Sociodemographic Characteristics of Obstetric Patients in the Intensive Care Unit in San Luis Potosí, Mexico
Introduction: Pregnancy is a natural state in a woman’s life; however, it can be accompanied by complications which may conclude in maternal death or in the development of morbidity. Worldwide, a health complication during pregnancy, childbirth and puerperium is 18% of the global diseases in women.
Objective: To identify the sociodemographic characteristics, diagnosis of admission and discharge of the obstetric patients in the ICU) of Instituto Mexicano del Seguro Social No.1 in San Luis Potosi, from January 1 to December 31, 2014.
Materials and Methods: Descriptive, transversal, retrolective study. A total sample of 52 patients, selected for consecutive cases, not probabilistically. Subsequently, a descriptive analysis was carried out where the results were graphed, and presented as frequencies in addition to Fisher’s test and Odds Ratio for the corresponding variables.
Results: We studied 52 patients admitted to the ICU from 18 to 41 years old with an average age of 27.7 years. It was found lack of complete education. The diagnoses found were 67.9% with hypertensive disorders, within hypertensive disorders, Severe Preeclampsia was found with 59.6%, mild preeclampsia 5.8%, and 3.8% with HELLP syndrome. However, when calculating the Odds ratio between the two groups for this relationship we find 0.44 with a confidence interval of 0.13 to 1.48. There were 28.3% with the diagnosis of obstetric hemorrhage due to uterine atony and 3.9% with sepsis whose causes included surgical wound infection and urinary tract infection, treated mostly with ceftriaxone.
Conclusion: The risk factors must be treated immediately for preventive measures such as close monitoring of blood pressure, obesity and urinary tract infections, these being those that most appeared in the patients admitted to the ICU.
Keywords: Sociodemographic characteristics; Obstetric patients; Intensive Care Unit
Pregnancy is a natural state in a woman’s life; however, it can be accompanied by complications, which may conclude in maternal death or in the development of morbidity [1]. Worldwide, health complications during pregnancy, childbirth and puerperium generate 18% of the global diseases in women between 15 and 44 years.
In these patients, 71% of the admissions to the ICU (Intense Care Unit) are generated by obstetric complications. The main pathologies that cause the admission of pregnant patients to this type of services are the hypertensive disorders of pregnancy and obstetric hemorrhage, followed by infectious processes, among other states of cardiovascular, hemodynamic and ventilatory compromise. It should be noted that more than half of these patients are admitted to this service during the postpartum period. Likewise, they require this level of care due to non-obstetric causes up to 20 to 30% of the income [2].
This condition can generate complications and require critical management in up to 10% of cases, exceeding in developing countries. It has been found that some Para clinical findings, such as elevation in proteinuria, act as predictors of some of these complications, so their presence could act as a good criterion for transfer to the ICU. In most of the studies carried out to date, preeclampsia and its complications represent the most frequent causes of transfer to the ICU, reaching up to 40% of these admissions [3,4].
Another of the pathologies that most frequently generate hospitalizations related to pregnancy in the ICU is obstetric hemorrhage secondary to uterine atony, which is usually associated with consumption coagulopathy, being the second cause in Latin America. It should be noted that, among the deceased patients, this diagnosis is the most frequent. This eventuality is related to greater morbidity when there is placental retention, multiple pregnancy, macrosomia, episiotomy and suture use [5].
To date, anemic states, history of this type of hemorrhage, induction and prolongation of labor have been identified as the main risk factors; however, its predictive power is still very limited, reaching between 7 and 10% of cases. Even in developed regions, from 60%, in the United Kingdom and the Netherlands, up to 90%, in France, maternal deaths are caused by obstetric hemorrhages, related to non-optimal prenatal care [6,7].
Although they are less frequent than the mentioned pathologies, infectious complications imply one of the greatest risks to life. In Latin America, severe sepsis and septic shock continue to represent a high proportion of obstetric patients admitted to the ICU despite being preventable through an adequate control of precipitating factors and the existence of adequate therapeutic options if it is detected early [8,9].
Despite the incorporation of newer antimicrobial agents and improvements in life support measures, these states are associated with a mortality of up to 28%. These patients should be assessed by a multidisciplinary team, and if there is a possible Septic focus, it must be removed upon identification, without delay, therefore avoiding the impossibility of reversing septic shock [10].
