The Role of Antibiotics in Post Tonsillectomy Morbidity: An Experience at Tertiary Centre, Steve Biko Academic Hospital, University of Pretoria
Introduction: Tonsillectomy with or without adenoidectomy continues to be one of the most common surgical procedure performed worldwide. Its main complications are post tonsillectomy bleeding, infection and pain. Despite improvements in anaesthetic and surgical technique, post-tonsillectomy morbidity has continued to be a significant clinical concern.
Objective: To determine clinical benefit of antibiotics for reduction of post tonsillectomy morbidity. The primary outcome measures were pain, time to return to normal diet and activity and secondary bleeding.
Study design: A randomized, prospective, placebo controlled double blind study, ENT department, University of Pretoria.
Methods: Subjects were recruited and randomised into Group A (antibiotics) or Group B (placebo). A diathermy technique was used on all patients. Pain was measured using a visual analogue score (VAS) and patient morbidity score (PMS).
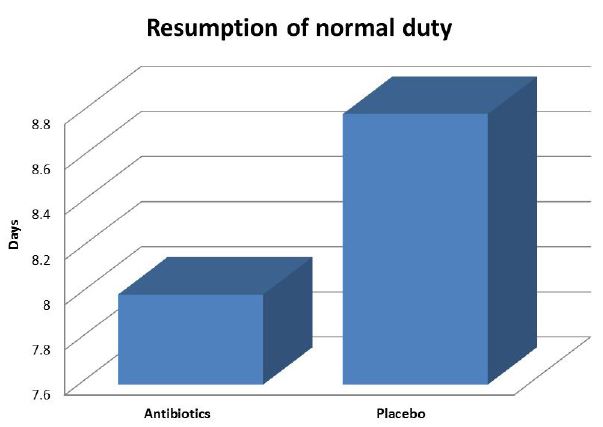
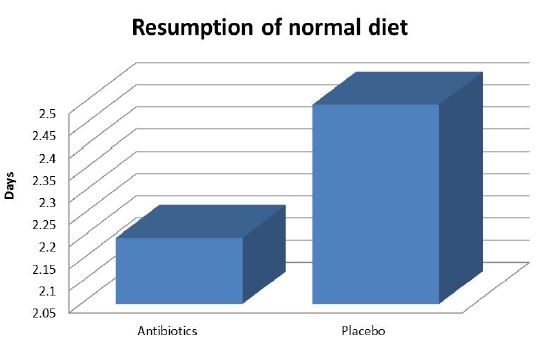
Results: Eighty-five patients were recruited of which 40 were included in Group A and 45 in Group B. Seven patients dropped out of the study. There were 41 females and 37 males with age ranging between 16 and 49 years. No haemorrhage reported in both groups. The mean duration for resuming normal diet was 2.2 and 2.5 days (p=0.449) and for returning to normal duty was 8.1 days and 8.8 days (p=0.433) for Group A and Group B respectively. There was no statistically significant difference in VAS and PMS pain scores measured between the two groups. Patients who started eating early and continuous with or without the presence of pain recovered much quicker. Staphylococcus aureus was the most common organism cultured.
Conclusion: The usage of antibiotics in post-tonsillectomy patients does not seem to reduce morbidity associated with tonsillectomy even in patients with positive culture. Early and continuous feeding has some beneficial effect.
Keywords: Antibiotics and Tonsillectomy; Post Tonsillectomy Morbidity; Pain; Time to Return to Normal Diet and Daily Activity; Secondary Bleeding
Tonsillectomy with or without adenoidectomy continues to be one of the most common surgical procedure performed worldwide. Its main complications are post tonsillectomy complications are bleeding, infection and pain [1]. Despite improvements in anaesthetic and surgical technique, post-tonsillectomy morbidity has continued to be a significant clinical concern [2]. This procedure is surrounded by controversies, especially regarding the tonsillectomy technique and adjuvant therapy in post-operation period [3].
In an effort to reduce morbidity associated with the procedure different methods (tonsillotomy and tonsillectomy) apart from cold steel instruments; harmonic scalpel, debridor, coblation, laser,radiofrequency, diathermy techniques have been used. The diathermy (monopolar/bipolar cautery) method is one of the commonest techniques used today due to cost and dry field. It involves separating the tonsil capsule from the constrictor muscle by way of electro cauterization [4].
