Non-Surgical Management of Large Periapical Cyst Like Lesion: Case Report and Litterature Review
This case report describes the non-surgical management of a large cyst-like periapical lesion in the mandible of an 11-year-old child with the chief complaint of periodic swelling from the mandibular anterior region with a history of traumatic accident in this area. Both mandibular left central and lateral incisors had enamel-dentin fracture.
Root canals of these teeth were filled with calcium hydroxide. After 6 weeks, endodontic therapy was carried out on both teeth. Clinical and radiographic monitoring at 3 months revealed progressing bone healing. Complete periapical healing was observed at the 12 month recall.
This report confirms that for management of a large periapical lesion the non-surgical procedure is essential and it can lead to complete healing of large lesions without invasive surgical treatments.
Keywords: Large Periapical Lesion; Mandibular Incisor; Orthograde Endodontic Therapy
Periapical radiolucent lesions of endodontic origin are caused by carious or traumatic pulp necrosis. They belong to chronic apical periodontitis. They are defined as being inflammation of the apical periodontium that is of pulpal origin [1]. Periapical lesions generally represent an inflammatory response to invasion of the root canal system by microorganisms and their by products [2]. It is viewed as a dynamic encounter between the host’s immune response and microbial infective factors at the interface of the periodontal membrane and infected pulpal tissue that results in local inflammation, resorption of hard tissues, destruction of other periapical tissues [3]. In spite of the defensive and preventive nature of these periradicular lesions to microbial infection, they are not self-healing [2-4].
Chronic apical periodontitis could be classified as granulomas, pocket cysts (also called as bay cysts) and true cysts. Granulomas usually composed of solid soft tissue, while cysts have semi solid or liquefied central area usually surrounded by epithelium. Pocket cysts have an epithelium lining that is connected with the root canal and true cysts are completely lined with epithelium and not connected with the root canal [1,5]. Epithelial cell rests of Malassez in the periodontal membrane are responsible for creating the epithelial lining of cysts. Radicular cysts may grow via a diversity of mechanisms, such as proliferation of epithelial cells or osmotic intensification [4].
It is generally accepted that periapical lesions cannot be differentially diagnosed as either radicular cysts or apical granulomas based on radiographic evidence alone, although there is a trend towards an increased incidence of cysts among larger lesions [6].
The treatment of this pathology constitutes a real challenge in Odontology. Various treatment options presented for large periradicular lesions may range from a root canal therapy to different surgical interventions [4].
Previous investigations demonstrated that large periapical lesions may be treated by non-surgical endodontic approaches. In fact, this usually occurs when the lesion has direct communication with the root canal system which can be improved with pus drainage through access cavity preparation (apical granulomas or pocket cysts). But, when the lesion is separated from the apical foramen and covered thoroughly by an intact epithelium (true cysts), it may not heal after non-surgical therapies [4].
Considering all this, non-surgical root canal treatment should always be the first choice in cases of non‑vital teeth with infected root canals. Elimination of bacteria from the pulp system using an efficient chemo mechanical preparation is the most important factor for the successful treatment of periapical lesions [2,4].
Mechanical instrumentation alone is unable to completely eradicate the root canal system from bacteria. Therefore, some form of chemical irrigation and disinfection is necessary to optimally disinfect the root canal system. Various medicaments have been widely advocated to help eliminate bacteria, reduce periapical inflammation and pain, and induce healing. Calcium hydroxide has been commonly used as an intracanal medicament [2].
The following case report describes the management of a mandiular large periapical cyst like lesion by non-surgical endodontic treatment using calcium hydroxide [Ca(OH)2].
We reported a case of an 11-year-old female attended to the Department of Pediatric Dentistry in Consultations and Dental Treatments Center, Rabat, Morocco, with the chief complaint of periodic swelling in the mandibular anterior region. The patient gave a history of trauma to her anterior teeth when she was 10 years old. At that time, she did not seek any treatment for the same.
Extra-oral examination showed non-palpable lymph nodes and no facial swelling.
