Role of Remote Monitoring in the Detection of Electromagnetic Interference, a Case Report of Two Patients with Implantable Cardioverter Defibrillators
The monitoring of implantable Cardioverter-defibrillators is important in early recognition of device problems. Over the last decades, the number of patients with these devices has increased exponentially and remote monitoring systems are widely used. These deliver alerts via wireless remote monitoring, so that health professionals can respond rapidly. Therefore, safe surveillance is effective in detecting potential problems, such as electromagnetic interference, lead malfunctioning, or atrial tachyarrhythmia’s, which could lead to inappropriate defibrillators shocks. Hence, remote monitoring has the potential to offer improved patient safety and quality of care.
We report on two patients with an implantable Cardioverter-defibrillator, in whom early recognition of electromagnetic interference was possible thanks to remote monitoring, so that an early diagnosis could be made, and further consequences avoided.
Keywords and List of Abbreviations: ICD: Implantable Cardioverter-Defibrillator; EMI: Electromagnetic Interference; VF: Ventricular Fibrillation; EGM: Intracardiac Electro GramCase
Remote monitoring of implantable Cardioverter-defibrillators (ICDs) has been shown to reduce inappropriate shocks and to shorten the time to event detection and clinical decision [1]. In addition, in some but not all studies a reduction in cardiovascular or overall mortality rate have also been observed [2,3]. To reduce the occurrence of inappropriate shocks, early detection of atrial tachyarrhythmia’s and of device/lead malfunctioning are essential. Although less common, early detection and avoidance of electromagnetic interference (EMI) is important.
In our centre all patients with an ICD are offered to have remote home monitoring follow-up. Device interrogation is performed every night via wireless technology, and an alert is sent in case of any malfunction. This information is accessible to health professionals, who can thereby evaluate if any action is required.