Adjuvant therapy in the form of local anaesthetics, dexamethasone intra-operatively and postoperative antibiotics have been used in an effort to reduce morbidity. To date there is no conclusive clinical evidence demonstrating the benefit of using antibiotics in post tonsillectomy morbidity. Penicillin resistance in streptococcus pneumonia and Haemophilus influenza resistance to amoxicillin have increased worldwide in recent years including Africa [5]. The 2014 WHO report identified Africa and South East Asia as the regions without established Antimicrobial resistance surveillance systems [6]. The kinds of patients who present for operations in our community are mainly due to chronic bacterial tonsillitis that requires antibiotic usage post operation. Increase antibiotic resistance has been proven to be due to increase antibiotic usage. One factor contributing to antimicrobial resistance is misuse of antibiotics [5]. This lack of quality data is problematic often leading to treatment guidelines that are not adequate for the local situation. The gap in public health capacity is also an issue given the changing resistance mechanisms and the emergence of multidrug-resistant bacteria, that can only be detected through systematic screening in quality assured microbiology laboratories [7,8]. Our aim was to determine clinical benefit of antibiotics for reduction of post tonsillectomy morbidity. The primary outcome measures were pain, time to return to normal diet and activity and secondary bleeding.
Postoperative usage of oral antibiotics is no better than placebo in reducing morbidity after tonsillectomy or adenotonsillectomy.
Postoperative pain, time to return to normal diet and activity and secondary bleeding were selected as separate primary endpoints for assessment of post tonsillectomy morbidity.
A randomized, prospective, placebo controlled double blind study conducted at a department of Otorhinolaryngology (ENT), Tertiary centre Steve Biko Academic Hospital (SBAH), University of Pretoria, South Africa. The study was done between March 2015-2018. A total of 85 adults patients booked for tonsillectomy were invited into the study.
Inclusion criteria: Adults (>16yrs) diagnosed with recurrent or chronic bacterial tonsillitis during the study period, Exclusion criteria: All patients with peri-tonsillar abscess, Antibiotics administered within 1 week before surgery, bleeding diathesis, HIV, Immunocompromised, penicillin/cephalosporin allergy, Prosthetic cardiac valves or rheumatic heart disease.
Patients were randomly allocated numbers from 001 to 100 designating either an antibiotic or placebo group (the researcher was blinded). The numbers had a medicine code (only the pharmacist could break the code) and an attached letter (sealed) to the anaesthetist instructing whether to give antibiotics or placebo intravenously before commencement of the operation. The researcher randomly allocated the numbers. The patient received following treatment regimens depending on whether the allocation was Group-A, 42 (antibiotic group) or Group-B, 43 (placebo group)
Group A received: Ampicillin/1g given intravenously in theatre during induction. Amoxicilling/250mg 8 hourly orally for 10 days. Chlorhexidine antiseptic gargle 6 hourly for 10 days. Paracetamol 2 tabs 8 hourly orally for 10 days when necessary.Indocid suppositories 100mg daily for 10 days when necessary
Group B received: Normal saline 2ml intravenously in theatre during induction. Placebo caps (same as amoxicillin in appearance) 8 hourly for 10 days. Chlorhexidine antiseptic gargle 6 hourly for 10 days. Paracetamol 2 tabs 8 hourly orally for 10 days when necessary. Indocid suppositories 100mg daily for 10 days when necessary
All operations were done by the researcher using the diathermy technique on all subjects. A pus swab was taken from tonsillar crypts before the commencement of the operation and send for microscopy, culture and sensitivity. Intra-operatively; the length of the operation was recorded as well as the diathermy machine voltage setting. All patients were discharged the following day and given a patient morbidity scoring (PMS) form were they indicated the severity of the pain on a daily basis. They also recorded the day they started eating normal diet, returned to normal physical activity and any other events e.g. bleeding. The patients were followed up at the clinic once a week for a period of three weeks. On review a visual analogue pain score based on 10cm line was used to estimate the severity of pain in the preceding weeks. The patient were asked to mark on the line with the left end indicating no pain and the right end indicating the most severe pain.
