Posterior Nasoseptal Flap in the Reconstruction of Skull Base Defects Following the Endonasal Surgery
Introduction: To study the clinical outcomes of posterior nasal septal flap in endonasal reconstruction of anterior skull base defects.
Methods: The early harvested flap was used to reconstruct anterior skull base defects among patients with high-flow on-table CSF leak. Post-operatively the patients were analyzed for CSF leak & bleeding.
Results: Of the total 100 patients 87 had macro defects while 13 had micro defects. Non-secretary lesions were present in 60 patients while lesion were present in 40 patients. Cerebrospinal fluid leak was present in all the patients undergoing surgery and majority of them were put on lumbar drain, while bleeding was present in 2% patients. Of the total 100 patients only 2 had post-operative cerebrospinal fluid leak 2%.
Conclusion: Use of posterior nasal septal flap for reconstruction of anterior skull base among patients with high-flow intra-operative CSF leak has a remarkable impact in preventing post-operative CSF leak. Its applicability to wide patient-profiles with respect to age, size of defect, diagnosis is making it a versatile choice of reconstruction after endonasal anterior skull base surgeries.
Keywords: Posterior Nasal Septal Flap; Endonasal Flap; Reconstruction Of Anterior Skull Base; Cerebrospinal Fluid Leak Repair; Hadad- Bassagaisteguy Flap; Pedicled Flaps
In the patients with large dural defects of anterior and ventral skull base, there is a significant risk of post-operative cerebrospinal fluid (CSF) leak. Advances in surgical technique, instrumentation, and intraoperative image guidance have made reconstruction of even large dural defects possible. Reconstruction with the vascularised tissue is desirable to facilitate rapid healing, especially in irradiated patients. Hadad-Bassagasteguy flap (HBF), a vascular pedicled flap of the nasal septum mucoperiosteum and mucopericondrium based on the posterior septal artery (branch of sphenopalatine artery), was first developed in university of Rosario, Argentina, for reconstruction of ventral skull base dural defects [1]. It is increasingly becoming a “workhorse” for the reconstruction in extended endonasal skull base surgery. Endoscopic endonasal repair of traumatic CSF leaks with the posterior nasoseptal flap (PNSF) has a success rate of approximately 95% comparable to that of traditional approaches [1]. Fortes et al used the Hadad–Bassagasteguy flap and reported a 5% incidence of CSF leak, which is similar to the rate after open craniotomy [2]. A posterior nasoseptal flap preserves the possibility of raising a Hadad–Bassagaisteguy nasoseptal flap if needed; therefore, it is indicated when a CSF leak is possible but not probable.
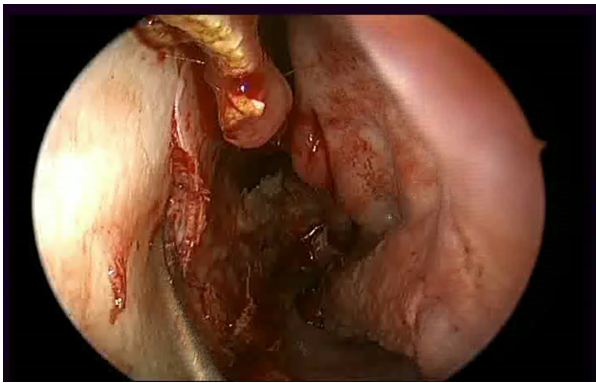
This prospective, non-randomized study was conducted in the Department of Otorhinolaryngology and Department of neurosurgery at Bombay hospital and institute of Medical sciences, Mumbai, Maharashtra from Jan 2013 to Jan 2017. Patient were selected from Department of Neurosurgery and Department of Otorhinolaryngology irrespective of gender, urban or rural population and identified patients who underwent skull base surgery via an Endoscopic endonasal approach (EEA) where the Posterior nasal septal flap (PNSF) was harvested early during the procedure (Figure 1 and 2). Study was conducted in a prospective manner involving 100 patients with CSF leak due to skull base defect following endonasal skull base surgery. Post-operative CSF leak reconstruction was done with vascularised tissue to facilitate rapid healing. These values when applied on the study of Hadad et al and Kassam et al study of patients with using posterior nasoseptal flap and 100 cases were included in the study [1,3]. All the patients who were subjected to endoscopic approaches for resection of skull base pathologies with significant risk of having a cerebrospinal fluid (CSF) leak on pre-operative assessment, with traumatic high-flow CSF leaks with large skull base defects that were repaired with a posterior nasal septal flap (PNSF) were included in this study. Patients with nasal septal injury due to trauma, previous surgery, tumors that infiltrate the nasal septum, pterygoid fossa, or the anterior wall of sphenoid sinus and patients with less the 18 years of age were excluded.