Both mortality and maternal morbidity are indicators that if taken together, can allow the identification of the triggers that generate these problems, if they are adequately studied. Up to 80% of maternal deaths can be potentially avoided by a series of interventions, most of which are feasible in countries of very different levels of development, beside the failure in the identification of cases that require critical care and lack of experience in the intensive management of pregnant patients [11-13].
Due to the little existing literature about the causes of admission of pregnant patients, their characteristics, their conditions, and time of stay in the ICU. In San Luis Potosí no similar study has been carried out, therefore with an objective knowledge of all these data, specific and effective strategies can be established to seek to target these risk factors of the concurrent pathologies, generating a reduction of them and diminishing the maternal morbidity and mortality.
The objective was to determine the sociodemographic and diagnostic characteristics of admission and discharge of obstetric patients who have required admission and management in the ICU of the Hospital General Zona No. 01 of the Instituto Mexicano del Seguro Social in San Luis Potosí, Mexico from January 1 to December 31, 2014.
A Descriptive, Transversal and Retrospective Study was carried out in the Instituto Mexicano del Seguro Social in the state of San Luis Potosí, a hospital of second level of care with ICU since 1980 with a total number of 4 beds. The total staff in all shifts in ICU was the following: Number of intensivists 18, Obstetric Gynecologist specialists 0 and intensivists nurses 18.
From January 1 to December 31, 2014 the total number of admissions were 64 patients in ICU with a total sample of 52 pregnant patients for consecutive cases representing the 81% of the total of the patients. Cases of patients admitted to the ICU in charge of the gynecology and obstetrics service with diagnosis to pregnancy or puerperium were included and those unrelated to the pathologies mentioned were excluded. Those who did not have complete data for the collection of information were eliminated.
This study complies with the recommendations and guidelines of the Declaration of Helsinki, as well as the General Health Law of Mexico. According to the General Law on Health in the field of Research, published in the Official Gazette of the Federation on January 6, 1987, within the section entitled “On the ethical aspects of research in human beings”, in its article 17, This study is classified as Class I, without risk with the registration number: R-2015-2402-15 approved by the ethics committee.
We identified the sociodemographic characteristics and diagnosis of admission and discharge of obstetric patients and subsequently emptied the information into a data sheet in Excel 2016, and a descriptive analysis was carried out. The results were graphed and presented as frequencies. In addition to the Fisher test and odds ratio for the corresponding variables.
We studied 52 beneficiaries being the 81% of total admitted to the ICU of Hospital General Zona N° 1, Instituto Mexicano delSeguro Social in San Luis Potosí, during the period from January 1 to December 31 of the year 2014. The distribution of the results of the General characteristics of population are shown in (Table 1).
It was found that 30.2% corresponding to 16 patients were registered in the clinical history 4 or less prenatal consultations, however, in the registry, 43.4% were found with a total of 23 patients with the same number of consultations, while that the 69.8% corresponding to 37 patients had 5 or more consultations, in the registry it was found that the 56.6% corresponding to 30 patients.
The occupation most found was housework with 54.7% corresponding to 29 patients, secondly 32.1% corresponding to 17 patients were employee, and finally 13.2% corresponding to 7 patients were operator.