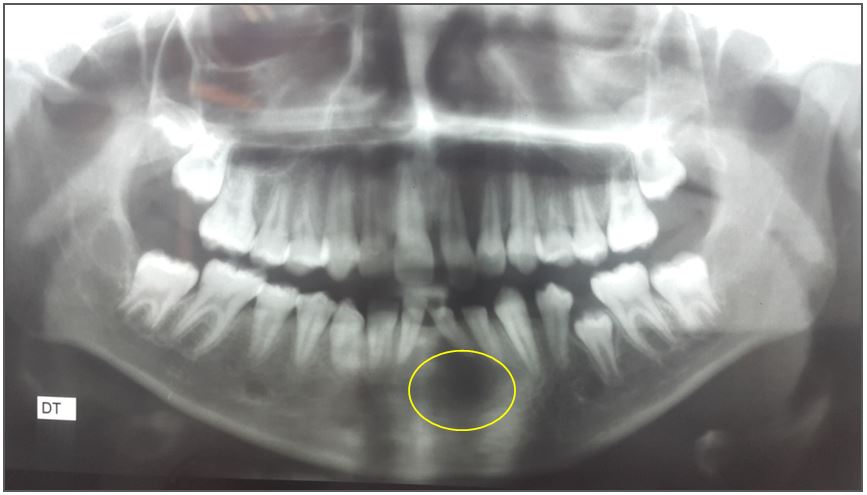
Oral examination showed poor oral hygiene and enamel dentin fracture on 31 and 32 (Figure 1). This examination showed no remarkable findings, including tooth mobility, sensitivity to percussion, or swelling. Vitality tests were done, 31 and 32 was found to be non-vital. The visual examination of the other teeth shows a crown fracture with exposed pulp on 21 and carious lesions in the first permanent molars.
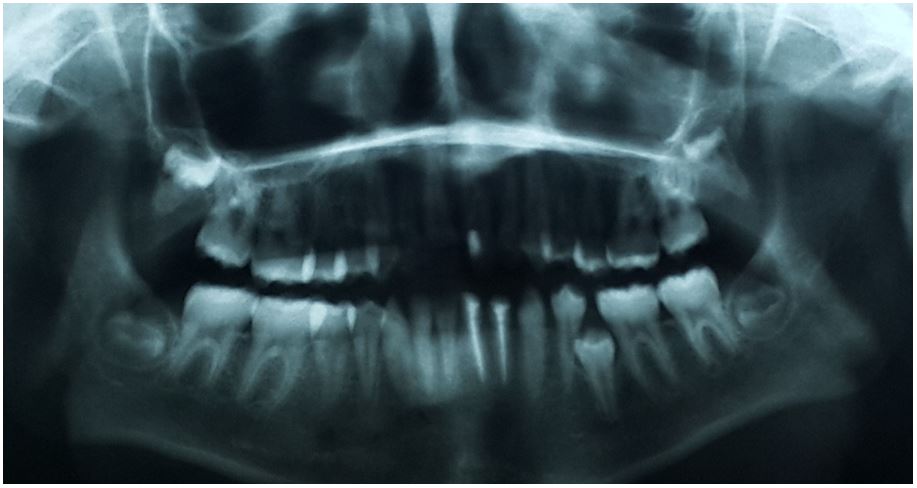
Retroalveolar and panoramic radiograph were done (Figure 2 and 3). There was a large unilocular radiolucent of up to 10 mm in diameter with a uniform radiolucency involving the apices of 31 and 32. There is no typical margin in the lesion because of secondary abscess, but the range is so large that diagnosed as “cyst-like lesion”. Both the teeth are mature. Also, radiography showed diversion of incisor roots.
The diagnosis retained is a chronic apical periodontitis of endodontic origin caused by dental trauma unsupported.
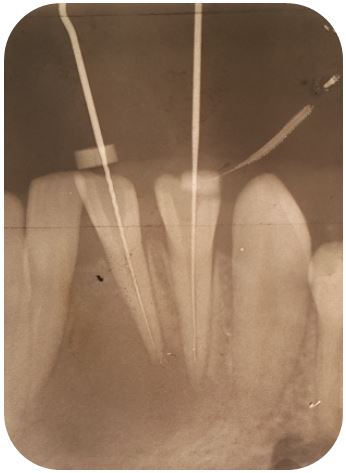
It was decided to perform root canal therapy on teeth 31 and 32. After preparation the access cavities, a suppurative fluid was drained through the cavities. Working length was determined and crown-down instrumentation was accomplished with abundant irrigation with 2.5% sodium hypochlorite at every change of instrument (Figure 4). Calcium hydroxide was given as an intracanal medicament. Access was sealed with glass ionomer cement.
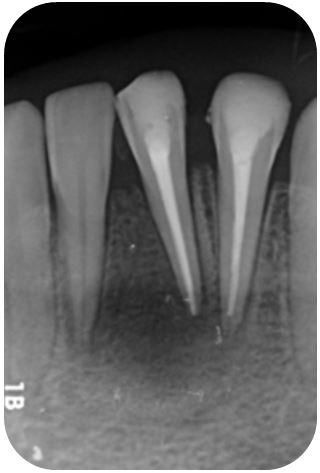
Similar procedure of irrigation and closed dressing with calcium hydroxide was repeated after 3 weeks interval due to the persistence of intracanal exudation. Both the canals were dry so obturated with gutta percha and zinc oxide eugenol sealer cement using the lateral compaction method (Figure 5). One week later, a permanent coronal restoration was made with glass ionomer cement and composite resin.
