Severe Hypoglycemic Coma Event on MRI: Specific Brain Necrosis
With the widespread of sale and use of oral hypoglycemic drugs or insulin, hypoglycemic coma event have become a common medical emergency. Some patients with severe hypoglycemic coma led to prolonged hypoglycemia with fatal coma due to delay in the treatment time [1], or may led to coma, reasons are difficult to assess as the blood sugar have returned to normal levels. Here, we report a case of severe hypoglycemic coma events, blood sugar level has returned to normal and its brain MRI changes.
Keywords: Hypoglycemic; Brain Necrosis; MRI
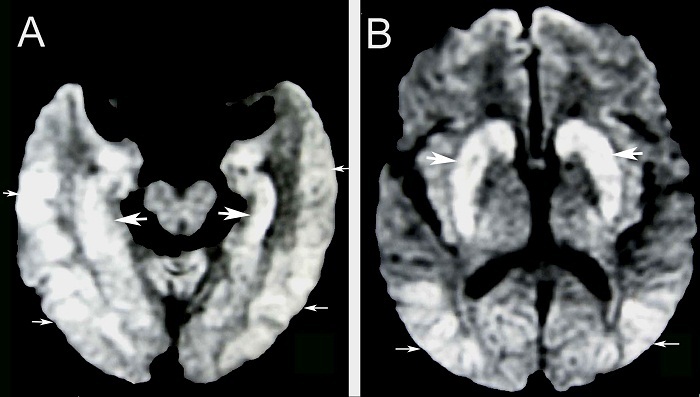
A 76-year-old woman with hypertension was in coma for 48 hrs, and its bed is exposed to anti-diabetic drugs, i.e., glibenclamide 100 tables/bottle leaving only 90 tables (2.5mg /piece). The patient had no exposure to carbon monoxide, and no history of diabetes mellitus and cardiac arrest. She used to live alone, the patient was unconscious for two days, only then discovered she fell ill, and then she was given 50 ml of sugar water oral. Unfortunately, the patient remained in a coma. Brain CT scans were normal. Blood pressure was 153/92mmHg.The respiratory rate and SpO2 were normal. She had a Glasgow coma score (GCS) of E1M4V1 with symmetry pupils (diameter 1.5mm), no light reflex, corneal reflex, and extraocular movements. On admission, laboratory blood glucose was 8.6 mmol/l. Electrolytes, liver and renal function was normal. ECG revealed normal. On the second day of hospital admission, brain DWI revealed diffuse high signals on the cerebral cortex bilaterally, hippocampus, and basal ganglia (Figure 1A and B). After four days of admission, the patient was still in deep coma and phlegm, so the tracheotomy breathing was performed. After five days, the patient was into a vegetative state, and she was discharged after 21 days. On follow-up 2 months later, the patient was a persistent vegetative state.
Hypoglycemic coma has become a common medical emergency, it is not only a common complication of diabetes due to widely available for use of oral hypoglycemic agents or insulin, but also can be a cause of mistake or even suicide. Some serious hypoglycemic patients often delay in treatment time led to irreversible coma [1] or because the half-life of hypoglycemic agents is past, and the blood sugar has been returned to normal levels, leading to coma reasons difficult to assess or misdiagnosed.
The patient shows neither signs of cardiac arrest, nor a history of exposure to carbon monoxide, so the whole brain anoxic and hypoxic-ischemic encephalopathy can be excluded. In general, if the cerebral circulation is stopped (more than 5 minutes), ischemia and hypoxia, can produce localized neuronal apoptosis and necrosis. It is difficult to fully recover in 6h. Cerebral ischemia may be focal or global. If patient was in cerebral ischemia, MR imaging showed that the global ischemia is usually in the gray matter junctions [2] whereas focal infarctions is in regions between major arterial territories [3]. Moreover, infarction is almost multiple asymmetric (different sizes), and also with the characteristics of gray matter involvement. Although infarctions in the bilateral basal ganglia is not uncommon, but it is asymmetry, and also in other vascular territory, including the brain’s white matter areas, often with ischemic lesions, which may be termed “satellite lesions”. Thus, the current MR image change is not used a global ischemic or focal infarction to explain.
Predominantly gray matter damage is termed “selective neuronal necrosis” [4]. Our patient’s DWI showed only a symmetrical gray matter injury, including bilateral temporal occipital cortex, basal ganglia, and hippocampus; whereas white matter not be affected. This selective neuronal necrosis in the gray of brain on DWI is a specific feature hypoglycemic brain injury [5,6]. However, glucose deprivation is different than the cerebral circulation stops. Coma can occur at glucose levels in the range of 2.3–2.7 mmol/l [7]. Experiments confirmed that some of the neuronal apoptosis can occur after hypoglycemic coma lasting 30 minutes [8], whereas glucose levels in the range of 1.7-1.9 mmol/l can lead to a prolonged coma due to irreversible neuronal death. In studies of insulin-induced hypoglycemia in monkeys, 5–6 hours of blood glucose concentrations of less than 1.1mmol/L were required for the regular production of neurological damage [9]. Profound, prolonged hypoglycemia can cause brain death [8]. It can be seen, the irreversible of brain injury is associated with the severity and duration of hypoglycemia coma [10]. Thus, delayed correction of plasma glucose concentration does not interrupt this cell death process. Therefore, the monitoring of the brain MR image is useful for the diagnosis of coma [9,11]. Our patient was an old woman lived alone and with a history of exposure to glibenclamide (half-life of 12 hours). She was conscious for two days when discovered she fell ill, and she was given oral 50ml of glucose water before admission.On admission, although her blood glucose was 8.6mmol/l, her prolonged coma was a performance of severe hypoglycemic brain lesion. Moreover, this specific high signals in the bilateral cerebral cortex and hippocampus, and especially in bilateral basal ganglia due to severe hypoglycemic event has been confirmed by our MR-DWI.
On other hand, the analysis of the brain MR image’ changes after a hypoglycemia coma can be useful to predict the prognosis. For instance, some prolonged hypoglycemia coma associated with lesions of the internal capsule, corona radiata and cortex have been reversed by raising glucose [12-14]. Lesions of the bilateral basal ganglia may survive in a persistent vegetative state, [5,6] even with a poor outcome and death [13,15].
According to the diagnostic criteria of persistent vegetative state published by the American Academy of Neurology in 1995, three months later, the patient with a persistent vegetative state has been diagnosed. This suggests that these high signals on DWI from severe hypoglycemia due to the mistake of overdose hypoglycemic drugs lead to irreversible neuronal necrosis or death. Patient could be misdiagnosed if blood glucose was returned to a normal level due to the half-life of hypoglycemic drugs absented. Therefore, we recommend that comatose patient who showed the specific high signals in the gray of brain on DWI, should be the evidence of diagnosed severe hypoglycemic coma.