Study of Association between Celiac Disease and Hepatitis C Infection in Sudanese Patients
Background: It has been hypothesized that non-intestinal inflammatory diseases such as hepatitis C virus (HCV) and hepatitis B virus (HBV) may trigger immunological gluten intolerance in susceptible people. This hypothesis suggests a possible epidemiological link between these diseases.
Method: Third generation enzyme immunoassay (ELISA) for the determination of antibodies to Hepatitis C Virus was used on 69 blood samples of celiac disease seropositive and seronegative patients. Positive and negatives ELISA samples were confirmed using PCR for detection of HCV RNA.
Results: The prevalence of HCV detected in seropositive celiac disease was 2% by serology (ELISA) and 12% using PCR, whereas the prevalence of HCV among seronegative celiac disease patients was 5.2% by serology (ELISA) and by 21% PCR. PCR detected 8 samples out of 69 as positive for HCV RNA which was negative by HCV Ab ELISA.
Conclusion:The results revealed that there was no association between HCV and CD in Khartoum State, Sudan.
Keywords: Celiac Disease; HCV; Sudan
Celiac disease (CD) is a chronic small intestinal immune-mediated enteropathy precipitated by exposure to dietary gluten in genetically predisposed individuals. CD is triggered by the ingestion of gluten, the protein component of wheat, rye and barley. HLA and non-HLA genes together with gluten and possibly additional environmental factors are involved in development of CD [1]. The primary HLA association in the majority of patients is with DQ2 and in a minority of patients with DQ8 [2].
The clinical presentation varies; no typical presentation exists. Some patients are asymptomatic or have only signs of nutritional deficiency. Others have significant GI symptoms. Celiac disease can manifest in infancy and childhood after introduction of cereals into the diet. The child has failure to thrive, apathy, anorexia, pallor, generalized hypotonia, abdominal distention, and muscle wasting. Stools are soft, bulky, clay-colored, and offensive. Older children may present with anemia or failure to grow normally [3].
In adults, lassitude, weakness, and anorexia are most common. Mild and intermittent diarrhea is sometimes the presenting symptom. Steatorrhea (foul-smelling, pale, bulky, and greasy stools) ranges from mild to severe (7 to 50g of fat/day). Some patients have weight loss, rarely enough to become underweight. Anaemia, glossitis, angular stomatitis, and aphthous ulcers are usually seen in these patients [3-5]. Potential consequences of untreated CD include impaired fertility and reduced bone density as well as an increased risk of gastrointestinal malignancy [6].
Hepatitis C Virus (HCV) is an enveloped RNA virus from Flaviridae family and Hepacivirus genus. It has a single positive-strand RNA [7]. HCV is the most common cause of chronic liver diseases. Chronic hepatitis C infection (HCI) is a major health problem that affects 2-3% of global population. Studies of hepatitis C virus in Sudan showed a low seroprevalence of 2.2%-4.8% [8]. Despite the fact that Hepatits B infection has been controlled over the previous years, Hepatitis C infection is still considered the major culprit of chronic liver diseases, and has been identified to cause several manifestations in many diseased categories, such as hemodialysis patients and autoimmune hepatitis patients [9-11]. Although mainly asymptomatic, patient’s infected with HCV usually present with fever, anorexia, nausea, vomiting, jaundice, pale stools and dark urine [12]. HCV is not only a frequent cause of chronic liver diseases such as hepatitis, cirrhosis and hepatocellular carcinoma, but is also involved in the pathogenesis of a number of autoimmune and rheumatic disorders (arthritis, vasculitis, sicca syndrome, porphyria cutanea tarda, lichen planus, nephropathies, thyroid diseases, and lung fibrosis), as well as in the development of B-cell lymphoproliferative diseases [13].
Initial testing for celiac disease includes the measurement of IgA antibody to human recombinant tissue transglutaminase (TTG). Because of the inferior accuracy of the antigliadin antibody tests (AGA), the use of AGA IgA and AGA IgG tests is no longer recommended. It is recommended that confirmation of the diagnosis of CD require an intestinal biopsy in all cases. Because the histologic changes in CD may be patchy, it is recommended that multiple biopsy specimens be obtained from the second or more distal part of the duodenum [3,14]. The diagnosis of HCV infection is made by the detection of antibodies against HCV (anti-HCV) and/or by detecting the presence of the HCV RNA in serum [15].
Seronegative HCV infection refers to the unusual absence of anti-HCV antibodies despite the presence of HCV RNA. This condition is associated with a number of conditions, such as HIV coinfection, but may also be seen in apparently healthy blood donors and other groups.
The association between CD and several liver diseases has long been documented. About 42% of adult CD patients have raised liver enzymes (ALT or/and AST). It has been hypothesized that hepatitis C virus infection might predispose to CD. In fact, several studies have implicated HCV infection in the development of CD [14,16,17].
The immunology department of the Central laboratory is a reference lab for diagnosis of celiac disease. It receives serum samples of patients suspected of Celiac Disease from all the government hospitals in the Khartoum state. The lab uses ELISA.