On clinical examination after 3, 9 and 12 months, no swelling was seen and no discomfort was reported by the patient. Both the teeth are functional.
Retroalveolar radiograph after 3 months exhibited bony trabecular formation in the lesion (Figure 6).
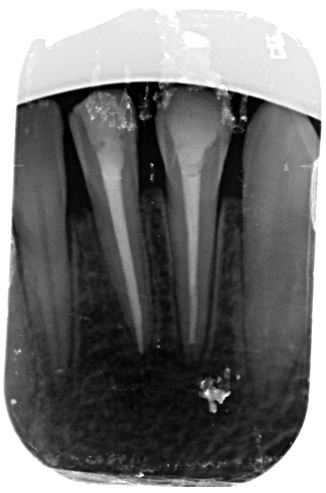
At 9 months after endodontic treatment (11 months after the beginning of management), retro-alveolar radiography showed a significant regression of the periapical lesion with a recovery of the root axes of the mandibular incisors (Figure 7).
At 12 months, the panoramic radiograph showed complete healing of the lesion (Figure 8).
Inflammatory cyst-like periapical lesions which originated from endodontic conditions undergo slow asymptomatic evolution and attain remarkable radiographic dimensions [5]. Such lesions grow via a variety of mechanisms, including osmotic fluid accumulation in the lumen, epithelial proliferation, and molecular mechanisms [2]. They are generally diagnosed either during routine dental radiographic examination or following acute toothache [7]. Historically, periradicular lesions of up to 10 mm in diameter was considered as periapical granulomas and larger ones were recognized as periapical cysts although the definitive diagnosis could only be confirmed by biopsy [5,6].
The incidence of cysts within periapical lesions varies between 6 and 55% [7,8]. This incidence is reported to be highest among patients in their third decade of life and greater among men than women. They have particularly high incidence in the maxillary anterior region, presumably as a result of trauma [6].
The definitive diagnosis of the type of periapical lesion can only be made by a histological examination. However, a preliminary clinical diagnosis of a periapical cyst can be made based on the following [6-8]:
- The periapical lesion is involved with one or more non-vital teeth,
- the lesion is greater than 200 mm2 in size,
- the lesion is seen radiographically as a circumscribed, well-defined radiolucent area bound by a thin radiopaque line, and
- it produces a straw-colored fluid upon aspiration or as drainage through an accessed root canal system.
Histopathological studies, including the distinction between granulomas, epithelio-granulomas and the two classes of periapical cysts, true or in pocket, have shown that among all these lesions, the prevalence of true cysts remains less than 10% [1]. This prevalence has a great importance on the therapeutic choice adopted since more than 90% of the periapical lesions are likely to cure by a conventional endodontic treatment [1].
Because it is clinically and radiographically impossible to differentiate a bay cyst from a true cyst, as it is likewise between a cyst and granuloma, judicious treatment planning should favour a conservative approach to treatment [1,6]. Various methods can be used in the non-surgical management of periapical lesions: the conservative root canal treatment, aspiration-irrigation technique, a method using calcium hydroxide, the apexum procedure…[7,8].
Packing the canal system with calcium hydroxide was considered a concervative approach to the management of a large cyst-like periapical lesion [6]. The whole mechanism of action for this paste is still unclear [4,7]. It is recommended that calcium hydroxide paste can improve periapical repair and eliminate residual microorganisms. Moreover, it has been shown that calcium hydroxide dressing strongly promotes periapical healing, notably in young adults [4].
Prolonged use of calcium hydroxide and overflow with the product beyond the apex (intentionally or accidentally) have been associated with successful non-surgical management of many cases of wide-spread periapical lesions [6].
Sathorn, et al. [9]. (2005) found no statistically significant difference in terms of cure of chronic apical periodontitis of treated teeth in a single session or in multiple sessions with transient calcium hydroxide-based intracanal medication. In addition, Yusuf B. et al [10]. Found in their study that the long-term use of Ca(OH)2 was associated with weakening of the root canal dentin and increased tooth fracture risk. Similarly, Caliçkan demonstrated that teeth with periapical lesions, in which calcium hydroxide paste protrudes beyond the apex, did not show a different healing pattern from those treated conventionally [11].
For these reasons, in spite of the indisputable biological benefits of calcium hydroxide, its prolonged use or any overtaking with the material in the lesion is no longer justified [1,6]. The control of root canal infection and periapical exudation has pivotal importance in the non-surgical management of large cyst-like periapical lesions. In addition, the use of calcium hydroxide intracanal dressing after chemomechanical preparation provides supplementary antisepsis associated at stimulation of periapical repair [5].