We present two cases of EMI in patients with an ICD, in which remote monitoring contributed to early detection and may have avoided further complications.
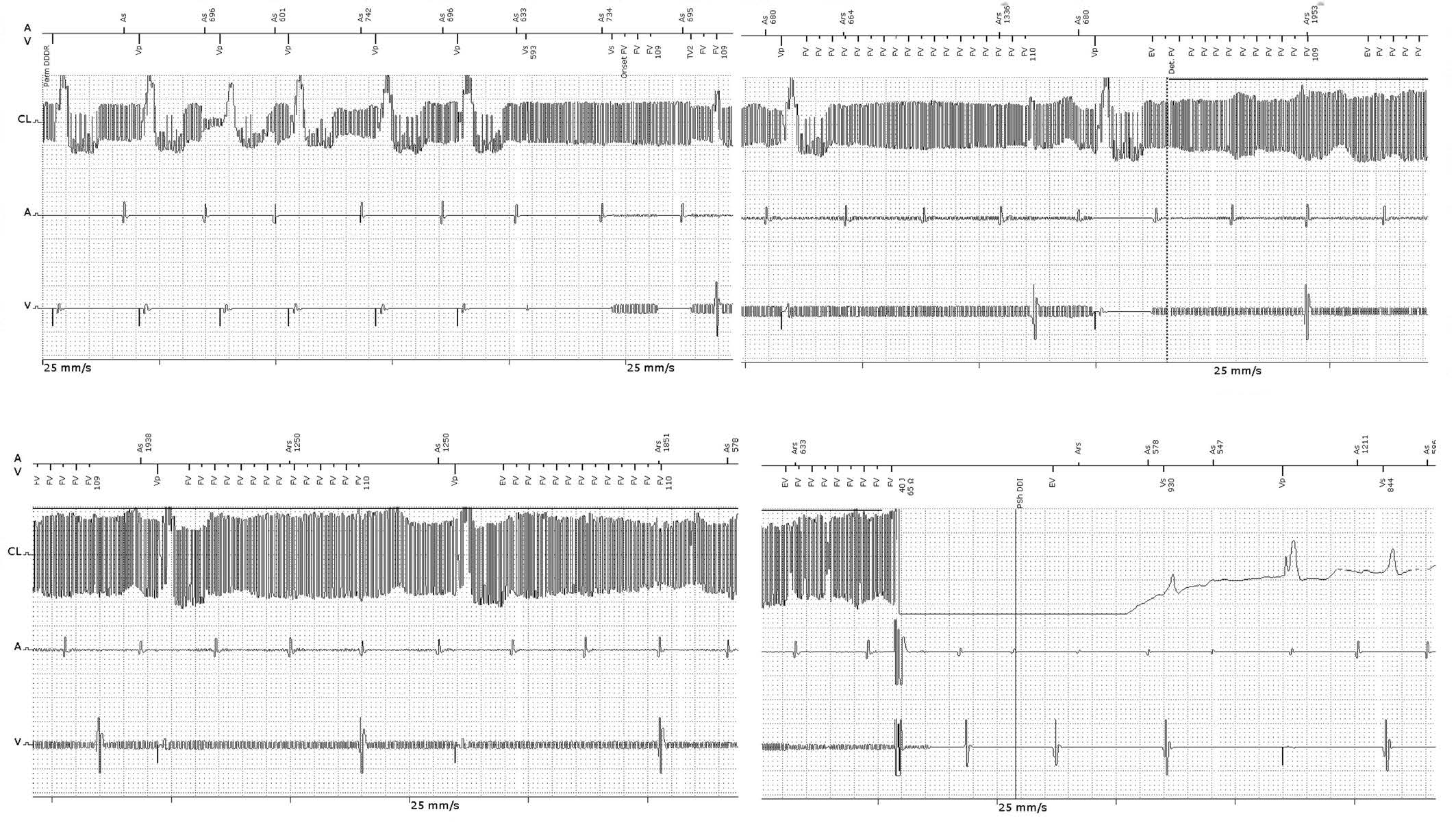
A 78-year-old male, with non-ischaemic dilated cardiomyopathy and depressed left ventricular ejection fraction suffered a cardiac arrest in 2015 due to ventricular tachycardia. He was resuscitated, admitted to a coronary care unit and treated with therapeutic hypothermia. After complete recovery, a dual-chamber ICD (Iforia 3 DR-T, Biotronik, SE&Co. KG) was implanted, and the patient was enrolled in remote monitoring. Because of narrow QRS, cardiac resynchronization therapy was not indicated. At discharge, beta-blocker therapy was started and heart failure treatment was optimized. No arrhythmia episodes were documented during follow-up. The patient was continuously monitored via the Biotronik Home-Monitoring system®. In January 2017, the cardiologist in charge received an alert of ventricular fibrillation (VF), which was treated with a shock. Analysis of the stored Intracardiac Electro grams (EGMs) of the episode, showed a typical pattern of EMI, with high-frequency signals in the atrial and ventricular channels, interpreted as VF, and resulting in one shock Figure 1
The patient was contacted and interviewed about the episode. He felt an electric shock when touching the water tap in the kitchen, but was not aware of having received a real discharge from the ICD. Some days before, a relative, who was not a professional electrician, had been working on renewing his home’s electrical wiring. We urged the patient to contact a licensed electrician to check the whole electrical installation. A ground fault was detected and corrected.
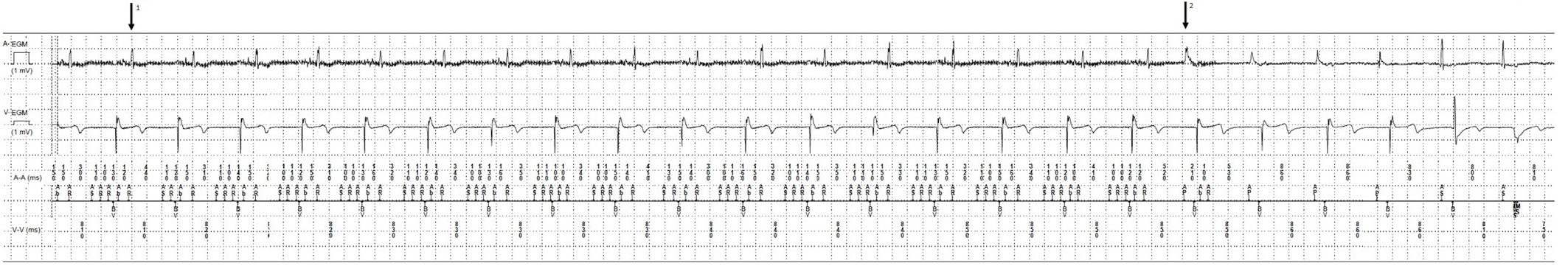
A 61-year-old woman with non-ischaemic dilated cardiomyopathy, left ventricular ejection fraction of 22%, left bundle branch block and symptomatic heart failure, received a cardiac resynchronization device with ICD (Brava Quad CRT-D, Medtronic, Minneapolis, MN, USA) in October 2015. She was offered enrolment into remote monitoring. During follow-up, an improvement in symptoms and left ventricular function was observed. Four months post-implant, T-wave over sensing was detected.
