Pleomorphic Adenoma of the Para pharyngeal Space: A Case Report and Review of the Literature
Parapharyngel space tumors are infrequent. Pleomorphic adenoma is a slow growing benign tumor, most commonly encountered in large salivary glands and less frequently in small salivary glands. The parapharyngeal space is a very rare site for this tumor. Hereby we describe a case of pleomorphic adenoma in this space diagnosed in 44 year female presented with an oropharyngeal swelling associated with dysphasia and speech disorder.
Keywords: Pleomorphic Adenoma; Parapharyngeal Space; Trans cervical Approach
Parapharyngeal space tumors are infrequent; represent only 0.5% of neoplasms of head and neck. Most of these tumors (70%-80%) are benign and 40-50% of these originate in the salivary glands, particularly the pleomorphic adenoma [1]. The majority of minor salivary gland tumors are malignant [2]. Among benign tumors of the minor salivary glands pleomorphic adenoma is the commonest, found most often in the oral cavity [3].
This tumor in the parapharyngeal space (PPS) can develop de novo or may arise from deep lobe of the parotid and extend through the stylomandibular tunnel into the PPS [4].
A 44-year-old woman, presented to our department with a swelling in the oropharynx since six months ago, the swelling is gradually increasing in size causing progressive odynophagia and speech disorder. The patient is asthmatic with no other history of medical importance. A physical examination revealed bulging mass on the left side of the oral cavity displacing the soft palate anteriorly and extends to the nasopharynx superiorly. The cranial nerves are spared and no significant lymph nodes enlargement were noted.
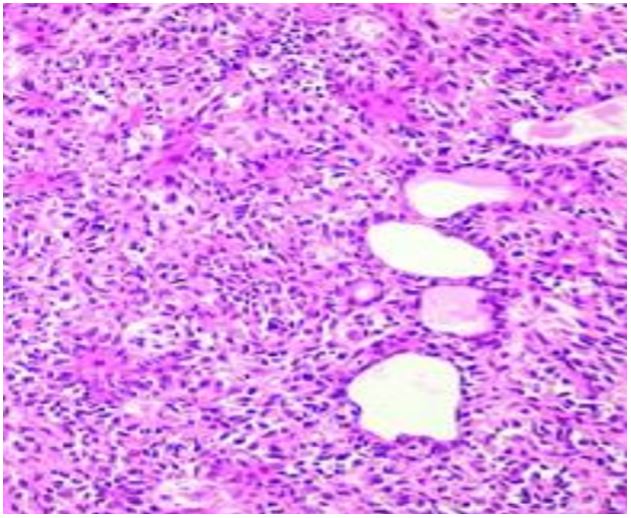
A CT scan of the head and neck showed a well-defined mass occupying the right parapharyngeal space with homogeneous contrast enhancement (Figure 1A), the MRI has demonstrated well circumscribed oval mass of 51×34×44 mm in the retrostyloid parapharyngeal space visible in isosignal T1 and hypersignal T1 injected (Figure 1B). Based on the history, Physical examination and the radiographic findings diagnosis of benign minor salivary gland tumor was established .The patient benefited from an excision of the tumor via a cervical approach with exposure of the external carotid (Figure 2). The pathological examination is compatible with a pleomorphic adenoma (Figure 3). Post-operative period was uneventful. CT scan repeated after 2 years of follow up and did not show any evidence of residual or recurrence.