All patients who presented with impaired vision, hemianopsia, headache, nausea and vomiting, oculomotor paralysis, hypopituitarism, polydipsia, polyuria, amenorrhea and galactorrhea underwent a complete preoperative out-patient evaluation by a neurosurgeon, Rhinologist, endocrinologist and neuro-ophthalmologist when indicated. The clinical diagnosis was established after taking a detailed history and doing clinical examination which included systemic examination and local ear, nose and throat examination. The examination of nose included anterior rhinoscopy, posterior rhinoscopy and Paranasal sinus examination. In the investigations included complete haemogram, coagulation profile, liver profile, serum creatinine, human immunodeficiency virus-1& 2, hepatitis B surface antigen, blood sugar and electrocardiogram was done. Endocrine function evaluation, examination of the visual field and visual acuity, radiological evaluation. In radiological evaluation axial sagital and Coronal section CT is essential for a preoperative review of the approach, including bony landmarks and relationships, extent of pneumatization of the sinuses and skull base, and areas of dehiscence with potential for injury. Gadolinium contrast enhanced MRI was done in all the patients for detailed preoperative assessment of intracranial content & extent MR imaging revealed macroadenomas (maximum diameter > 1cm) small non-secretory tumours, less than one centimetre termed microadenoma. Microadenoma can be followed with serial MRIs to monitor for progressive enlargement before proceeding to surgery. A written consent was taken from each patient prior to surgery. All cases were operated under general anaesthesia.
A posterior nasoseptal flap or Hadad Bassagaisteguy nasoseptal flap that involves elevating the pedicle of the Hadad Bassagaisteguy nasoseptal flap. The posterior nasal septal flap was harvested at the beginning of the operation if a high-flow CSF leak is anticipated and was placed in the nasopharynx for protection during the case. The use of a vascular pedicle flap has become the preferred skull base reconstruction. The most commonly used technique is a vascular flap of the nasal septum mucoperiosteum and mucoperichondrium that is pedicled on the nasoseptal artery, a branch of the posterior septal artery, which is one of the terminal branches of the internal maxillary artery. The nasal cavity was decongested with oxymetazoline (0.05%). The inferior, middle and superior turbinate’s are out-fractured to allow the visualization of anterior wall of sphenoid. This was done bilaterally to facilitate bimanual technique, which allows nasoseptal flap to take on one side and reverse flap on other side. The flap was designed according to the size and shape of the anticipated defect. Two parallel incisions were taken following the axial plane of the septum, superior incision at the level of sphenoid ostium up to the level of anterior end of middle turbinate, then curved superiorly, in situation of CSF leak, a standard Hadad–Bassagaisteguy nasoseptal flap can be harvested by extending the incisions coming anteriorly to mucocutaneous junction then extended inferiorly to join inferior horizontal line of incision. Inferior incision starts laterally just above the ET opening and continue along just above the choana on to the septum. It then proceeds anteriorly along the floor of the nose to join the anterior vertical incision and allow elevation of this HB flap. The flap was elevated anteriorly with a freer elevator. Elevation of the flap from the anterior face of the sphenoid sinus is completed with preservation of a poster lateral vascular pedicle. The technique was repeated bilaterally. Wide sphenoidotomy and posterior septectomy were subsequently performed. HB Flap thus elevated can cover defects from frontal recess to the clivus. Reverse flap was harvested on other side, to cover the bare cartilage. Once harvested, the flap was displaced into the nasopharynx until the pathology was removed. After the skull base approach and tumor resection, the subsequent skull base defect is prepared by denuding approximately 1 cm of mucosa around the bony defect to prevent delayed mucocele formation from trapped paranasal sinus mucosa. The sphenoid sinus was also completely denuded of mucosa in the transsellar and transplanum trans tuberculum repairs to avoid potential sphenoid sinus mucocele formation. This step also optimizes flap adherence to the native bone, and prevents residual intervening mucosa from causing delayed flap dehiscence. If there was no intra operative CSF leak, at the end of pituitary surgery the nasoseptal flap was translocated posteriorly to cover any denuded bone at the floor of the sphenoid sinus. But in situation of CSF leak, a standard Hadad–Bassagaisteguy nasoseptal flap can be harvested by extending the incisions. Fat harvested from the thigh or abdomen was used to assist in the repair, if required. Fibrin glue or other biologic glue was used to help secure the flap and nasal packing was done.