In other words, whether a periapically involved tooth is affected by a granuloma or a cyst, non-surgical endodontic therapy may be the treatment of choice [1,12]. A non-surgical approach should always be adopted before resorting to surgery [7]. If the periapical lesion does not heal properly, an apicoectomy can be performed at a later date [1,12]. The advantages of non-surgically managing patients with large periapical radiolucencies are that the psychological trauma is less and is more comforting to the patient [7]. The postoperative complications may increase with the use of surgical procedures [13]. After surgical treatment of large lesions of endodontic origin, it is difficult to obtain good bone healing. Sometimes only scar tissue healing is obtained. As a result of the surgical procedure and even after the membrane is laid, bone healing inside is not always achieved. But it will be a restitution ad integrum after orthograde endodontic therapy [14].
Permanent restoration after endodontic treatment affects the prognosis and sufficient coronal restoration should be placed as soon as possible [4].
After proper non-surgical endodontic therapy, most periradicular lesions except apical true cysts heal. The processes of wound healing of periapical lesions after non-surgical endodontic therapy follow the same principles as that of connective tissues elsewhere in the body. Once irritants in the canals are removed by chemomechanical instrumentation and the canal is completely sealed, all cell components participating in inflammatory reaction will gradually resolve [15].
This healing is a dynamic process, and sufficient time is required to evaluate its progression and completion. The kinetic of the healing of these lesions is variable [16]. Thus, after one year, 90% of lesions likely to heal already show signs of repair (reduction in the size of the lesion), but only 50% of these lesions heal completely in one year [1,16]. In two years, the majority of lesions is healed or continue to show signs of repair by reducing the size of the lesion [1,6,16]. Reduction of the radiolucency occasionally continues for 4–5years [1,16]. The younger patients having a better prognosis than older patients [1].
Those lesions should be monitored clinically and radiographically to ensure such resolution. Endodontic treatment outcomes should be defined in reference to healing and disease, as follows: healing, healed, disease. When follow-up reveals a combined clinical and radiographic normalcy, the tooth and surrounding tissues are classified as having healed. When the radiolucency has persisted without change, that is an expression of disease even when there is clinical normalcy. To accommodate the fact that healing processes may require considerable time, reduced radiolucency combined with clinical normalcy can be interpreted as a suggestion of healing in progress [16].
The absence of healing of large lesions of endodontic origin after endodontic therapy can be justified by the persistence of bacteria in the endodontic system, the extrusion of septic debris beyond the apex, the presence of extra-radicular bacteria capable to survive in the periapex (Actinomyces and Arachnia), the true cysts, the reactions to foreign bodies (dentin debris, cellulose from absorbent paper tips ...) or the accumulation of certain degradation products tissue such as cholesterol crystals [1]. In these situations, a priori clinically unidentifiable, the therapeutic remedy, after orthograde reprocessing, remains endodontic surgery [1].
In the present case, a large periapical lesion, which, according to the above mentioned criteria, was probably a periapical cyst. The size of lesion related with two non-vital teeth, the existence of straw-colored exudate, and divergence of adjacent teeth roots strongly demonstrated a radicular cyst [4]. However, a definitive diagnosis is histopathologic. For the management of this lesion, an antibacterial calcium hydroxide-based paste dressing was placed and repeated after 3 weeks interval. The teeth were obturated after 6 weeks. One week after obturation, composite restorations on both teeth were placed and were further followed up after 3, 9 and 12 months. After which complete healing was seen.
This patient was a young healthy subject and these factors will contribute to successful radiographical and clinical healing; previous studies have showed that the patient’s general health may have an influence on the healing process in periradicular lesions [17].
This case confirms the potential utility of non-surgical treatment protocols for management of large cyst-like periapical lesions. This approach should always be adopted as a routine measure in large periapical lesions of endodontic origin. Conservative orthograde endodontic therapy demonstrates favorable outcomes [18]. Long-term success is dependent on adequate and appropriate cleaning and shaping of the root canal along with proper and correct obturation of the entire prepared space [19].
Due to a more or less discreet and uncomplicated symptomatology, the radiography provides a crucial element in the diagnosis of a large cyst-like periapical lesion of endodontic origin. However, only histological examination makes it possible to differentiate between the forms that exist. Faced with this difficulty of differential diagnosis, it is necessary to carry out a careful orthograde endodontic therapy and to institute a rigorous follow-up to evaluate the necessity of performing endodontic surgery in case of refractory lesions.