Odontogenic Keratocysts in Gorlin–Goltz Syndrome: How to Manage?
Odontogenic keratocysts (OKC) is a frequently reported manifestation of the Gorlin–Goltz syndrome, particular among young people. There are two types of treatment conservative or surgical treatment.
A close clinical monitoring is needed as the high risk of malignant transformation of this syndrome.
Keywords: Basal Cell nevus syndrome; Odontogenic cysts, Gorlin’s Syndrome
The Gorlin-Goltz syndrome (GGS) is an autosomal dominant disorder characterized by a predisposition to neoplasms and other developmental abnormalities [1].
The first case was described by in 1960 by Robert James Gorlin and William Goltz with skeletal abnormalities, presence of multiple OKC and Basal Cell Carcinoma [2,3].
The odontogenic keratocyst (OKC), currently designated by the World Health Organization as a keratocystic odontogenic tumor is a locally aggressive, cystic jaw lesion high growth potential and a propensity for recurrence. OKC is a frequent manifestation of Gorlin–Goltz syndrome (GGS) and can be its first sign, mainly in young patients.
This syndrome has numerous names as basal cell nevus syndrome, multiple BCC syndrome and fifth phacomatosis [4].
A specific gene suppressor, called Patched (PTCH) located in the 9q22.3 chromosome, was identified as potential cause of GGS) [5,6].
That gene mutation results in loss of control of several genes known to cause many disorders and have an affect on organogenesis, carcinogenesis and odontogenesis responsible the development of GGS [7-10].
The prevalence is about 1/60000 live birth, and it has both sporadic and familial incidence [11].
This syndrome affects both male and female equally and is seen during the first, second, third decades of life [12]. The management of this syndrome requires a multidisciplinary approach and the treatment is mostly surgical.
The purpose of our study is to provide an objective basis for therapeutic management of OKC and a review of the scientific literature.
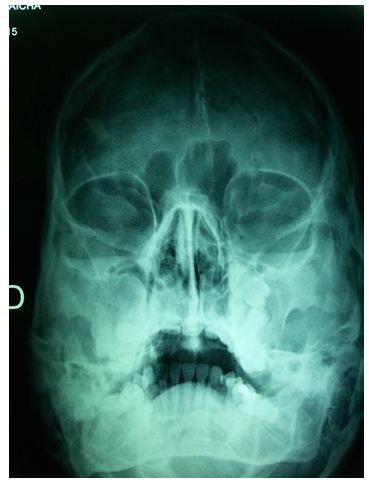
A 22-year-old female patient, with no particular medical history, presented at the oral and maxillofacial for the management of several maxillomandibular cysts (Figure 1). The orthopantomogram was performed by a dentist who found a bilateral lower vestibular bulge.
One lesion was in left ramus with the impacted 38 tooth, of about 2cm × 2 cm and another lesion was in the right and the left body of mandible from 47 to 45, of about 4 cm × 2 cm and the last one was in the left body o from 37 to 36 of about 3cm × 2 cm. She had reported to the dentist with a chief complaint of swelling in the left side of lower jaws. It had started as a small swelling that increased in size over 10 months.
The patient was the fifth child of non-consanguineous parents there were no familial history of similar lesions.
Clinical examination revealed dysmorphic facial features including mild macrocephaly, frontal bossing, hypertelorism, multiple nevi of size on the face and suspected nodular lesions on the left lower eyelid and on right side of the forhead.
Other examinations were also performed which included skullradiograph showed calcification of falx cerebri (Figure 2) and bridging of sella turcica.
The biological assessment was without particularity
Under general anesthesia, extended ward’s incision was placed in the left ramus region. Cyst enucleation and surgical removal of 38 was performed. On the right body of the mandible, a crevicular incision with relieving incision was placed from 48 to 45 and cyst enucleation was performed. Carnoy’s solution was applied on the exposed bony walls with preservation of the inferior alveolar neurovascular bundle in the cystic cavities for 3 min, and charring effect was achieved. The cystic cavities were then irrigated thoroughly with normal saline and closure done with 3-0 Vicryl
Simultaneously, the tumor on the forehead and on the lower eyelid were removed, the defect consecutive was repaired by local flap (Figure 3).
The specimens were sent for histopathological examination
Histopathological report revealed and confirmed the presence OKC and basal cell carcinoma.
Based on clinical, radiographic and microscopic data, the diagnosis of Gorlin-Goltz syndrome was established.
New bone formation sites were identified in the three month radiological follow-up. The patient is being followed-up for past 6 months on a regular basis without evidence of any recurrence. In addition, molecular genetic studies confirmed PTCH 1 germline mutations.
The patient and his parents are aware of the importance of regular examination.
According to the clinical criteria of Kimonis, et al. the diagnostic criteria of GGS require the presence of two major, or one major and two minor criteria ( Table 1) [13]. OKCs are among the most consistent and common features of GGS. They are found in 65 to 100% of affected individuals [14].
Clinically, the lesions are characterized by aggressive growth and a tendency to recur after surgical treatment. The mandible is involved more frequently than the maxilla and the posterior regions are the most commonly affected sites [15].
There are two methods for the treatment of OKC, a conservative and an aggressive. In the conservative method, simple enucleation with or without curettage and marsupialization are suggested. Aggressive methods include peripheral ostectomy, chemical curettage with Carnoy’s solution, and resection [16].
Radical interventions as enucleation with shaving of surrounding bone or sometime resection might contribute to preventing recurrences and to improve the prognosis [17,16].
In the following cases the aggressive method should be applied:
1) When OKC recurrence is reported after a conservative method 2) in cases of multilocular (multilobular) aggressive intraosseous OKC; 3) in a diagnosed OKC exhibiting particularly aggressive clinical behavior (eg, growth, destruction of adjacent tissues) that should require resection as the initial surgical treatment [18]. In our case, as far as OKC is mulilocular without any aggressiveness, a conservative method was appropriate.
Although some authors believe that simple enucleation might be the most appropriate conservative method for the treatment of OKC [18].
Application of Carnoy's solution into the cyst cavity for 3 min after enucleation results in a lower rate of recurrence (0–2.5%) without any damage to the inferior alveolar nerve [19,20].
Although benign, the recurrence rate after excision of OKC is 12% to 62.5%, that’s due to a higher rate of proliferation of the epithelial lining [21,22].
Regular follow-up by a multi-specialists team should be offered (Multidisciplinary follow-up should be offered in long-term. An annual dental panoramic radiograph is usually suggested between the ages of 8 and 40 years to aid in monitoring the recurrence or development of new OKC [23,24].
Moreover it is of great importance to make a dermatological examination every 3-6 months with removal of basal cell nevus showing evidence of growth, ulceration or hemorrhage. The patient must prevent harmful exposure to ultraviolet and ionizing radiations that increase the risk of developing basal cell carcinoma.
The authors are grateful to the patient and their family for their contribution to this article. Written consent for publication was obtained from the patient.