Phrenic Paralysis after Chest Trauma: About 3 Cases
Introduction: Post-traumatic phrenic paralysis remains rare and most often related to cervical trauma, whereas attacks following closed or open chest trauma are very rarely reported. Through three cases of post traumatic diaphragmatic paralysis, we will focus on the mechanism of these paralysis as well as on the diagnostic problems encountered and the therapeutic modalities available.
Observation 1: Patient aged 20 years, admitted for multiple thoraco-abdominal wounds, one sitting in parasternal left, another left basithoracic and a third in the right hypochondrium and for whom the chest X-ray shows an elevation of the left diaphragmatic dome. thoracic CT revealed a stomach in the intrathoracic position with liver fracture. The patient underwent laparotomy exploration demonstrating an intact diaphragm with wound of the common bile duct repaired. The chest X-ray of control showed a return of the diaphragm to its normal position.
Observation 2: A 35-year-old patient who was admitted for chest trauma after being turned over and whose lesion showed a right pneumothorax with contusion of the right pulmonary base; important elevation of the right diaphragmatic dome with intra-thoracic position of the liver. The patient underwent thoracic exploration by assisted video minithoracotomy that did not achieve diaphragmatic rupture. The patient is well clinically with progressive return of the diaphragm to its normal position after a six-month follow-up.
Observation 3: 44-year-old patient, admitted to the emergency department for closed chest trauma following an accident on the public highway and in whom the examination finds a polypnic patient. The lesion report showed a right pneumothorax of great abundance, contusion of the right pulmonary base, multiple costal fractures and lesion of liver laceration. The patient underwent right pleural drainage, and in the chest x-ray controls a significant elevation of the right diaphragmatic dome. Thoracic CT showed an abnormally high liver position. a surveillance was decided and the patient is clinically well with a follow-up of 8 months.
Discussion: Post-traumatic phrenic palsies may be related to phrenic nerve stretching in the context of closed chest trauma, or to a section or simple irritation of the nerve in the event of a thoracic wound sitting opposite to its path. The main diagnostic problem lies in the presence or absence of a diaphragmatic rupture, the surgical exploration of which makes it possible to dispel the doubt except in the case where the patient’s condition is precarious and in this case the expectation is a wise decision, particular on the right side.
Conclusion: Post-traumatic diaphragmatic paralysis require long-term follow-up and evaluation of their clinical, respiratory, and somnography impact to provide an indication of surgical repair.
Keywords: Diaphragm; Chest Trauma; Phrenic Nerve
Phrenic paralysis is most often due to tumor invasion, such as invasion from a pulmonary or mediastinal tumor. the surgical trauma, especially after cardiac surgery, or post-traumatic origin remains rare cause of phrenic paralysismost often related to cervical trauma, whereas attacks following closed or open chest trauma remain exceptional [1]. The aim of this work is to report the mechanism of these paralyses as well as on the diagnostic problems encountered and the therapeutic modalities available.
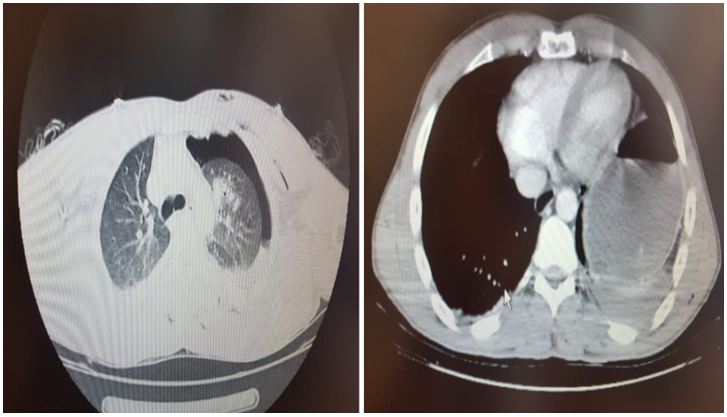
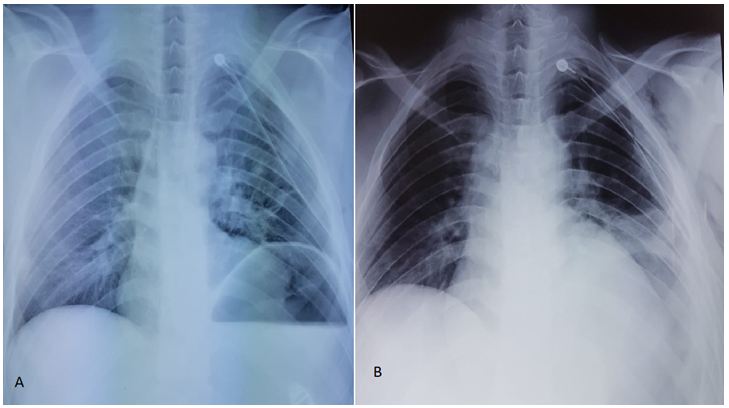
A 20-year-old male admitted for multiple abdominal and thoracic wounds, with a stable hemodynamic state, and a left pleural effusion, with a deep and blowing chest wound parasternal left at the 3rd intercostal space, a second left basithoracic next to the 7th intercostal space on the posterior axillary line and a third in the right hypochondrium. Abdominal examination was without particularity. The chest X-ray showed a left pneumothorax of average abundance. In addition to left pneumothorax, thoracoabdominal CT showed subcutaneous emphysema with respect to the seat of the thoracic wounds, stomach in intrathoracic position with hepatic fracture (Figure 1). The control by the chest X-ray revealed a return of the lung to the wall with elevation of the left diaphragmatic dome (Figure 2A). In view of the suspicion of a diaphragmatic hernia, the patient underwent laparotomy exploration demonstrating an intact diaphragm with wound of the common bile duct repaired. Surveillance by chest X-ray has objectified a return of the diaphragm to its normal position (Figure 2B).