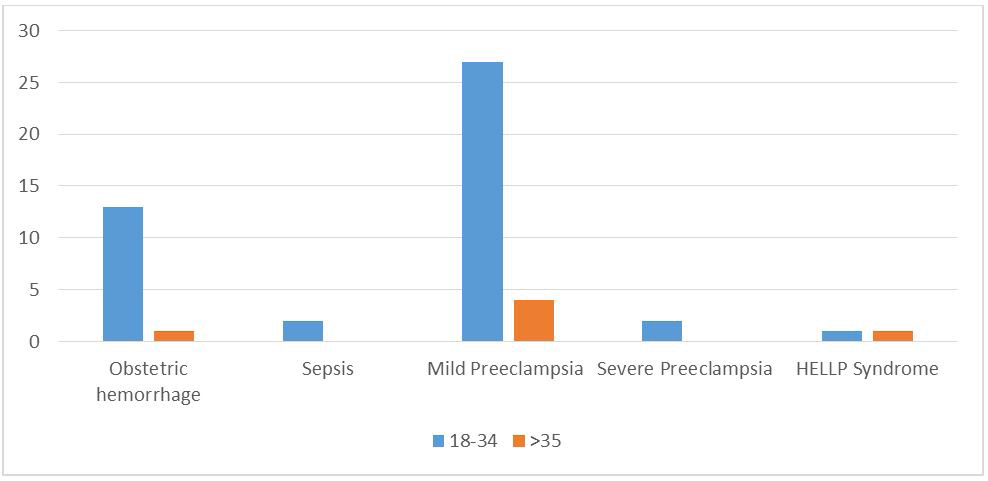
The diagnoses found were 67.9% with 35 patients for hypertensive disorders, 28.3% with 14 patients due to obstetric hemorrhage and 3.9% with 2 patients with a diagnosis of sepsis. Finally, with 2 patients for HELLP syndrome with 3.8%. Frequency by age group is shown in (Figure 1).
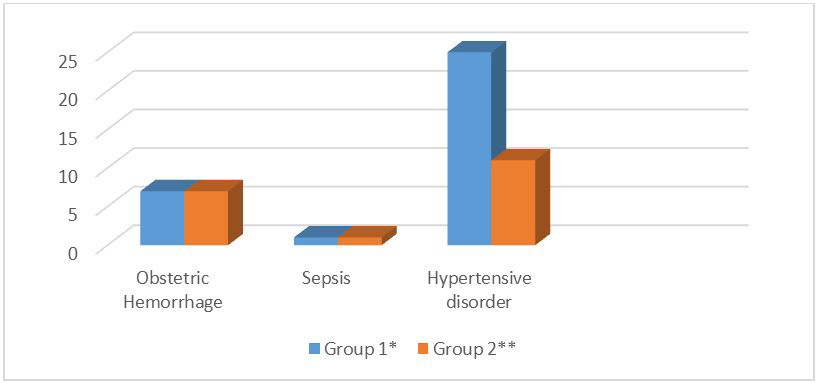
When comparing the results of the, we observed that the only difference was in the hypertensive disorders of pregnancy between group 1 and group 2 (Figure 2).
However, when calculating the Odds ratio for this relationship we found 0.44 with confidence interval of 0.13 to 1.48. It was found that the second cause was hemorrhage in the 14 patients was uterine atony, the minimum age was 18 years, maximum of 41 years, with a mean of 27.7 and a standard deviation of 5.90.
Among the most frequent antihypertensive medications we found hydralazine with 32.7% on 32 occasions, continued by nifedipine with 29.6% on 29 occasions, alpha-methyldopa with 14.3% on 14 occasions, metoprolol with 8.2% on 8 occasions, enalapril with 4.1% on 4 occasions, furosemide and losartan with 1% on 1 occasion each.
There were a total of 2 patients with a diagnosis of sepsis being the causes of infection: infection of surgical wound and urinary tract infection, and the use of antibiotics was ceftriaxone in 50%, amikacin in 25% and clindamycin in 25%.
If we make a comparison with the studies found in Mexico at the Centro Nacional La Raza it was found that the average age of mothers’ income was 28.1 ± 5.9 years. In the results of our study we found that the age of admission was found in 25 to 35 years of age with 55%, but important figures in the range of 18 to 24 years with 34%. In our study the range of 18 to 24 years also has to be under strict surveillance because of the high percentage of frequency [14].
In the series reported here, the frequency of obesity with the mothers who entered was high with 55% with a BMI (Body Mass Index) > 30, which implies an increase in the risk of maternal and fetal complications in morbidity and mortality. As mentioned in New York in 2007, it was observed that obesity with BMI> 29 increases 3-fold the risk of maternal morbidity and mortality (3.0, 1.7 to 5.3) [15].