The parapharyngeal space (PPS) is located lateral to the oropharynx, anatomically shaped like an inverted pyramid with its base at the skull base and its apex at the greater cornu of the hyoid bone [4.6]. Bound medially by the superior pharyngeal constrictor and laterally by the medial pterygoid muscle, mandibular ramus, and deep lobe of the parotid gland [6]. Tumors of this site a very rare, with pleomorphic adenoma being the most common [2]. They are often large at the time of presentation as they may be asymptomatic or misdiagnosed when being small [7]. Tumors arising in the minor salivary gland accounts for 22% of all salivary gland neoplasms [8]. Majority of them are malignant with only 18% being benign. Of the benign tumors pleomorphic adenoma is the commonest [3]. The most common site of a pleomorphic adenoma of the minor salivary gland is the palate followed by lip [8]. Pleomorphic adenoma of the parapharyngeal space is rare. De novo occurrence of the pleomorphic adenoma can arise from displaced or aberrant salivary gland tissue within a lymph node in the parapharyngeal space [9]. This site of origin is in contrast to the tumors that arise in minor salivary glands medial to the constrictor muscles of the pharynx [3.9]. Another source of such a tumor is the deep lobe of parotid gland, in which case the tumor may present either as a dumbbell tumor abutting the stylohyoid ligament or a round tumor within the parapharyngeal space [3]. A comprehensive review of literature showed very few case reports of pleomorphic adenoma arising de novo in the parapharyngeal space [4]. Though most of the benign tumors of the minor salivary gland in the oral cavity present as a painless submucosal swelling, those from the parapharyngeal space may show additional symptoms, like otalgia, neuralgia, palsies of 9th, 10th, or 11th cranial nerves or trismus [1.4].
CT with contrast can define the site of origin and extent of the tumor, as well as its vascularity and relationship to the great vessels of the neck and other neurovascular structures [4]. Contrast enhancement is seen in vascular and neurogenic tumors. Presence of intact fat plane helps in distinguishing benign tumors from malignant [3]. Extension of tumors from the deep lobe of a parotid gland is distinguishable from tumor arising de novo in the parapharyngeal space by a fine lucent line representing the compressed layer of fibroadipose tissue between the tumor and deep lobe of parotid [9]. Histopathologically, pleomorphic adenoma is an epithelial tumor of complex morphology, possessing epithelial and myoepithelial elements arranged in a variety of patterns and embedded in a mucopolysaccharide stroma [9]. Formation of the capsule is as a result of fibrosis of surrounding salivary parenchyma, which is compressed by the tumor and is referred to as “false capsule” [3]. The treatment of pleomorphic adenoma is essentially surgical [3]. The parapharyngeal space is however, a complex anatomic region located between the mandibular ramus and lateral pharynx and extending as an inverted pyramid from the skull base superiorly to hyoid bone inferiorly [9]. Within this potential space are cranial nerves IX, X, XI, and XII, the sympathetic chain, carotid artery, the jugular vein and lymph nodes [9]. The location and surrounding vital structures, resection of tumors from this space can prove challenging to the head and neck surgeon. The approach of choice to the parapharyngeal space to allow adequate removal of the tumor should meet two criteria: wide intra-operative visibility for safe radical dissection and minimal functional and or cosmetic after-effects [3]. The patient was operated through a transcervical approach .Cervical transpharyngeal approach was first described by Roux in 1981. The transcervical approach is commonly used for most PPS neoplasms; it provides good local disease control with minimal risk of facial nerve injury and good cosmetic results [10]. Many authors 8-10 have addressed the need for additional approaches to obtain oncologically safe results, such as mandibulotomy. In particular, Malone et al. 10 described 40% of combined techniques [10]. The transparotid approach is used for tumors of the deep lobe of parotid gland 6. It offers a wide access to PPS, but the risk of facial nerve injury is higher [11]. The transoral approach is the most controversial. It provides limited, direct access to the PPS and makes identification of neurovascular structures more difficult [11]. Some authors suggested robotic transoral resection for large benign masses that are accessible from the oropharynx and involving the poststyloid space [12]. Complications of surgery of the PPS include tumor recurrence, nerve injury, vessel injury and hematoma [1]. Tumor recurrence is possible, especially if the capsule is broken and tumor spillage occurs [3].
The PPS is a complex anatomical region containing many vital neurovascular structures.
This adequate understanding of the anatomy and pathology of the PPS is requisite in the systematic preoperative evaluation of PPS lesions and the choice of a safe and effective surgical approach for their removal.

.JPG)
.JPG)
.JPG)
.JPG)