Data analysis was performed using Microsoft Office Excel 2007 (Microsoft Corp). Data was stored in a Microsoft Excel 2007 file for descriptive statistical evaluation. The observed data for various parameters was presented in terms of minimum, maximum, and mean and standard deviation for the descriptive analysis.
A total of 100 patients were treated with PNSF for the reconstruction of skull base defects in the endonasal skull base surgery. The mean age of the study subjects was 41.8 ± 13.8 years with approximately equal number of males and females (Table 1). Out of total patients, 87% had macro skull based defects while micro defects were present in about 13% cases. Additionally, non-secretory lesions were present in 60 patients while secretory were present in 40 patients (Figure 3). Headache was the most common presenting complaint (71.7%) followed by decreased vision (56.6%) and acromegaly (13.2%) (Table 2). After the reconstruction by posterior nasoseptal flap, post-operative CSF leak was observed in 2 patients, giving it a failure rate of 2 %. In first patient leak resulted from straining and was observed on 3rd post-op day. The leak was repaired with the help of fascial graft. In second patient, leak was observed on 2nd post-op day. A lumbar drain was inserted with and complete bed rest was advised, the leak stopped subsequently.
The well-known skull base surgeon, Prof. Paolo Cappabianca from Naples said that “reconstruction is more problematic than resection”. Therefore it comes as no surprise that it were the advantages in reconstructive techniques for the closure of surgically induced defects of the skull base that enabled the important progress in endonasal skull base surgery. The ultimate goals of all techniques for reconstruction in the region of the skull base are the stable separation between the nose and the cranial cavity, the protection of neurovascular structures, the conservation or reconstruction of cosmoses, the preservation or reconstitution of function and the avoidance of dead spaces. In this respect, the separation of nasal and cranial cavity is of utmost importance because it prevents postoperative CSF leaks, pneumocephalus, and intracranial infections, and protects cranial nerves and large vessels from infection and trauma. The effects of postoperative radiotherapy also have to be considered. Although a number of different techniques have been used successfully to endoscopically treat CSF-leaks after trauma, iatrogenic injury, or in spontaneous rhinoliquorrhea, these methods have proven insufficient to reconstruct the large defects in extended endonasal skull base surgery [5-8].
Since the neuro-endoscope was applied, especially after EEA, the incidence of complications, such as CSF leakage, infection and encephalocele formation, was high. Carrabba, et al. reported that the incidence of CSF leakage was 24% after EEA [9]. Therefore, the reconstruction of skull base defect is of paramount importance to prevent CSF leakage after endoscopic endonasal surgery [10,11]. In patients with large dural defects of anterior and ventral skull base, there is a significant risk of post-operative cerebrospinal fluid (CSF) leak after reconstruction. Reconstruction with vascularised tissue is desirable to facilitate rapid healing, especially in irradiated patients (Table 3 and 4). Hadad-Bassagasteguy flap, a neurovascular pedicled flap of nasal septum mucoperiosteum and mucopericondrium based on the nasoseptal artery, was first developed in university of Rosario, Argentina, for reconstruction of ventral skull be dural defects [11].
It was not until local vascularised flaps in particular the Hadad-Bassagasteguy flap were developed that the rate of postoperative CSF leaks even after expanded resections at the skull base could be reduced to below 5% [12]. In the landmark study which introduced HB flap, Hadad et al reported a post-operative leak rate of 4.5% without any, partial or complete flap loss, in the study [11] (Figure 4 and 5). And recently, in total, 96 skull base defects with high-flow CSF leaks which included 47 sellar (including 2 revision cases: 1 recurrence and 1 residual tumor) defects, Eloy, et al. reported a post-operative CSF leak rate of 3.1% [11].