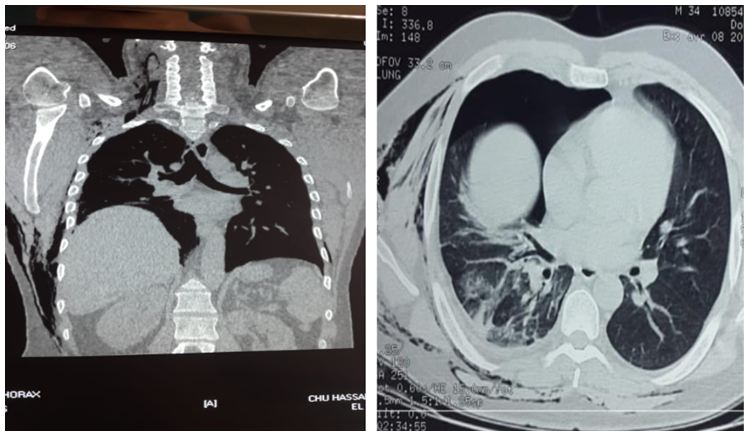
A 35-year-old patient admitted for closed chest trauma following the reversal of his vehicle from which the patient was ejected, and in whom the examination found a stable hemodynamic state, exquisite pain on the palpation of the middle arch of the 4th right rib and right aerial pleural effusion syndrome. Thoracic and abdominal CT showed a lower right lobe lung contusion with suspicion of diaphragmatic rupture and intrathoracic liver herniation (Figure 3), and the chest X-ray showed a right apical pneumothorax with elevation of the right diaphragmatic dome (Figure 4A). The patient underwent thoracic exploration by assisted video minithoracotomy that did not achieve diaphragmatic rupture. The patient is well clinically with progressive return of the diaphragm to its normal position after a six-month follow-up (Figure 4B).
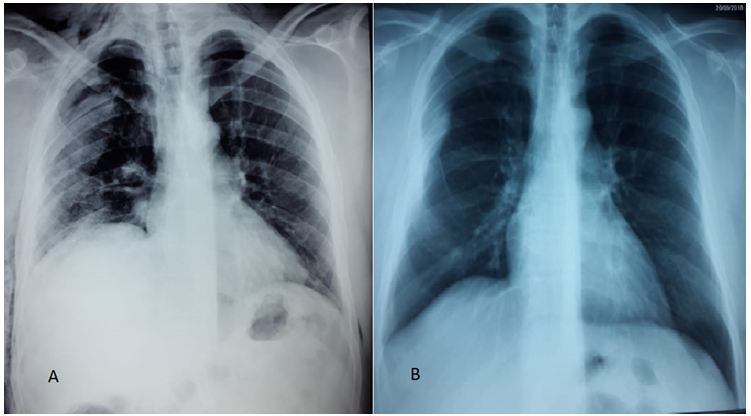
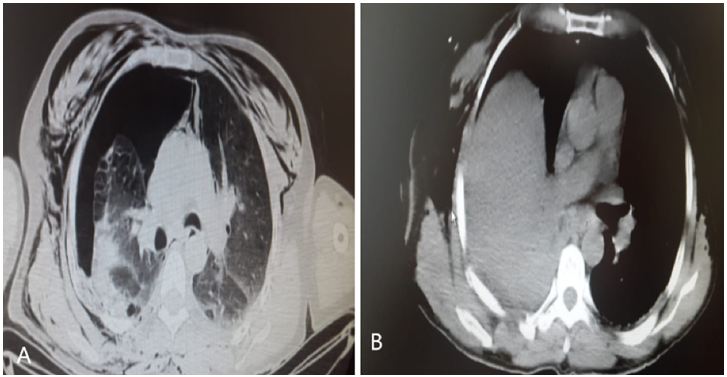
44-year-old patient admitted to the emergency department for chest trauma after a road accident (vehicle hit by another at high speed) and in whom the examination finds a patient with dyspnea. Chest x-ray showed a great abundance of a right pneumothorax. Thoracic abdominal CT showed a contusion of the right pulmonary base, multiple costal fractures and lesion of liver laceration (Figure 5A). After pleural drainage, a chest X-ray showed a return of the lung to the wall and a significant elevation of the right diaphragmatic dome. Chest CT scan showed an abnormally high liver position (Figure 5B). Surveillance was decided and the patient is clinically well with a follow-up of 8 months (Table 1).
