Parietal Bone Metastasis of Rectal Adenocarcinoma as an Initial Diagnosis of Recurrence: Case Report
The most common metastatic sites of colorectal cancer are the regional lymph nodes, liver, lung, and peritoneum. Parietal bone metastasis without vertebral bone metastasis from colorectal cancer is an unexpected situation. Herein, we report an unusual metastasis from colorectal cancer.
Keywords: Skull metastasis; Parietal bone metastasis; Metastatic colorectal cancer
Colorectal cancer (CRC) is a most common and lethal disease of the gastrointestinal tract [1]. CRC can usually spread by lymphatic and hematogenous routes. The most common metastatic sites are the regional lymph nodes, liver, lungs, and peritoneum [1]. Uncommon metastasis of CRC were described such as skin, muscles, skull and thyroid [2-6]. Involvement of unusual sites with metastasis frequently occurs in the presence disseminated disease. Thus, the patient presented with widespread metastasis had poor prognosis [4]. Although all types of tumors lead to metastasis to skull hematogenous route, breast cancer and lung cancers are associated with the highest rate, skull metastases of CRC are quite rare [5]. Parietal bone metastasis without vertebral bone metastasis from CRC is an unexpected situation. The most common presenting symptom of skull metastases is a visible, localized swelling of skull produced by growing tumor [7]. Herein, we report a case of patient with a visible, localized swelling of skull.
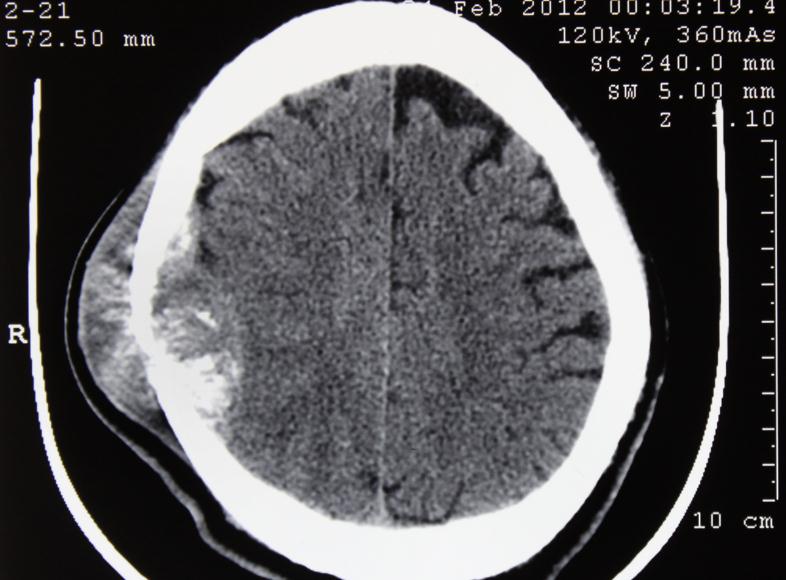
A 44-year old man had diagnosed with adenocarcinoma of the rectum as a result of colonoscopic biopsy in July 2009. Fluoropyrimidine-based neoadjuvant chemoradiotherapy had performed. “Low Anterior Resection” was held in September 2009 and after surgery 4 cycles adjuvant chemotherapy had admitted. The patient was followed in remission until February 2012. He had presented with a mass approximately 6 cm in diameter located his temporoparietal region in February 2012. The mass had grown rapidly in 4 or 5 months. Because of tumour diameter and pain, he had applied to Neurosurgery Department. Magnetic resonance imaging (MRI) showed a 6.0x4.0 cm mass, extending from bottom of scalp and epidural space (Figure 1). The mass had excised with parietal bone. After histopathological evaluation of parietal bone, the diagnosis was metastatic adenocarcinoma. Immunohistochemical analysis was positive for TTF-1, CK-19, CK-20 and CDX2. The specimens were negative for PSA, CK-7, CD10, surfactant. The final diagnosis was metastatic adenocarcinoma of CRC. He applied to Medical Oncology Department in April 2012. Palliative radiotherapy was performed to parietal bone. After the radiotherapy to the parietal bone, infusional 5-fluorouracil, leucovorin, and irinotecan and bevacizumab (FOLFIRI-BEV) was planned but he refused chemotherapy. He applied to Medical Oncology Department because of neurological complaints in July 2012. After re-staging new metastatic lesions detected in lungs, brain metastasis. Bone scan revealed widespread skeletal metastasis. Palliative radiotherapy was performed to painful bone lesions. Due to poor performance status no chemotherapy applied and he had followed up with best supportive. The patient died 9 months after the diagnosis of parietal bone metastasis.
CRC is a most common disease of the gastrointestinal tract and the second most common type of primary cancer in both and women in the world [8,9]. The most common metastatic sites are the regional lymph nodes and visceral organs. Bone metastases typically occurs with other visceral organ metastasis. The most common metastatic bone lesions are shoulder, pelvis, femur and vertebral column. The average time of metastasis is approximately two years after primary tumour rejection. Five-year survival rates of metastatic rectal adenocarcinoma is approximately 6% [1,10].
Skeletal metastases with colorectal cancer occur in 5-10% of cases and usually after widespread metastatic disease. The most likely route for skeletal seeding is through Batson’s plexus, a valveless system of veins draining to the vertebral column. The usual pattern of metastasis is through the liver and lungs, thus making isolated skeletal metastases uncommon, at 1 -2%. [5,11,12]. The other unusual metastatic site is skull [5]. Although surgical excision of unusual metastasis such as skin, skull, scapula of colorectal cancer cannot influence the course of the underlying disease, the mean survival time and morbidity can be improved by surgery [12-14].
Onesti et al. reported scapula metastasis of CRC. The patient treated with chemoradiotherapy followed by chemotherapy with infusional 5-fluorouracil, leucovorin, oxaliplatin and bevacizumab (FOLFOX-BEV). After 12 cycles, the because of developing side effects, the regimen has changed to FOLFIRI. After chemotherapy, the patient underwent surgery [12].
Fahrtash et al. reported a cervical metastases of colorectal cancer with pathological fracture as an initial diagnosis. Palliative radiotherapy to the cervical spine in 10 fractions of 30 Gy has performed. After palliative radiotherapy, FOLFOX chemo regimen had started [15].
In this case, we present a parietal bone metastasis of rectal adenocarcinoma as an initial diagnosis of recurrence without vertebral bone metastasis after approximately 3 years. The rectal adenocarcinoma of this patient was diagnosed in 2009. Neoadjuvant chemoradiotherapy, low anterior resection and adjuvant had performed. He was followed-up until 2012 asymptomatically. He presented with a visible, localized, round subcutaneous nodules. This symptom is also most common symptom of the patient with presenting skull metastasis [7]. To date, only a few metastatic adenocarcinoma of gastrointestinal tract tumours to skull had been reported [5,16,17].
As a conclusion, physicians should keep unusual metastasis of colorectal cancer in mind involvement of unusual sites with metastasis frequently occurs with the other visceral organs in the presence disseminated disease. Because unusual metastasis with the other visceral organs behave more aggressive.