Progressive Myoclonus Epilepsy Responded to Vagus Nerve Stimulation
Progressive myoclonus epilepsies (PMEs) are a group of heterogeneous disorders characterized by different seizure types and multifocal neurological deficit. They have deleterious effect on patient’s life; furthermore failure of medical treatment has a great burden on the patient and caregivers.
The role of vagus nerve stimulation (VNS) in PMEs has been a matter of debate; however recently there is case reports addressed the effectiveness of VNS in such disorders.
The aim of presenting this case report is to support the role of VNS in the treatment of refractory epilepsies such as PMEs.
PMEs are rare disorders with variable subtypes which are usually resistant to anti-epileptic drugs with deleterious clinical effects on the patient, however few cases in the literature have been responded to VNS as in our case, furthermore VNS could control myoclonic jerks in such disorders, and it’s effect can be predicted earlier than it was thought.
More studies are needed in the future to elaborate the role of VNS in the management of such disorders and their clinical manifestations.
Keywords: Progressive myoclonus epilepsies; Vagus nerve stimulation; Refractory epilepsy; Antiepileptic drugs
Progressive Myoclonus Epilepsies (PMEs) are a rare devastating neurodegenerative disorders, characterized by stimulus sensitive myoclonus, action myoclonus, generalized tonic clonic seizures, other types like absence, tonic or focal seizures and cerebellar dysfunction (ataxia, dysarthria, tremors) [1].
Most PMEs have autosomal recessive inheritances, however autosomal dominant inheritance has been described [2].
There are several forms of PMEs with variable prognosis, for example one of the most common form of PMEs is Unverricht–Lundborg disease or what so-called progressive myoclonus epilepsy type 1 [EPM1] has variable phenotype with earlier disease onset and longer duration being linked to severity of the disease [3,4], furthermore this type of PMEs has been reported to carry good prognosis with nearly normal life span if adequate care given to the patient, [4] in another hand some forms of PMEs have a devastating course like Lafora body disease, neuronal ceroid lipofuscinoses, and neuro-nopathic form of Gaucher disease [2].
Another rare variant of PMEs is related to mitochondrial disorders for example, MERRF syndrome or myoclonic epilepsy with ragged red fibers [4,5] and MELAS or mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes [5].
Antiepileptic drugs like valproate, clonazepam, and phenobarbital (or primidone) are more commonly drugs used to control generalized tonic clonic seizures and myoclonic jerks, however their effect is reduced with advanced disease progression [6].
It’s well known that some of antiepileptic drugs (sodium channel blockers carbamazepine, Oxcarbazepine, Phenytoin and GABAergic drugs (Vigabatrin and Tiagabine), as well as Gabapentin and Pregabalin) may exacerbate myoclonus and generalized tonic clonic seizures as well [6].
Vagus nerve stimulation (VNS) has been introduced in the treatment of generalized and focal epilepsies since 2003, with favorable outcome of approximately 50% seizure frequency reduction, furthermore in some cases the improvement may reach up to 75%, this effect may related to accumulated effect of vagus nerve stimulation [7].
It was thought that vagus nerve stimulation effectiveness start several months after VNS implantation [8], however recent study showed earlier response to VNS stimulation than it might be expected which could be seen from (0-4 months) after implantation and seizure freedom rates increase over time with VNS therapy [8,9].
They are several case reports that address the role of VNS therapy in controlling seizures in patient with PMEs, furthermore its role in myoclonus, cerebral symptoms and mental retardation yet to be clarified by further studies [10].
Vesper J, et al had reported a case of undetermined syndrome, in which generalized seizures responded well to VNS with deterioration of myoclonic jerks [11].
We reported a case of 32-year-old male patient, right handed with seizure onset at the age of 7-years.
He reported no auras and he has multiple seizure types started with drop attacks 1-2 per year, and then he developed generalized tonic clonic seizures with frequency of one every two days, at times he would have very frequent uncountable myoclonic jerks with history of fall down and fracture of the left ankle.