From a pool of 304 samples with their corresponding records, every 6th sample was chosen to make a total of 50 samples.
Ethical approval from the Federal Ministry of Health regarding data was obtained for collection and examination of serum samples. A total of 69 serum samples (50 CD seropositive, 19 CD seronegative) were obtained from the immunology department of the Central Lab of the Ministry of Higher Education and Scientific Research, Khartoum. The serum was stored at -20°C until use.
Third generation enzyme linked immunoassay (ELISA) for the detection of IgA autoantibodies against tissue transglutaminase in human serum and plasma from Euroimmun® (Germany) was used according to manufacturer protocol. A positive serology plus a strong clinical suspicion were sufficient to make a diagnosis of CD.
Third generation enzyme immunoassay (ELISA) for the determination of antibodies to Hepatitis C Virus in human plasma and sera from Diagnostic Bioprobes Srl, Milano, Italy was used. The microplates are coated with HCV-specific antigens derived from “core” and “ns” regions encoding for conservative and immunodominant antigenic determinants (Core peptide, recombinant NS3, NS4 and NS5 peptides).
Total RNA was extracted by using the Analytikajena kit (Germany) according to the protocol of the manufacturer
The polymerase chain reaction (PCR) assay was performed using Solis Biodyne master mix (Russia) following the manufactures instructions. The sequences of the primers used were as follows: F. primer GCA GAA AGC GTC TAG CCA TGG CGT and R. primer CTC GCA AGC ACC CTA TCA GGC AGT. The reaction was conducted in a thermocycler using the following protocol; 55 °C for 10 min, 95 °C for 5 min for initial denaturation, 40 cycles of 95 °C for 20 s, 60 °C for 1 minute, and 72 °C for 45 s, final extension at 72 °C for 5 min. All the amplified products were subjected to 2% agarose gel electrophoresis. Positive specimens for HCV resulted in PCR fragments of 244 bp [17].
By ELISA HCV antibodies were detected in 1 out of 50 (2%) in the CD seropositive group and 1 out of 19 (5.2%) in the CD seronegative group. Meanwhile, HCV RNA was detected in 6 out of 50 (12%) of the CD seropositive group and in 4 out the 19 (21%) in the CD seronegative group by PCR.
The cross-tabulation between PCR and ELISA is shown in (Table 3). A total of 50 seropositive CD samples and 19 CD seronegative samples tested using the two techniques were used to compare the results between the ELISA and PCR. Of the first group (CD seropositive), 6 samples were positive by PCR, 1 was positive by both PCR and ELISA and none were positive by ELISA only (6/50 [12%] samples in total). In the second group (CD seronegative), 4 were positive by PCR, 1 was positive by both and none were positive by ELISA only (4/19 [21.1%] samples in total). In all samples, 8 were positive by PCR only, 59 were negative by both techniques and 2 samples were positive by both. By calculating cohen’s kappa coefficient (k), an overall agreement of 87.34% between the two tests was found.
The liver and the intestine are two inseparable organs of the gastrointestinal system, and it is no surprise that dysfunction in either of these organs may also affect the other. An interesting example of this complex relationship is the implication of viral hepatitis in a number of autoimmune disorders, including Celiac Disease (CD) [14,15,17,18]. This may be particularly true in the case of CD, as the cell-mediated inflammatory response to the HCV may involve T cells restricted to human leukocyte antigen (HLA)-DQ2, the class II HLA allele linked to celiac disease [19,20-22]. Numerous studies have tried to prove this possible relationship between HCV and CD, however, none were able to settle the debate in question.
Our study revealed that 1/50 (2%) CD seropositive patients and 1/19 (5%) CD seronegative patients tested positive for HCV antibodies using ELISA, while 6/50 (12%) CD seropositive and 4/19 (21%) CD seronegative patients were found to be positive for HCV-RNA using PCR. These finding are somewhat comparable to a study conducted by Fine, et al. [23], which hypothesized that patients infected with the hepatitis C virus also may have an increased prevalence of celiac sprue compared with other forms of liver disease or with controls without liver disease. On antibody screening, 3/259 (1.2%) HCV patients had antigliadin, antiendomysial, and antitissue transglutaminase antibodies in serum and were subsequently found on intestinal biopsy to have celiac sprue. Also, Silano, et al. [24] found that 34 out of 3,725 CD patients included in their study (0.91%) had positive serology for HCV antibodies.
On the other hand, Gravina, et al. [25] denied any relationship between HCV and CD, where 3/194 CD patients were positive for both HCV antibodies and HCV-RNA. Moreover, Hernandez, et al. [16] did not reveal a direct association between celiac disease and HCV in their retrospective study, but rather suggested IFN-α therapy as the culprit. Out of the 878 CD patients included in their study, only 6 (0.7%) were found to be positive for HCV, 4 of which had received interferon therapy. Additionally, numerous other studies have explained the relationship between CD and HCV as a result of blood borne infection via either transfusion or IV drug use [20,17]. In a study conducted by Teml, et al. [25], comprising 488 patients who were regular CD patients of the outpatient department, 3 of the patients were also diagnosed with HCV. Of these 3 HCV positive patients, 2 required recurrent blood transfusions during labor and one was a known IV drug user. Similarly, in case reports by Colombo et al and Garg, et al. HCV was found to be caused by blood transfusions [20].