Post-traumatic phrenic palsies may be related to phrenic nerve stretching primarily as a result of a deceleration mechanism in the context of closed chest trauma or a section or simple irritation of the nerve in case of a thoracic wound sitting opposite from its cervical origin at C3-C5 to the level of its bifurcation in the diaphragmatic muscle [2-3]. Clinically, and depending on the unilateral or bilateral involvement, diaphragmatic paralysis can be completely asymptomatic and fortuitous discovery as it can result in dyspnea of varying intensity that can lead to respiratory distress in case of bilateral involvement [4-7]. The main diagnostic problem is the presence or absence of diaphragmatic rupture [8,9]. In this sense, the imaging does not confirm with certainty the presence of a diaphragmatic breach except in the case of a abdominal hernia of organs in intrathoracic. Indeed, if the chest x-ray can provide elements of presumption [10], the ultrasound performed in the context of what Anglo-Saxons call the EFAST (extended focused assessment with sonography for trauma), could be a useful examination , especially since it is an examination performed on the bed of the traumatized, non-invasive and repetitive. Ultrasonography can in rare cases highlight the diaphragmatic gap or indirect signs of rupture such as peridiaphragmatic peritoneal effusion, absence of diaphragmatic contraction or visualization of abdominal organs in intrathoracic [11,12]. As for thoracic CT, its sensitivity in the detection of diaphragmatic fractures varies from 50% to 84%. It may suggest diaphragmatic paralysis in the presence of muscle dysfunction observed on inspiratory and expired sections [13,14]. Chest MRI is more sensitive than thoracic CT in the detection of diaphragmatic fractures; however, its feasibility in the emergency setting remains highly controversial [15].
The best way to eliminate a diaphragmatic rupture is surgical exploration by thoracoscopy in a patient in a stable hemodynamic and respiratory state. We are used in our department to practice exploratory thoracoscopy in the face of any penetrating left basithoracic wounds. In the case of the first patient, the exploration was made by laparotomy given the presence of a hepatic fracture. In closed chest trauma, and if the hemodynamic and respiratory state allows it we recommend thoracoscopic exploration. While in the opposite case and especially on the right sided, we favor a simple monitoring at the risk of aggravating the patient’s condition by general anesthesia and at the price of finding only a simple diaphragmatic paralysis recoverable without risk of herniation of the digestive organs in intrathoracic.
Once the diagnosis of diaphragmatic paralysis has been confirmed, an impact assessment must be performed including spirometry while standing and lying in order to quantify the importance of the restrictive syndrome, arterial gasometry, oximetry and polysomnography [16]. Paralysis phrenic can regress in 6 to 12 months in the absence of definitive lesion of the phrenic nerve [2]. Non invasive ventilation (NIV) is one of the non-specific and non-invasive treatments for correcting the symptoms associated with alveolar hypoventilation. In some very specific cases such as unilateral paralysis, surgical plication of the diaphragm may be considered. Paralysis of central origin may, in some well selected cases of supraspinal lesions with intact nerves and muscles, benefit from the implantation of a phrenic stimulator to suppress positive pressure mechanical ventilation by restoring more physiological ventilation.
Post-traumatic diaphragmatic palsies may be due to either a phrenic nerve injury along its path or nerve stretch following closed chest trauma. The main problem lies in the presence or not of a diaphragmatic continuity solution and in this case the best diagnostic means is thoracoscopic exploration when the hemodynamic and respiratory state is stable. If surveillance has been decided, long-term follow-up should be instituted because an unknown diaphragmatic hernia can be several years after the trauma.