Novel Use of C-MAC in A Non-Anaesthesia Field
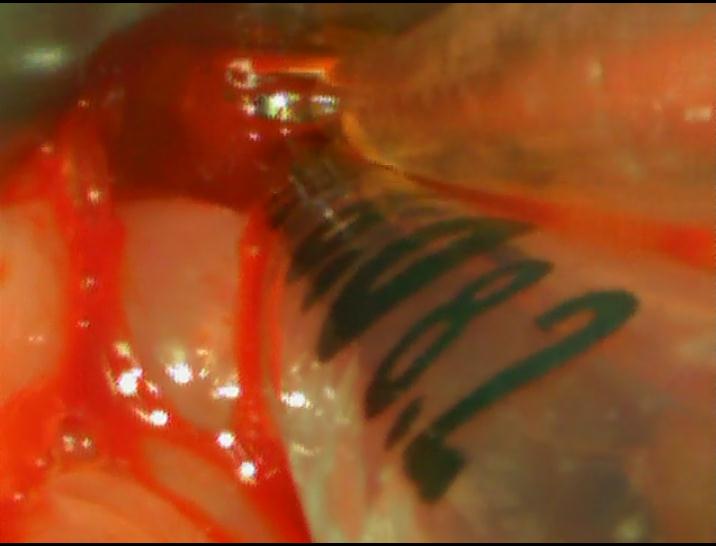
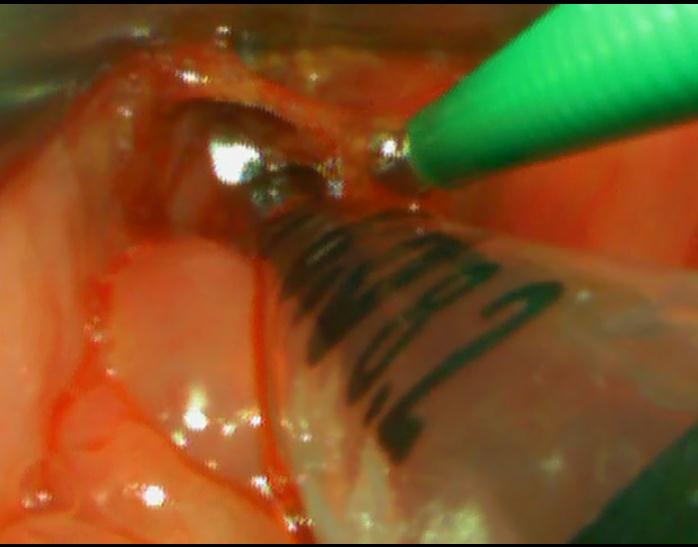
A 56 years old 65 kg male patient with a diagnosis of vocal cord growth was posted for Direct Laryngoscopy biopsy. On airway assessment his Mallampati score was II, mouth opening was adequate, the temporomandibular distance was more than 6.5 cm and neck movement was slightly restricted. After shifting to the operation theatre all the monitors, like 3 lead ECG, NIBP and pulse oximeter were attached. An Intravenous cannula was placed in the left hand with a 20 g cannula. The patient was preoxyginated for 3 minutes with 100% oxygen. Then, induction of anaesthesia was done with intravenous injection Propofol 140 mg and intravenous 50mg rocuronium was given after confirming the adequacy of mask ventilation. Intubation was done with 6 mm ID PVC micro laryngeal endotracheal tube using a bougie. It was an anticipated difficult airway. Two attempts were required, as Cormac Lehane grading was 3a. The situation was harder for head and neck surgeons as they had to take a biopsy as well as excise vocal cord growth which was situated anteriorly. They were not able to see any portion of vocal cord with their direct, rigid, straight laryngoscope. They were about to abandon the procedure. Then, we suggested them to use C-MAC D blade with flexible bronchoscopy biopsy set. With the use of C-MAC visualization of growth was significantly improved but directing the bronchoscope towards the desired area was still difficult as bronchoscope was very flexible, thin and was continuously slipping downwards. Then surgeon was suggested to use the suction catheter of size 16 F and it was directed easily over the tube to the target area (Figure 1). Biopsy wire was then passed through the suction catheter and biopsy was taken successfully (Figure 2). At the end of the procedure, the patient was extubated uneventfully.
Since the arrival of C-MAC video-laryngoscope by the Karl Storz GmbH & Co. KG (Tuttlingen, Germany) in 1999, it is well known to provide both direct and video laryngoscope with the same device [1,2]. Several significant advantages like upgraded laryngeal visualization without the need for alignment of three airway axes, especially in difficult airway scenario, the magnified airway image offering ease to identify the airway anatomical structures. Moreover, a shared visualization opportunity, improve the coordination between intubator and assistant thus change difficult airway management practice from “I” to “we” [3-5].
A completely portable setup that features an improved image quality by means of improved optics, the field of view, interface for adjusting video quality, and easy recording of imaging even by a standard video output port [1,2,6]. The C-MAC D Blade due to its narrowed, half-moon shape and broader angle provide a wider view. The problem encountered with such features is an incompatibility with the angles of a routinely used endotracheal tube. Thus, directing the endotracheal tube within the mouth into the trachea is difficult [3]. It increases the number of attempts, duration of intubation, chances of trauma. Now it is well accepted to use a stylet as an intubating aid to decrease hassles [3].
Use of C-MAC in managing the difficult airway is popular and well accepted. But its successful use in the surgical field is not very frequently documented. In the course of our experience, C-MAC became a novel device to the surgeon, holding them from abandoning the direct laryngoscopy biopsy. Our idea to offer them C-MAC D Bade device with modification was fully successful. 16F suction catheter became the conduit for flexible biopsy wire to the desired area of the larynx. With this experience, failed with Macintosh laryngoscope, we used C-MAC for insertion of Ryle’s tube and Freka tube intraoperative. It decreases the number of attempts, time and trauma to the oropharynx.
ECG: Electrocardiogram; NIBP: Non-Invasive Blood Pressure; ID: Internal Diameter