Surgical Outcomes of Thyroid Surgery in a Teaching Hospital in Mid-West Nepal
Objectives: The aim of this study was to evaluate the surgical outcome and complications of various thyroid surgeries in a teaching hospital in mid-west of Nepal.
Study design: Restrospective hospital based study.
Materials and methods: The study was carried out in Universal College of Medical Sciences, Tribhuvan University Teaching Hospital, Bhairahawa, and Rupandehi, Nepal from April 2014 to December 2017. The outcomes and complications (intraoperative and postoperative) of various thyroid surgeries for different benign and malignant thyroid pathology were noted.
Results: There were total 84 cases of thyroid surgery performed during the stated period. There were 75 female and 9 male patients with female to male ratio of 8.3:1. The oldest male patient was of 78 years old and female of 59 years old with the age range of 16-78 years old. The youngest patient operated was in 16 years old female. There were 45 cases of colloid goiter, 2 cases of thyroid cyst, 5 cases of thyroid adenoma, 18 cases of MNG (multi nodular goiter), 6 cases of papillary carcinoma of thyroid, 5 cases of Hashimoto thyroiditis, 2 cases of Hurthle cell neoplasm and 1 case of follicular neoplasm. We had a case of hematoma, 2 cases of transient recurrent laryngeal nerve palsy, 1 case of serous discharge, 2 cases of hypocalcemia, 1 case of numbness above the incision site and1 case of superior laryngeal nerve palsy.
Conclusion: Complications in thyroid surgery are possible, and even inevitable occasionally depending on the nature of disease and patient presentation. However, life threatening complications do occur but rarely. Experienced surgical team, meticulous dissection and early recognition and prompt treatment of complications lead to successful outcome in thyroid surgery.
Keywords: Complication; Hypocalcemia; Multinodular Goiter
The frequency of thyroid surgery in head and neck region is not uncommon and shown to be with an extremely low mortality. It has also specific morbidities which are related to the experience of the surgeon and the nature of disease, however, very low surgical morbidity rates for thyroidectomy are reported in various specialised centres [1]. Documented mortality rate of thyroid surgery was as high as 40% from hemorrhage and sepsis in eighteen century, however, consequent to modern antiseptic, anesthetic facilities and improved surgical techniques along with better hemostatic and surgical instrumentation during the last century has led to tremendous low morbidity and mortality. There are various indications for thyroidectomy like hyperthyroidism resistant to conservative treatment, benign and malignant thyroid tumors, compressive and mechanical disturbances and aesthetic reasons. The type of thyroidectomy is determined by the benign or malignant features of lesion, size of the lesion, and degree of impairment [2,3,4]. Even though most patients fully recover without any adverse events, however, there are reported postoperative complications like wound infection, hematoma/ hemorrhage causing airway compromise, hypocalcemia, recurrent or superior laryngeal nerve injury, thyroid storm and lymph leakage. A thorough anatomical knowledge and meticulous surgical techniques are prerequisite determinants of successful outcomes and minimization of complications [3,4].
The aim of this study is to assess outcomes of different thyroid surgeries done for benign and malignant thyroid diseases and compare it with other published data.