Ventricular sensitivity was reduced to 0.6 mV (nominal 0.3 mV), and the problem was corrected. Atrial sensitivity remained unchanged at 0.3 mV. No arrhythmias were detected since the implant. One year later, an alert was received from Carelink® due to an episode of atrial tachyarrhythmia causing mode switch. When reviewing the episode, high-frequency signals typical of EMI could be seen in both channels but were sensed only by the atrial lead. As ventricular sensitivity had been previously programmed lower, this fact probably precluded sensing of noise, and consequently avoided an inappropriate ICD shock Figure 2.
The patient remembered that on the day of this event, she had done some garden work and helped her husband while he was using an electric saw. She had not perceived any abnormal sensation. We advised her to avoid the electrical device and to ensure that it was functioning properly. Since then, no more alerts have been received.
Appropriate and inappropriate ICD shocks are known to increase mortality and worsen quality of life, which is why early detection of abnormalities leading to them is essential. Atrial arrhythmias, including sinus tachycardia, lead malfunctioning, T-wave over sensing and EMI are the most common causes of inappropriate shocks. Remote monitoring of patients with cardiac implantable electronic devices has an important role in early recognition and in solving many of these abnormalities. In a recent meta-analysis remote monitoring reduced inappropriate ICD shocks and decreased time to event detection and clinical decision [1]. The effect of remote monitoring on overall and cardiovascular mortality is less well established, but it has been suggested that a higher level of adherence to remote monitoring may imply an improvement in survival rates [4].
According to current guidelines, all patients on complex cardiac implantable electrical devices are recommended to have remote monitoring, besides in office visits. In our health system, the remote monitoring transmitters and full framework are provided by devices manufacturers. Reimbursement for remote monitoring is similar to that offered for standard follow-up visits.
In spite of advances in device engineering, with continuous improvements in shielding of devices and signal filtering, as well as new algorithms that improve discrimination, patients with an ICD may be exposed to a variety of potential sources of EMI [5]. Many of them are found in the hospital and health-care environment, such as magnetic resonance imaging, cardio version, radiofrequency ablation, electro cautery, radiation therapy, lithotripsy and transcutaneous nerve stimulation, among others. Fortunately, these potential interferences are easily avoided because patients and hospital staff are usually aware of them. But potential sources of interference are also present in daily life. Widespread and increasing use of wireless technology and gadgets that produce electromagnetic signals represents a challenge to the normal functioning of cardiac devices [6]. Mobile phones, due to their ubiquitous use, are the most common potential source of EMI. However, their normal use is safe for patients with implanted cardiac devices if certain sensible recommendations are followed. Airport security systems, both hand-held and walk-through, and electronic article surveillance devices that are commonly used by retailers, deliver electromagnetic waves that can interfere with normal device function. Patients must be informed about potential risks and the need to avoid prolonged exposure to these fields. Items with magnetic properties, such as some used in headphones, jewellery or clothes, are also potential sources of interference, especially when placed very close to the device; patients should also be advised to use these judiciously.
Household appliances are not a source of EMI if they are functioning properly. Technical issues or improper grounding of electric devices and wiring have been reported as causes of inappropriate ICD shocks [7,8].
In our two cases, the patients were not aware of the presence of an EMI resulting in device malfunctioning. However, appropriate corrective measures were undertaken thanks to the alerts and the information obtained from remote monitoring. These early diagnoses probably avoided further complications.