In prenatal control we can see the importance in a study conducted in Colombia in 2015, finding inadequate follow-up in weight control (OR 5.12: 95% CI 1.33-19.65), blood pressure (OR 5.18, 95% CI 1.40 -19.12), iron supplementation (OR 1.73, 95% CI 1.19-3.68), laboratory uptake (OR 2.19, 95% CI 1.11-4.42), an increase in maternal and fetal morbidity and mortality. In the results of our study, despite having 56.6% of patients with 5 or more prenatal visits, they required admission to the ICU, so the characteristics of each prenatal visit should be evaluated [16].
In a study of maternal deaths in Mexico, it was found that maternal education had a level below secondary school at 45.66% and 79.19% were housewives. In our study, we found 39.4% with completed secondary school and 54.7% with house work. It is important to highlight that its members revolve around that nuclear figure, whose absence usually leads to the disintegration of the family. It should be mentioned that in our results the association of risk with schooling was obtained an OR of 0.44 with an interval of confidence of 0.13 to 1.48 which we attribute possibly to the size of the sample [17].
In Chile in 2016, the principal cause of admission to the ICU was hypertension with 53%, followed by infections 23.27% and hemorrhages with 13.79%. In our study we found hypertensive disorders with 67.9%, obstetric hemorrhages with 28.30% and sepsis 3.8%. Hypertensive disorders remain the leading cause of maternal morbidity similar as described in the literature.
Hemorrhage and infections continue taking place as important causes of admission to the ICU, therefore physicians should continue to be trained in their prompt detection and correct response [18].
In Mexico it was found that 65.5% had obstetric hemorrhage as the main cause of admission, from 30 to 39 years, with the following causes: caesarean section, placental accreta and uterine atony. In our study it was found that 28.3% admission due to obstetric hemorrhage secondary to uterine atony, even though the age was from 18 to 41 years, the gestation was from 33.4 to 40.2 weeks.
In other study realized in Mexico, it was found that the main causes of infection were urinary tract infection with 41.6%, deciduitis with 25%, surgical wound infection with 16.7% and pneumonia with 16.7%. In our results, 3.8% of admitted to the ICU had sepsis, 50% due to infection of the urinary tract and infection of the surgical wound, respectively, the use of antibiotics was with ceftriaxone in 50%, amikacin 25% and clindamycin 25% [19].
In a study realized in Argentina taking into account the drugs used in hypertensive disorders, it was found that 33% used alpha-methyldopa, 31% magnesium sulfate, 19% clonidine and 9.5% amlodipine, 4.8% furosemide and 2.4% labetalol [20]. In our study was the most used was hydralazine with 32.7%, following with nifedipine in 29.6%, alpha methyldopa in 14.3%, metoprolol 8.2%, enalapril 4.1%, furosemide 1% and losartan 1%.
Currently there are multiple antihypertensive drugs available that could be used in the treatment of hypertensive disorders of pregnancy. Nifedipine is recommended in the use of preeclampsia in our study it was the second most used drug. With the rest of the medicines their use depended in each particular case and according to the evolution of the patients.
Our findings are similar with previous study, which we found the same three causes in these obstetric patients, nevertheless, the obstetric hemorrhage was the second cause, having a clear impact because in the hospital where the study took place, they created an immediate response team in 2010 to offer a major quality of obstetric care.
The population studied cannot be generalized to the entire population opened by geographical location, in addition to the fact that they differ from the health institutions where medical attention was provided, being two important limitations in this study. While its strength, is that it confirms the global scenario of causes of maternal mortality, thus being able to identify obstetric patients with risk factors, having a diagnosis and early treatment, decreasing maternal mortality.
For later studies, it is recommended to carry out a broader, comparative study where all the risk factors could be detected to amplify a preventive medicine and the creation of an immediate response time to achieve a greater impact in the reduction of maternal mortality.
Sociodemographic characteristics in critically ill obstetric patients should be taken into account as risk factors, since, it diminishes morbidity and mortality of obstetric patients. The risk factors associated to complications that were found in the present investigation should be treated immediately as preventive measures such as close monitoring of blood pressure, reduction of obesity and early diagnosis of urinary tract infections, these being the ones that most appeared in the patients admitted to the ICU.
Hypertensive disorders, obstetric hemorrhages and infections continue to be the most important causes of maternal complications, being essential to have a multidisciplinary team to manage the natural history of the disease and its complications in order to make appropriate and timely decisions.