Quite noticeably, in both our groups, HCV antibodies were detected far less than HCV RNA. The reason for this is uncertain, but it may indicate that these patients have impaired antibody production against HCV.
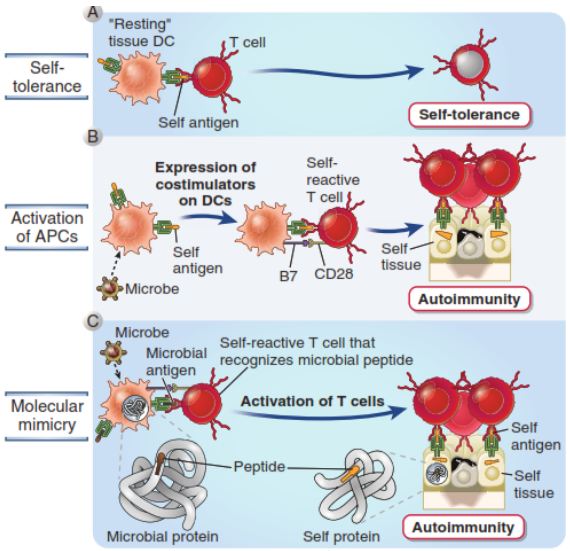
Statistical analysis of the result returned a p value of = (0.445), denying a likely association between the two conditions. However, we strongly believe that by way of molecular mimicry (Figure 1) [12], the similarity between the amino acid sequences of HCV and gliadin might cause an erroneous immune response against gliadin [2,22].
Strong evidence suggests that the primary HLA association in CD is to the classical peptide presenting HLA molecules DQ2 and DQ8 [2]. Similarly, the cell-mediated inflammatory response to HCV may involve T cells restricted to HLA-DQ2 [18]. Many authors have attempted to elaborate the link between HCV and CD, through a great deal of approaches. However, none were able to identify the exact point of intersection between these two entities.
Fine, et al. debated the possibility that inflammatory diseases resulting from antigenic stimuli other than gluten may trigger celiac disease, and posed HCV as a strong candidate, as it was found to cause a number of secondary autoimmune processes in different parts of the body, including lichen planus of the skin and mouth, Sjogren’s syndrome, and the development antinuclear antibodies. This theory was aided by the finding that 52% of the study population were found to have the HLA-DQ2 haplotype [23]. Furthermore, HCV may have amino acid sequences homologous to some gliadin epitopes [26].
Furthermore, in an interesting study by Izadi, et al. bioinformatics tools were used to investigate genes whose interactions is supposedly challenging in both of the CD and HCV pathogenesis and comorbidities. In their study, a total of 105 common genes were found, and CD was significantly related with HCV with P-value < 0.05 [27,28]. It was found that among the CD and HCV assigned genes, there were a number of interferon genes (IFNA1, IFNG) seemingly regulated by NFKB1, IFR1, STAT1 and STAT3 participating in inflammatory and apoptotic events, as well as HLA genes. Of these transcription factors, NFKB is a pivotal regulator of the adaptive immune system, as it modulates the activation, proliferation and survival of lymphocytes. NFKB pathway has been demonstrated to be constitutively upregulated in CD [29]. They concluded that several genes and transcription factors were highlighted which are thought to interact to each other in giving rise to CD-HCV comorbidity principally via immune responses.
The results of our study may favor a non-association between CD and HCV. However, we strongly believe there is a hidden link between these two diseases. In a sense, CD and HCV might overlap more often than we think. A significant number of effector genes were found to be shared by HCV and CD [27]. The interaction between these two entities may be indirect, through activation of various immune pathways. Celiac disease presents itself in a rather vague manner, with nonspecific GI symptoms such as diarrhea and weight loss [1]. Similarly, the first phase of HCV infection, the “prodromal phase”, might also present with nausea, fatigue and weight loss [30]. So, in our second group (CD seronegative), the patients might have actually been experiencing prodromal symptoms of HCV, and due to the clinical similarity of both conditions, were sent for investigating CD. Therefore, it would be logical to test patients suspected of CD and presenting with such vague symptoms for HCV
To the best of our knowledge, this is the first study investigating the possible association between celiac disease and HCV infection in Sudan. Further studies should perform HLA genotyping to detect the presence of the HLA DQ2 haplotype, as well as HCV genotyping, to identify the genotypes associated most with celiac disease. Future studies should focus on the common immune pathways involved in CD and HCV. The immune response should be traced downstream, with the CD4 T cell response as a starting point.