It’s a retrospective study of patients who underwent thyroidectomy from April 2014 to December 2017 in Universal College of Medical Sciences, teaching hospital, Lumbini, Nepal. Patient’s inpatient files from the hospital record books were reviewed regarding indication for surgery, type of surgery and complications like bleeding or hematoma requiring reexploration, change in voice, vocal cord status, hypocalcemia, wound infection, chyle leak. Ethical approval was taking from instituitional review committee. All patients were operated by ENT surgeons. Preoperatively, USG (ultrasonogram) of neck, thyroid function test, FNAC (fine needle aspiration cytology) and other routine tests for PAC (pre anesthetic checkup) along with computerized tomography (CT) in selected cases were done. Routinely, IL (indirect laryngoscopy) were done preoperatively to know the vocal cords status and in cases of hoarseness on postoperative period. NPL (nasopharygnolaryngoscopy) were done pre and postoperatively in cases where IL had difficulty to access. Serum calcium level was measured on first postoperative day and on subsequent days as indicated in some cases and after every case of subtotal, neartotal and total thyroidectomy. Permanent vocal cord palsy or permanent RLN (recurrent laryngeal nerve) palsy was defined as continued postoperative vocal cord paralysis 6 months after surgery and labelled as temporary if improved vocal cord mobility within 3-6 months post-surgery. Hypoparathyroidism leading to hypocalcemia is considered when postoperative serum calcium level is below 7.5 mg/dl or below 8.5 mg/dl if hypocalcemic symptoms are present. It is considered as temporary if patient gets normalized within 3-6 months without calcium and vitamin D supplementation. Likewise, patients requiring more than 6 months of calcium or vitamin D supplementation for postoperative hypocalcaemia were defined as permanent hypocalcemia or hypoparathyroidism. Patients were classified as having hypothyroidism if both clinical like paresthesia and numbness over fingertips and perioral area and muscle cramps which are usually seen 24-48 hours after surgery and biochemical supportive parameters were present. The minimal follow up period was 1 year.
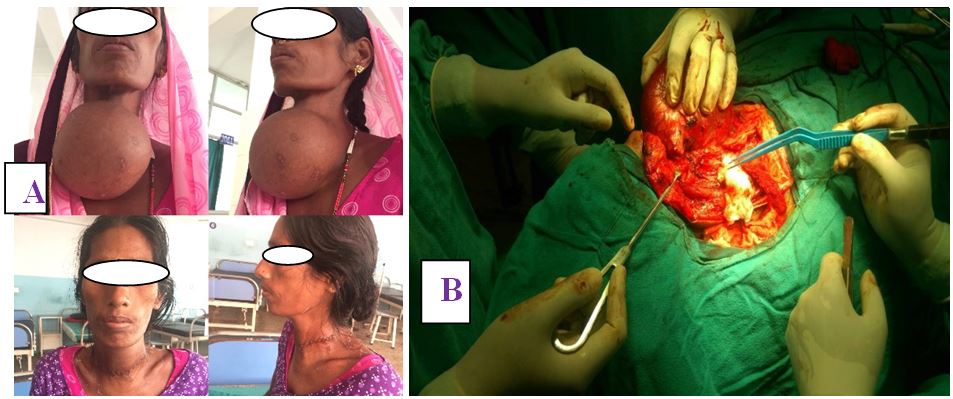
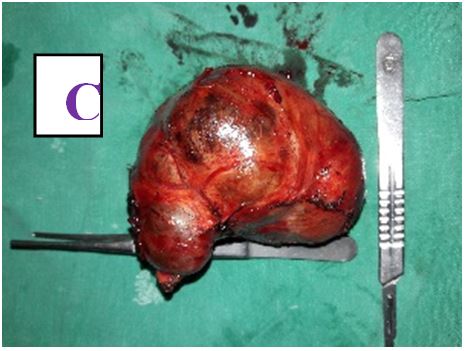
A total of 84 patients, aged between 16 and 78 years (mean, 47 years), underwent different types of thyroid surgery during the study period (Table 1) (Figure 1 and 2). There were 75 female with age range of 16 to 59 years old and 9 male patients with age range of 25 to 78 years old with female to male ratio of 8.3:1. The oldest male patient was of 78 years old and female of 59 years old. The youngest patient operated was in 16 years old female.
There were total 84 cases of thyroid surgery performed during the stated period. There were 75 female and 9 male patients with female to male ratio of 8.3:1. There were 45 cases of colloid goiter, 2 cases of thyroid cyst, 5 cases of thyroid adenoma, 18 cases of MNG, 6 cases of papillary carcinoma of thyroid, 5 cases of Hashimoto thyroiditis, 2 cases of Hurthle cell neoplasm and 1 case of follicular neoplasm.
We had a case of hematoma, 2 cases of temporary recurrent laryngeal nerve palsy, 1 case of numbness (temporary) above the incision site, 1 case of superior laryngeal nerve palsy, 1 case of seroma and 2 cases of hypocalcemia ( 1 temporary and 1 permanent).
