Small Intestinal Amyloidosis: A Case Report
Background: We present a rare case of gastrointestinal amyloidosis. The diagnosis of this disease is not always easy and quick. The aim of the case report is to remind this orphan disease in the differential diagnosis.
Case Presentation: A 54-yrs-old woman with a 2 years’ history of asthenia, weight loss and abdominal distension without diagnosis. After specific laboratory tests, Computed Tomography (CT) scan, endoscopies and biopsies we made diagnosis of multiple mieloma and amyloidosis that involved gastrointestinal tract and lung too. So we described a rare case of gastrointestinal (GI) amyloidosis.
Conclusions: The key message of the case report is to consider amyloidosis in the differential diagnosis when a patient presents gastrointestinal symptoms.
Keywords: Gastro-intestinal amyloidosis; Multiple mieloma; uncommon disease; abdominal pain; Congo red staining
Amyloidosis is a broad term used for a group of uncommon disorders that cause structural and functional organ dysfunction with anomalous extracellular deposition of abnormally-folded peptide derivatives [1]. Amyloidosis is a disease that can present with systemic or localised organ involvement. Primary and secondary amyloidosis are the more frequently encountered systemic subtypes. Primary or amyloid light chain (AL) amyloidosis mostly occurs as a stand-alone disorder or in association with multiple myeloma (MM), with the deposited fibrils composed of immunoglobulin light-chain subunits. Secondary (AA) amy loidosis results from chronic inflammatory processes that increase the levels of acute-phase reactant, serum amyloid A (SAA), with the deposited fibrils comprising SAA subunits. Furthermore, dialysis-related disease, heritable and senile amyloidosis are other systemic subtypes. Organs that may be affected include the heart, kidneys, liver, spleen, nervous system and digestive tract. Signs and symptoms of amyloidosis are evident when the condition is advanced; they depend on which of organs are affected.They may include: severe fatigue and weakness, shortness of breath ,swelling of ankles and legs, edema, diarrhea, possibly with blood, or constipation, unintentional weight loss,enlarged tongue,skin changes like thickening or easy bruising,purplish patches around the eyes, irregular heartbeat. [2, 3]
We present here a case of multiple myeloma-associated AL amyloidosis with symptomatic small intestinal involvement, which is an extremely rare clinical entity [4]. Symptomatic amyloidosis involving GI tract is a rare, diverse and a difficult condition, it can be confused with other GI conditions also gastric cancer. [5] A mucosal biopsy is necessary for a definitive diagnosis[6-8].
In a case series of 769 patients with biopsy-proven AL amyloidosis, GI disease was noted in 8% only while symptomatic stomach involvement was present in only 1% of the cases [9]. The prognosis of AL amyloidosis involving the stomach and small intestine is largely dependent on the underlying aetiology and the nature, number, and extent of the organ involvement.
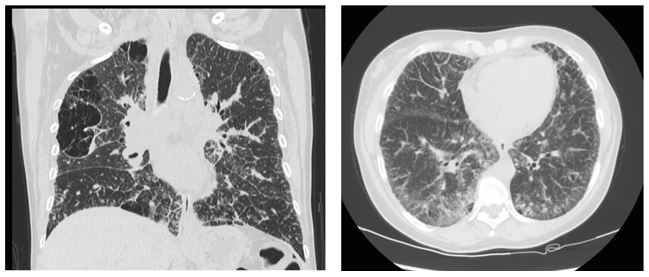
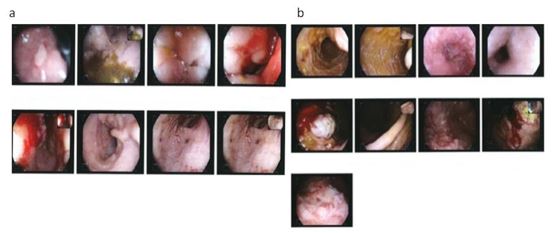
The gastointestinal tract can be affected by different types of amyloidosis accumulation (AA, ATTR, β2-microglobulin and α2-microglobulin in patients which are doing long-term dyalisis) at any age and at any anatomic site. Generally, it is asymptomatic, but it may present clinically with ulcers, mobility disorders, ddysphagia, rectal bleeding, hemorrhage areas on the mucosal surface or as a pseudotumor mass [10-12]. In this case a lower and an upper gastrointestinal endoscopies show:diffuse congestion and thickening of the small and large intestine as showed in figure 1.