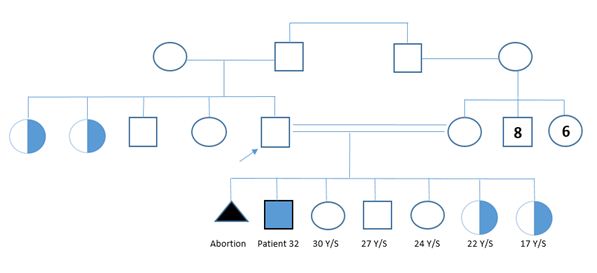
He is a product of full term pregnancy, his pregnancy was uneventful, delivered vaginally, without surgical or instrument interventions, no neonatal intensive care unit (NICU) admissions and no other risk factors, however he had positive family history of (2paternal aunts and 2 sisters with the same disease and seizure types as well). The parent of the patient are first degree relative, as shown in family pedigree below (Figure 1).
He was started on Valproic acid and then Clonazepam was added later on, despite of that he progressively deteriorated in terms of having daily myoclonic jerks, and his activities of daily living have been affected, so Topiramate was added without additional benefit.
The patient was compliant to his antiepileptic drugs, and he continued following with Epilepsy clinic, ultimately Levetiractem and Lamotrigine were added without significant benefits.
Clinical examination showed normal vital signs. He was oriented to time, person and place, normal language, however he has mild to moderate cognitive impairment.
Apart from horizontal nystagmus cranial nerves were intact.
Patient is unable to stand possible due to previous fracture in the left ankle as well ataxia and positive cerebral signs.
Tone and reflexes were normal.
Basic laboratory investigations include: complete blood count, Electrolytes, liver functions tests, and renal profiles were normal, Serum Lactate – 1.9 mmol/L (1.1-2.2), LDH – 211 U/l (135-225), TSH: 4.15 mlU/L (0.27-4.2), T3 and T4: normal, antithyroid antibodies: normal, unremarkable tandem MS, normal Male karyotype 46- XY on cytogenetic analysis.
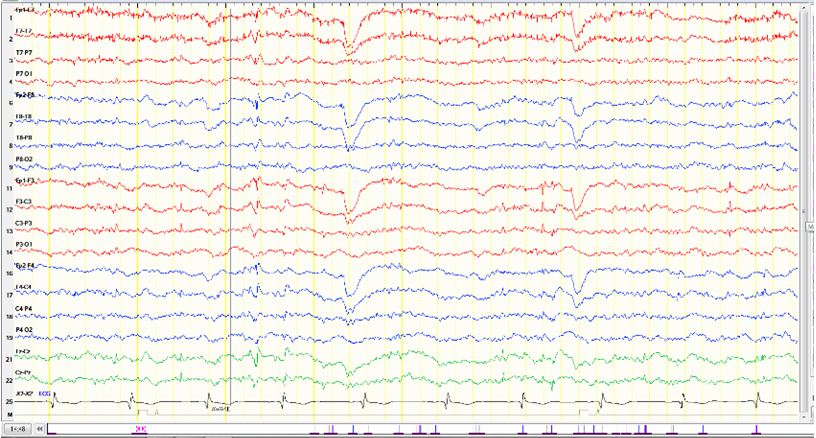
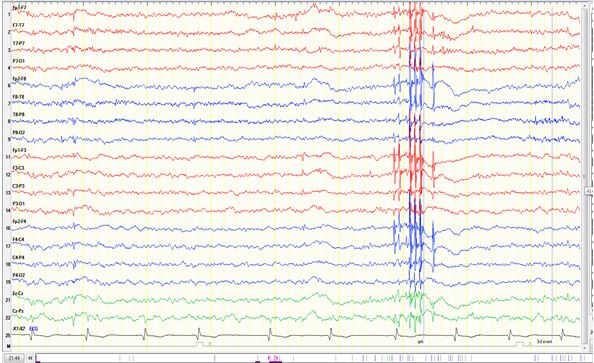
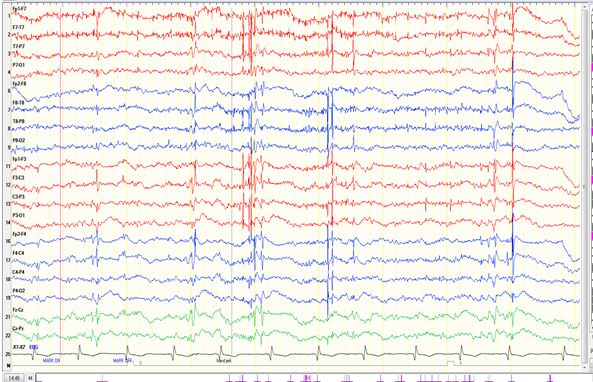
Electroencephalography (EEG) showed poorly developed posterior background consisting of 6-7 Hz of medium amplitude, superimposed by diffuse Beta activity (possible due to Clonazepam). Sleep potentials were symmetric, frequent multifocal and generalized spikes associated with positive and negative myoclonic jerks (Figure 2, 3, and 4).
