Penetration Syndrome : About a Case of an Intra-Bronchial Foreign Body in an Infant at Dschang District Hospital
Foreign body (FB) inhalation into airways of the respiratory system is a life-threatening and an emergency condition that may be fatal. Children of all ages may ingest a FB, however the highest incidence is between the ages of 6 months and 3 years, and in those with developmental or behavioural problems. Delayed diagnosis and treatment may lead to complications and death. We report a case of an infant who presented with persistent crying, cough and dyspnea. He was treated for asthma in a primary health care center for four days. Since there was no improvment he was brought to a district hospital where thoracic radiography was performed and signs of intrabronchial foreign body seen. In fact, parents unrecognized clinical feature of inhalation of peanuts into airways. He had an intra bronchial foreign body with fatal issue after delay of diagnosis and management by performing the rigid bronchoscopy removal under general anesthesia. The prevention of this domestic accident should consider the population lifestyle and cultural habits to be more effective and the best way to manage it is an early diagnosis and a rigid bronchoscopy removal under general anesthesia used by fully trained staff.
Keywords: Case Report; Foreign Body; Unrecognized; Peanuts
Upper airway foreign bodies remain relevant in pediatrics and are potentially serious, potentially fatal [1]. The penetration syndrome is manifested by a sudden attack of suffocation accompanied by a barking expulsive cough. It is the pathognomonic inhalation syndrome that is often underestimated and the evaluation of which in the literature is variable [2]. This syndrome is noted in 70 to 85% of cases, but, may have been overlooked and then forgotten. It is essential to make this clear during the interrogation [3]. Children under three are more vulnerable and peanuts are responsible in almost 50% of cases [4]. The consequences of inhalation depend mainly on the foreign body, its volume, its nature, its location and the duration of its stay. However, the anatomical and physiological peculiarities of the air axis are important to take into account, especially in young children. A rounded foreign body passes through the glottis more easily, but it is often responsible for a more severe obstruction, its wall sealing the cylindrical bronchial cavities [5]. Any suspicion of an intra-bronchial foreign body requires the practice of bronchoscopy [6]. We present the case of a seven-month-old infant who inhaled peanuts and who died from them despite endoscopy, after a delay in diagnosis and inadequate initial management.
This is a 7-month old male infant, received urgently, in consultation, for severe respiratory discomfort, progressing for four days.
The illness had started four days before his consultation, when he was at the family home with his maternal grandmother. A family friend had visited them, and was eating roasted peanuts, mixed with corn. Moments after a moment of her grandmother’s inattention, the infant let out a loud cry, followed by a strong inspiration and began to cry and cough incessantly. Respiratory discomfort gradually set in, leading the child’s mother to consult at a nearby health center, where the diagnosis of onset of asthma had been made. The treatment administered was: dexamethazone 1 ampoule of 4 mg IM, with slight relief according to the parents, who returned home. They had consulted again, the next day, in the same center for persistence and even increased respiratory discomfort. The treatment was this time: Azithromycin syrup dosed at 200 mg / 5 ml, or 5 ml per day for 3 days; Bethamethasone 0.05% in drops, or 20 drops 3 times a day for 3 days; Metronidazole in oral suspension dosed at 250 mg / 5 m, or 5 ml 3 times a day for 3 days and Salbutamol in syrup dosed at 2 mg / 5 ml, or 5 ml 3 times a day for 3 days. The worsening condition of the child, under this treatment after three days, had led the parents to see a district hospital.
Born at term of a well-followed pregnancy, he was the second child of two siblings, his older sister being 2 years and 6 months old and in apparently good health. Her 34-year-old married mother had a history of multiple miscarriages before the birth of her first child. The infant had never been sick. His vaccines were up to date. He had good physical growth and good psychomotor development
There was no contagious infection and no medication pending.
He hadn’t presented with a fever or a cold. He was not coughing before this episode
On physical examination: He was very irritable, cried constantly, and was very restless, seeking a position of comfort. He did not have cyanosis but showed significant signs of wrestling with flapping of the wings of the nose, chest indrawing, thoracoabdominal rocking, and inconspicuous wheezing. Its oxygen saturation in ambient air varied between 90% and 94%. His respiratory rate was 66 movements per minute.
It weighed 8750 grams (+ 1DS). Her temperature was 36.7 ° C. Heart rate at 124 beats per minute.
On cardiopulmonary auscultation, the sounds of the heart were audible, regular, without breath; there was a unilateral decrease in vesicular murmur in the right lung, without rales. The remainder of the physical examination was normal.