Amyloidosis deposits in the colorectal tract following two different accumulation patterns: vascular and gastrointestinal; in the figure 2a we can see that in H&E (Hematoxylin and Eosin) sections these gastrointestinal stores appear as pink and hyalinized tissue infiltrate, respectively and submucosal deposits.
Amyloid angiopathy has been described in a variety of vessels. Three forms involving the media, intima, and adventitia have been described. Unfortunately, due to the non-specific clinical presentation, amyloidosis symptoms and signs are often misinterpreted. Fatigue, purpura, petechiae, mucosal hemorrages,anemia can be associated to other disease. For these reasons diagnosis of amyloidosis requires a multidisciplinary approach and should be confirmed by Congo red staining in polarised light of a tissue sample as we made in our case report. In fact, figure 2b and 2c confirm amyloidosis with the tipycal apple-gree birefringence consistent with amiloyd deposits.
Gastrointestinal amyloidosis must be distinguished from other storage disorders such as Collagenous Colitis, Thick base- ment membrane and Radiation Colitis using the patient clinical history, the symptoms, the signs, the etiology, their different histological arrangement, and last but not least, ancillary studies such as special stain (Congo red stain, Tri-chrome stain, etc.) and immunohistochemistry (ex. CD3). Immunohistochemistry should be also used to define the pro- tein fibril type because it is of diagnostic, prognostic, and therapeutic importance.
We present here a case of multiple myeloma-associated AL amyloidosis with symptomatic small intestinal involvement.
A 54-yr-old woman presented to our hospital with a 2 yr history of asthenia, weight loss, and abdominal distension. In history only diagnosis of sarcoidosis, evidenced from a chest CT and a transbronchial biopsy. At a physical examination she presented a soft, round, bloated abdomen but intestinal sounds were normal. Laboratory testing revealed anaemia, elevation of platelets and hypoalbuminemia. An immunofixation urine test showed kappa free light chains, whereas serum protein electrophoresis revealed elevated free kappa light chains, low free lambda light chains and elevated kappa/lambda ratio. A chest and abdomen CT showed multiple lymphadenopathies. An upper (Figure 1a) and lower (Figure 1b) gastrointestinal endoscopies were performed and showed diffuse congestion and thickening of the small and large intes- tine. Intestinal biopsies evidenced the presence of extracellular matrix deposition which corresponded to amyloid (Figure 2a-2b-2c). A bone marrow aspiration showed an increased cellularity with 30-40% plasma cells. On the basis of these results we made diagnosis of multiple mieloma and amyloidosis which involved gastrointestinal tract. On this basis we considered chest granulomas and lung interstitiopathy (Figure 3) lung manifestation of amyloidosis and not a sign of sar- coidosis.
Immediately a first-line chemotherapy was started with Dexamethasone, Cyclophosfamide and Bortezomib. A supportive therapy was used for the management of pain, aenemia and gastro-intestinal symptoms. There was not a good response to first line chemotherapy so a second line chemotherapy was started with Bendamustine. Also this therapy did not resul well infact: kappa/lambda ratio continued to increase and there was no improvement of GI symptoms. The patient con- tinued to have an important nausea, asthenia, abdominal distension and symptoms of malabsorption.
During the recovery she had a stroke an CT brain showed cortical and subcortical areas of hypo density that involved the frontal operculum and the caudate nucleus. Doppler Ultrasonography showed the presence of endoluminal thrombosis obstructing the right carotid bifurcation. Because of pro-hemmoragic conditions related to Amyloidosis and Multiple Mieloma the patient was not a candidate for fibrinolysis.
She died after 3 months from the recovery for a Candida Albicans sepsis .
We describe a rare manifestation of amyloidosis with intestinal and pulmonary involvement. The diagnosis of this disease is not always easy and quick. It is therefore recommended to remind this orphan disease in the differential diagnosis.
AL amyloidosis causing GI disease has a poor long-term prognosis (median survival: 4-6 months) when detected at an advanced stage, with cardiac disease, renal dysfunction and infection being the major causes of death, as happened in this case report.
In case of abdominal distension, malabsorption, asthenia or lung interstitiopathy rarely amiloydosis is considered in dif- ferential diagnosis, so the treatment is delayed. So the key message of the case report is to consider amyloidosis in the differential diagnosis when a patient presents GI symptoms.
Conflict of Interest: The authors declare that they have no conflict of interest.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5).

.JPG)
.JPG)
.JPG)