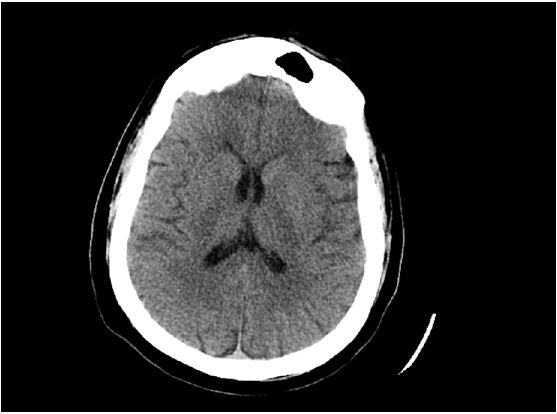
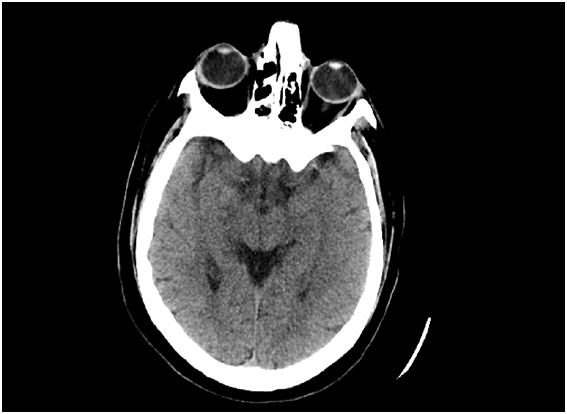
Magnetic resonance imaging (MRI) brain epilepsy protocol was not combatable with metal in the left ankle, brain CT was unremarkable (Figure 5 and 6)
He was admitted to Epilepsy Monitoring Unit (EMU) for seizures classification and pre surgical evaluation, during EMU admission we could capture frequent myoclonic jerks as well as polymyoclonus, unfortunately few months later he had very frequent seizures requiring admission to High dependency unit, after we controlled his seizures, vagus nerve stimulation implanted on May, 2015.
3 months later after VNS implantation with the following parameter:
Output current of 0.5 mA, signal frequency of 20 Hz, pulse width of 250 microseconds,
The patient and his family reported significant improvement of seizures frequency in terms of disappearance of generalized tonic clonic seizures (GTCs) and significant reduction of myoclonic frequency and intensity, no changes have been made on his anti-epileptic drugs.
On follow up and at output current of 1.75 mA, signal frequency of 20 Hz, pulse width of 250 microseconds, No generalized tonic clonic seizures (GTCs) and very few mild startle myoclonic jerks were reported.
Patients with PMEs are usually refractory to conventional antiepileptic drugs, however few drugs like Topiramate, Clonazepam and Zonisamide have proved their efficacy in the treatment of myoclonic jerks [10].
Our case report addresses the role of VNS in patient with refractory seizures due to PMEs, indeed this role is supported by previously reported cases in the literature [10-12].
VNS implantation has shown significant effectiveness and reduction of seizure frequency mainly of GTCS types, this observation consistent with the findings of other studies [13,14] moreover our patient has significant reduction in myoclonic jerks as well. No clear effect on cerebellar dysfunction.