The most common indication for hemithyroidectomy was colloid goiter, adenoma, thyroid cyst, solitary thyroid nodule and a papillary carcinoma of thyroid. Subtotal thyroidectomy was done for hashimoto thyroiditis and multinodular goiter. Near-total thyroidectomy was done for hurthle cell neoplasm, hashimoto thyroiditis and multinodular goiter. Total thyroidectomy was done for papillary carcinoma of thyroid and follicular carcinoma of thyroid (Table 4).
Total thyroidectomy with central compartment neck dissection was done in 2 cases (each case of papillary and follicular cell carcinoma).
A patient who underwent right hemithyroidectomy for colloid goiter developed hematoma on first POD (postoperative day) and was managed under LA (local anesthesia) in the ward and oozing was found from the cauterized portion of anterior jugular vein. Hoarseness (temporary) due to right RLN palsy was seen in two cases after near total thyroidectomy. A patient who underwent near total thyroidectomy developed high pitched voice due to SLN (superior laryngeal nerve, external branch, palsy. Out of 6 total thyroidectomies, 1 developed temporary and 1 permanent hypocalcemia. There was a case of serous discharge postoperatively and managed conservatively with regular dressing and pressure bandage. Two patients were observed in ICU after surgery because of suspected tracheomalacia for 24 hours, both cases of huge MNG with neck swelling history of 30-35 years, 1 of them was toxic. Second ring tracheal cartilage was seen eroded partially by the disease intraoperative in a case of follicular carcinoma of thyroid. None of the patients require blood transfusion postoperatively. There was nil mortality till study period.
The main concerned complications post thyroid surgery are hoarseness due to RLN palsy, hypocalcemia and postoperative hemorrhage and it may hamper the social life of the patients throughout. Mortality rate used to be more than 20% in the earlier days, however, with the revolution in the surgical technique, better understanding of the anatomy and pathology of the thyroid, the mortality rate has dropped down to 0.8% and also has helped to keep down the complications within the reasonable limits [5-8].
The total rate of total complications in our study was 9.5% which is below the published results that is 20%, 21%, 24% [4,9,10]. However, other several studies have shown similar rates to ours that is 0.19-2.1% [8,11-13]. Hematoma was seen in 1 case of hemithyroidectomy on 1st POD (postoperative day) and was explored and evacuated under LA in the ward. None of the patients required blood transfusion although there was routine preoperative arrangement. As per the multicentric analytical study done in 2004 by Lodovico R, et al. 1% of the all cases of hemorrhage (i.e., 0.12% of all operated thyroids, n=14934) received blood transfusion and also 80% of the surgeons had not prepared any blood units prior to surgery. Majority of this life threatening complication occur within 24 hours after surgery suggesting acute arterial bleed and presents with respiratory distress, pain and pressure, dysphagia, while, delayed bleeding is of venous origin. It can be prevented by securing hemostasis strictly at the end of surgery. One can be ascertained of bloodless field intraoperatively by increasing the intrapulmonary pressure to 40cm H2O by Valsalva manuevre so as to recognize the bleeder [4].
