyclase is impaired. Since vasopressin involves in regulation of vascular tone of kidney, kidney with long term administration of lithium results in kidney’s chronic ischemia. Santella, et al. found eight reports in the literature suggesting a cause and effect relationship between lithium therapy and nephropathy [10]. All patients showed partial or complete remission with discontinuation of lithium therapy, and three patients showed recurrence when lithium was restarted. Kidney biopsies of these patients showed tubulo-interstitial disease, glomerulosclerosis and minimal change disease [14].
While the tubulo-interstitial disease, including tubular atrophy and interstitial fibrosis, is the result of direct lithium injury on tubule-interstitial compartment, the focal segmental glomerulosclerosis is considered to be a secondary phenomenon due to loss of tubules in nephron. This patient, discussed in this report, had FSGS then progression to globally sclerotic glomeruli. There is also experimental evidence that suggest the possibility of FSGS may be the result rather than the cause of proteinuria [15]. The “focal and segmental” nature of FSGS requires good number of glomeruli on biopsy to be diagnosed, so those reported “minimal change disease” may be because of lack of enough renal sample or in early stage of disease that is immature to develop morphological lesion. Furthermore, Glen. et al. report biopsy proven lithium associated nephropathy in 24 patients [13]. Biopsy specimens of these patients revealed a surprisingly high prevalence of focal segmental glomerulosclerosis (50%) and global glomerulosclerosis (100%), almost of equivalent severity to the chronic tubule-interstitial disease. Podocyte foot processes effacement on electron microscopy examination in these cases suggested a severe podocyte injury for FSGS rather than minimal change disease. Unlike Santella et al studies this study support our findings where despite discontinuation of lithium, patients progressed to end staged renal disease because of FSGS but not minimal change disease. Glen, et al explained that by Kaplan-Meier survival analysis, creatinine level of more than 2.5 mg/dl is a single significance predictor of progression to ESRD [10,13] (Figure 1).
Observation of our patient who had prolonged lithium therapy showed the progression of chronic kidney disease to end stage renal disease even though lithium was discontinued long time ago (approximately 20 years). Diabetes is also a contributing factor in the development of nephropathy however, it is worth keeping in mind that prolong lithium use can lead to progression of tubular atrophy and interstitial fibrosis [16,17]. This explains the importance of early detection of nephropathy to prevent progression to end-stage renal disease despite discontinuation of lithium. This area is open for more research work.