A post-operative CSF leak rate of 2% (2/100) observed in our study following the posterior nasal septal flap repair of 100 sellar defects with the use of external lumber drain (ELD) in around 87% of cases keeps well with theses published results of Post-operative CSF leak rates after PSNF. The relatively higher rate (10.66%) of post-operative CSF leak observed by Kassam et al was predominantly found in those patients which required intra arachnoidal dissection and the authors partly attributed it to the initial experience with the technique [12]. Against that all patients in our study has sellar defects; 13/100 macro sellar defects & 87/100 micro-sellar defects. A substantial, non-traumatized & well perfused flap is must for achieving the desired efficacy of the repair technique. The approach of early harvesting of the flap (before resection) is meant to ensure the quality of the flap & there by the repair. Like most of the published studies used we also employed the pre-harvesting approach in all of our patients (Figure 6). Although the exact size of the expected skull base and dural defect is unknown, a good estimation can be obtained by carefully reviewing the preoperative imaging. Early harvest of the PNSF allows harvest of a maximal sized flap that can be tucked into the nasopharynx or maxillary sinus, away from inadvertent trauma during the approach and tumor resection. A maximally sized PNSF that has not been compromised by trauma with a well-preserved vascular pedicle may provide the most robust closure. This is even more important in cases where the approach to access a lesion may involve sacrificing a portion of the PNSF [12].
Disruption of the surgical barrier between relatively septic nasal cavity and highly aseptic arachanoid cavity is inherent to the transnasal approaches to anterior cranial fossa and so is the risk of iatrogenic meningitis. The surgical dissection area that is involved in such surgery will also have an inherent risk of olfactory dysfunctions and like all other surgical procedures post-operative bleeding, especially in an area of compromised access, remains a possibility. Though rare, such complications are real with endoscopic nasal approaches to the skull base. The true extent of rarity of these complications should be viewed cautiously keeping in view the relatively smaller sample size of the all studies reported on the subject till now. Like most of the reported studies we did not find any post-operative episodes of meningitis or nasal bleeding even in those cases which had intra-operative bleeding from cavernous injury (2/100) [4] (Figure 7 and 8).
Kassam et al has reported post-operative bleeding in 1/75 patients. Wang XI (2013) reported a single death due to post-operative meningitis in among 20 patients studied by them. The study however does not specify the kind of mucosal vascular flap used in that patient [13]. None of our patients had significant post-operative nasal synechiae, nasal obstruction or significant nasal crusting.
Some recent published reports have highlighted the olfactory dysfunction that is associated with HD flap reconstruction [14]. According to Bernal-Sprekelsen et al titled, ‘’Management of anterior skull base defect depending on its size and location.” A total of 54 who underwent advanced skull base surgery (large defects >20mm) and 62 patients with CSF leaks of different origin (small 2-10mm and mid-size 11-20mm defects) were included in this retrospective study. Large defects were reconstructed with a nasoseptal pedicled flap positioned on fat and fascia lata. A lumbar drainage was used (Table 5 and 6). In small and mid-sized leaks of other origin intrathecal fluorescein was applied before the surgery to identify the defect. Fascia lata in an underlay position was used for its reconstruction covered with mucoperiostium of either the middle or the inferior turbinate. The success rate after the first surgical reconstruction was of 91% and 98% in large skull base defects and small / mid-sized respectively. After rescue surgery the rate of closure achieved was 100%. They concluded that Endoscopic surgery for closure of any type of skull base defect is the gold standard. The size of the defects does not seem to play a significant role in the success rate. Fascia lata and mucoperiostium of the turbinate allows a two-layer reconstruction of small and mid-sized defects. For larger skull base defects, a combination of fat, fascia lata and nasoseptal pedicle flaps provides a successful reconstruction [14] (Table 7).
Brain WR et al has reported a decrease in mean UPSIT (university of pennsalyvania smell indentification test) scores from preoperative 37.2 (normosomic) to 30.8 (hyposomic).15 These decreased scores of UPSIT persisted even after complete healing at 6 months post-surgery. The authors hypothesized that olfactory impairment results from use of the HB flap, and recommended that the possibility of permanent olfactory changes be added to routine patient counseling and consent for this procedure, and that HB flaps be raised judiciously during trans-sphenoidal endoscopic procedures [15].We regret for not including such evaluation in our study.
The limitations of the study are that the patients were not evaluated for pre- & post-operative olfactory status. Also the study lacked a control group. Lastly, the study is single institutional. Consequently, multi-institutional study as well as prospective randomized controlled double blinded studies would be ideal to validate these results
Endonasal reconstruction of anterior skull base defects by posterior nasal septal flap is associated with very low rates of post-operative CSF leak. As our result show very low rate of CSF leak, endoscopic endonasal skull base reconstruction using a nasal septal flap seems to be useful and reliable for ventral skull base defects after Endoscopic Endonasal Approaches (EEA) as compared with our previous single-layer reconstruction using free fat grafts or fascia lata.