Rapidly Extensive Chest Wall Sarcoma: Report Case
Primary chest wall sarcomas are uncommon in clinical practices. Therefore, a limited number of studies are published examining the outcomes and efficiencies of surgical, medical, and radiological treatment options to guide the therapeutic approach.
In this paper, we will describe the surgical management of a rapidly extensive chest wall sarcoma.
Keywords:Anxiety; Sarcoma; Chest Wall; Surgery
The occurrence of primary chest wall sarcomas is scarce in clinical practice. Additionally, our knowledge of surgical outcomes is limited to small case series. Every year, 10,600 new cases of sarcoma are diagnosed and only 6% to 10% among them are chest wall sarcomas [1]. Consequently, a small number of studies are published examining the outcomes and efficiencies of surgical, medical, and radiological treatment options to guide the therapeutic approach.
Herein, we describe the surgical management of a rapidly extensive chest wall sarcoma.
This case is about a 60 years old patient with a history of type 2 diabetes for 15 years, who was presented in 2014 with a right-sided chest pain.
The clinical examination found a palpable right chest mass, with presence of inflammatory signs on the skin. The biological assessment was normal, and the chest scan demonstrated a 30*42*21 mm right sided chest wall mass. The tumor extension assessment was negative.
A surgical resection was then performed, and the pathological results that ensued were in favor of a dermatofibrosarcoma with negative margins resection.
After discussion in a multidisciplinary meeting, the patient was referred to the department of radiation oncology for adjuvant radiotherapy and chemotherapy.
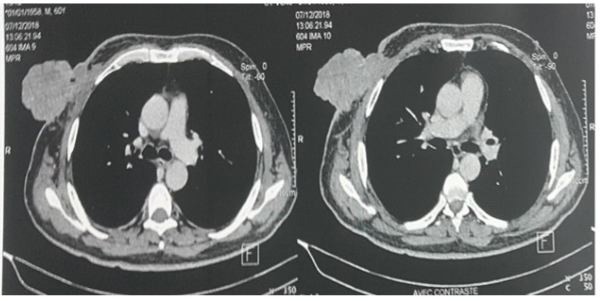
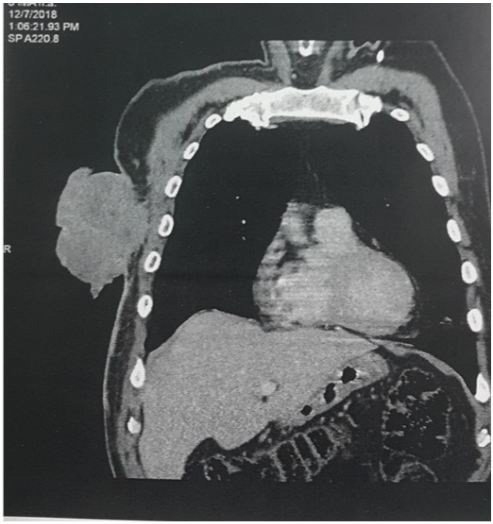
However, 4 years later, a control exam objectified a rapidly larger tumor recurrence in the same site with inflammatory signs and necrosis on the skin (Figure 1). A chest CT demonstrated a 97*71*68 mm tissue mass within the anterior and lateral chest wall with infiltration of the cutaneous tissue, the major pectoralis and tumor infection (Figure 2). This was followed by a tumor extension assessment which was negative.
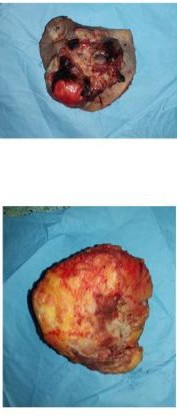
The patient also underwent wide local surgical resection. As a result, the tumor was removed in the surgery block using resection of the clavicular portion of major pectoralis (Figure 3).
The final pathology demonstrated a slightly differentiated sarcoma measuring 10.5* 10 cm. Furthermore, the complementary immune-histo-chemistry report was in favor of a Darier-Ferrand dermatofibrosarcoma with transformation zone of fibrosarcoma.
The patient underwent hyperbaric oxygen therapy (20 session) followed by negative pressure wound therapy for 7 days. Then, he was later called for reconstruction surgery by auto log cutaneous transplant (Figure 4).
Finally, the scare healing was good and a follow up of 20 months is without local recurrence or distant metastasis.
Sarcomas are malignancies arising in connective and supportive tissues. The chest wall contains several different tissues at risk for sarcoma development including fat, muscle, bone, cartilage, and blood vessels.
Primary chest wall tumors are only 1% to 2% of all thoracic neoplasms [2]. They are best classified according to their tissue of origin (bone or soft tissue) and are further subdivided as either benign or bearing malignant potential. Approximately 60% of primary chest wall tumors are malignant, with increasing malignant risk at the extremes of age [2].
The clinical presentation is variable. Thus, it is usually a palpable mass, increasing in size and painful in case of associated bone involvement [3].
The initial evaluation begins with a carful physical examination to exclude other sites of distant disease, to delimit the proximity to vital structures, and to determine the patient’s ability to undergo aggressive therapy.
The most common study on presentation is chest radiography and a computed tomography (CT) scan of the chest. For those lesions in proximity to vital Structures such as the brachial plexus, magnetic resonance imaging is useful to delineate tissue planes and surgical relationships [4].
The primary treatment for sarcomas of soft tissue is complete surgery. It consists of a large excision done in block carrying the Biopsy scar (if performed) and the tumor with a circumferential margin of non-tumoral tissue of 2 cm or an anatomical barrier (resection R0). If the margins are invaded, a surgical re-excision must be made [5]. Radiation therapy has been effective as an adjuvant to surgery for soft-tissue sarcomas of the extremity to decrease local recurrence but does not seem to have an impact on overall survival [6-8].
Our patient underwent both a large resection with an adjuvant radiotherapy and chemotherapy.
For prognostic factors, Patients who had undergone marginal resection had a 3.3 times higher risk of recurrence compared to patients who had undergone wide surgical resection [9]. The risk of distant metastases was closely related to histologic grade. Patients with high-grade soft tissue sarcomas had a 6.5 times higher risk of developing metastases when compared to patients with low-grade tumors [9].
Darier-Ferrand dermatofibrosarcoma of chest wall is rare and requires wide local excision, negative margins, and adequate reconstruction.
Different surgical teams may be required for more complex situations. Early diagnosis of chest wall sarcomas, which confirmation is done by an experienced sarcoma pathologist and undergo a multidisciplinary discussion before treatment initiation, are all required for optimal and successful therapy.