RLN injury, one of the most debilitating complications, usually manifests with hoarseness or go remain asymptomatic if unilateral injury or with stridor and acute airway obstruction requiring urgent tracheostomy if conservative treatment with high dose corticosteroids and broad spectrum antibiotics fail after 48-72 hours in case of bilateral injury. Corticosteroids should be the first line of treatment together with antibiotics for the vocal cord immobility secondary to RLN injury especially for the goiter with chronic thyroiditis [14]. The incidence of transient and permanent RLN palsy reported in the literature ranges from 3-8% and 0.3-4.8% respectively [4,7,15-20]. The incidence of RLN injury in our study is 2.38% i.e, in corcodance with the published data [4,7,15-20]. The injury was of transient nature as it got improved by 1 month postoperatively with the help of oral corticosteroids in tapering dose and the broad spectrum antibiotics. The cause of the injury in our case seen in post total thyroidectomy done for huge nontoxic multinodular goiter could be due to traction injury and the neural manipulation intraoperatively. Several mechanisms have been proposed for the nerve injury like partial or complete transection, traction, crushing injury, contusion, thermal injury by electrocautery, ischemia, perineural fibrosis, calcification, toxic neuritis, ligature or clip misplacement or compromise blood supply due to edema or hematoma compression [[2,21-24]. In a study [4,23], Grave’s disease, thyroiditis, recurrent goiter, malignant pathology and extensive thyroid surgery were found to be independent risk factors for transient RLN injury whereas presence of Grave’s disease and recurrent goiter undergoing reoperative surgery were suggested as independent risk factors for permanent RLN injury. Additionally, surgeons experience or surgeon’s patients volume and the consequences of nonsurgical aspects including anesthetic procedures (0.4-3%) like trauma while difficult intubation, mucosal erosions or edema or even subluxation of arytenoid cartilage are also catergorized for RLN injury [2,18]. Several studies have proposed recommendations for identification and preservation of RLN during thyroidectomy like routine identification, capsular dissection since nerve is always extracapsular, special attentions to be made while dissecting on the right side as in 1% of cases nonrecurrent RLN has been found, hence it has been said that there’s high chances of right RLN injury intraoperatively, to cover the bare nerve with luke warm wet gauze when removing thyroid from laryngotracheal axis, use of bipolar cautery near the nerve, follow the landmarks like Beahr’s triangle, Simon’s triangle, pay attention to RLN entry site into the larynx near Berry’s ligament as nerve passes behind Zuckerkandl’s Tubercle lateral to Berry’s ligament and use of intraoperative nerve monitor [8,18,25,26].
There had been reports of 0-58% of post-operative external branch of superior laryngeal nerve (EB-SLN) injury [27-29] and could be transient or permanent. Post-operatively, patients usually manifest with voice fatigue, problems reaching high-pitch sounds that they were used to reach, and the need of an extra effort to speak; can also complain of various rates of dysphagia. It often goes unnoticed and under reported as it is highly noticed in professional speakers like singers, politicians, teachers [4,18]. In our study, a female patient who underwent near total thyroidectomy for nontoxic MNG developed high pitched voice due to SLN palsy. However, she was complaint free at 6 months follow up. Generally, it gets injured while ligating the superior thyroid vessels near the capsule of the gland [4]. Routinely, postoperative IL was not performed so we would have missed the SLN palsy in the beginning and it accounted as the limitation of this study.
The incidence of temporary and permanent hypocalcemia ranges from 1.6-50% and 1.5-4% respectively reported by the various literatures. In our study, we had 1 case of transient hypocalcemia seen in near total thyroidectomy (1/15) done for huge MNG and 1 case of permanent hypocalcemia seen in total thyroidectomy (1/6) done for follicular carcinoma of thyroid. Dissimilarity in the reported incidence of hypocalcemia could be the consequence of variations in surgical technique, diseases and the defining factors. However, the risk factors so far have been observed are malignancy, postoperative wound infection, lymph node dissection, hyperthyroid state, few number of parathyroid glands preserved, low preoperative serum calcium level, revision surgery, autotransplantation of parathyroid glands [30,31]. There’s been a controversy on what exact numbers of parathyroid glands need to be preserved to avoid postop hypocalcemia. As per few centers a functioning gland is enough whereas others recommend at least three to be preserved [32,33].
The incidence for seroma after thyroid surgery varies from 1.3% to 7% [34]. We had a case of seroma which was seen on the first week of near total thyroidectomy for huge MNG. It was managed successfully with 2 attempts of aspiration and pressure bandage. In few cases we had used continuous sutures otherwise interrupted in most of the cases. Till date, we haven’t encountered a case of hypertrophied or keloid scar during the follow up.
Complications in thyroid surgery are possible, and even inevitable occasionally depending on the nature of disease and patient presentation. However, life threatening complications do occur but rarely. Experienced surgical team, meticulous dissection and early recognition and prompt treatment of complications lead to successful outcome in thyroid surgery.