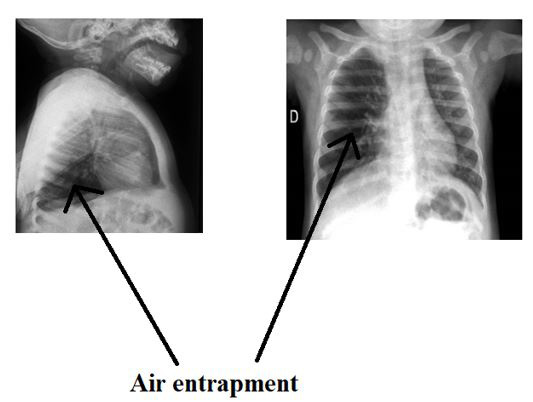
We evoked a penetration syndrome, with probable foreign body of the airways (with an acute bronchiolitis as differential diagnosis) and requested a chest x-ray in inspiration and expiration which confirmed our diagnosis by showing obstructive emphysema of the right lungs by trapping of air linked to the obstruction of the right main bronchus by a foreign body, moreover, radio transparent (figure).
The parents had been informed of the diagnosis and the baby had been sent by ambulance to a referral hospital about, 400km from the city, to an ear, nose and throat specialist (ENT) for extraction of the foreign body. Rigid GA bronchoscopy had been performed with the extraction of four fragmented peanut seeds, but the patient died in a picture of acute pulmonary edema and severe anemia approximately one hour after this procedure. This report was given to us by telephone by the specialist doctor who took care of this baby.
The case of a foreign body that we have presented is typical according to the data in the literature. The peanut remains the public enemy n ° 1, representing more than 50% of foreign bodies inhaled in children, in most statistics [1, 4, 7]. In children, it is the little boy who pays the heaviest price (2/3 of cases) and these accidents occur from the age of grasping (6 to 9 months) reaching a peak during the second year. [7, 8]. Food foreign bodies are poorly tolerated, including oilseeds which are responsible for neighboring bronchial inflammation (peanuts bronchitis) which can go as far as true ulcerations of the wall. These lesions increase the confinement of the foreign body and make extraction particularly difficult (hypervascularized mucosa bleeding at the slightest contact) [5, 9]. The most frequent locations of foreign bodies are laryngotracheobronchial, according to various reviews of the literature [1, 10]. If the foreign body enters the bronchial tree, the right main bronchus is most often involved, due to its obliquity (the bronchial angles with the tracheal axis are similar in children and in adults, 30 ° on the right, 45 ° on the left) and its caliber slightly greater than that of the left mainstem bronchus [10]. This accident is always marked by the penetration syndrome made up of cough, dyspnea and sometimes even respiratory distress, in 70 to 80% of cases, but it can be neglected, or even forgotten, posing a major diagnostic problem. Indeed, the mother of this child did not describe a penetration syndrome, but rather crying preceded by a cry, even though the baby was in respiratory distress. Any hypothesis of foreign bodies was denied by the child’s mother, who believed that her child was having an asthma attack. The history of the disease had been reconstructed retrospectively after the results of the chest x-ray and the announcement of the diagnosis, as that was when the child’s grandmother told the real story, confessing , moreover, that half a peanut seed had come out of the baby’s mouth at the very beginning of the crying. Objective chest x-ray of ventilation disorders with lobar atelectasis, or even of an entire lung (20%), images of condensation attesting to the existence of pulmonary foci most often unique, an obstructive emphysema localized to a lobe or to an entire lung and clearly demonstrated by images in inspiration and forced expiration (50%). The simple notion of penetration syndrome requires tracheobronchial endoscopy, a delay in diagnosis that can lead to serious complications and even death [11]. Our patient had inhaled peanuts which became embedded in the right mainstem bronchus and obstructive emphysema of the said lung was found on the x-ray. Despite his management by endoscopy in a specialized setting, he died postoperatively, in a picture of hemorrhage and pulmonary edema with severe anemia. The limits of this case are essentially linked to the diagnostic delay due to ignorance of the penetration syndrome and to the difficulties in transferring patients which led to a fatal outcome. We should also note the abuse of the use of corticosteroids in our health facilities. We believe that their administration to our patient, having given a slight clinical improvement, had contributed to the diagnostic delay. In addition, data remains insufficient in our country concerning the inhalation of foreign bodies and no regulations exist to date.
The unrecognized penetration syndrome or found very late in the interrogation is frequent, especially when the accident occurs when the small child is alone, or accompanied by an uninformed adult. Obstructive emphysema, by entrapment of air, is best evidenced by taking pictures during exhalation. Bronchoscopy is the rule for any suspicion of an intra bronchial foreign body. It is essential to sensitize and inform parents of the risks run by the child who ingests peanuts / peanuts and the clinical picture which should alert them. Attending to the penetration syndrome and knowing its value should immediately refer the child to a specialized setting in order to avoid progressing to potentially serious complications, or even death.
Conflict of Interest: The authors declare no conflict of interest for the publication of this clinical case.
Authors’ Contribution: All the authors contributed to the realization of this work. They all read the final manuscript.
Acknowledgments: We thank the parents of this baby who allowed us to publish this case.
Informed Consent: The mother of the child had been informed of the publication of this case and had given her informed consent in writing.