The Student’s t-test was used to calculate any statistically significant difference in the number of days before resuming normal diet and duty.
The same test was also used to compare pain scores and postoperative bleeding between groups. This was done in consultation with a statistician. The micro-organisms were identified using the standard tests available in the laboratory.
Ethics approval obtained from the institutional research ethics committee. There was no cohesion; any patient could withdraw at any time with no penalty.
Eighty-five (85) patients were entered in the study. Of these, only seventy eight (78) were analysed and seven dropped based on poor follow up. The indication for tonsillectomy in all patients was recurrent bacterial tonsillitis.
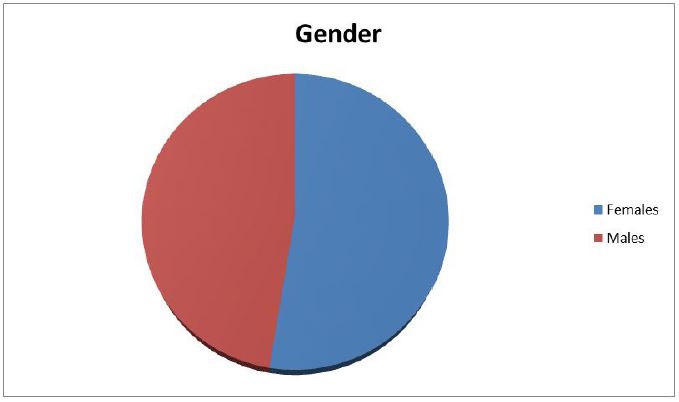
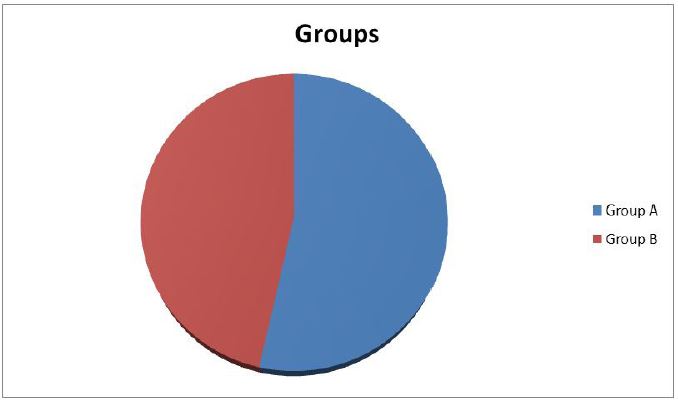
There was a slight predominance of females: Females forty-one (41) with thirty-seven (37) males (Figure 1). The age ranged between 16 and 49 years with a mean of 32 years. Forty (40) were randomized to Group-A and thirty-eight (38) to Group-B (Figure 2). The mean age for Group-A was 31 years and Group B 33 years.
The average time for the tonsillectomy procedure was 10 minutes. The monopolar diathermy voltage setting for both groups was 15mV on average for coagulation and cutting modes.
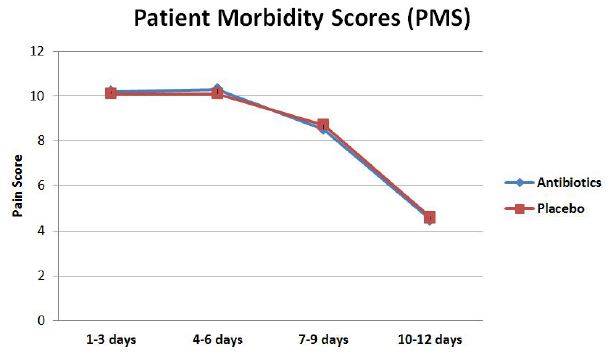
The pain scores as measured with patient morbidity score (PMS) were 10.2 and 10.4 for day one to three (p=0.721), 10.4 and 10.7 for day four to six (p=0.581), 8.9 and 8.7 for day seven to nine (p=0.716), 4.8 and 4.6 for day ten to twelve (p=0.601) for Group-A and Group-B respectively. All were statistically insignificant (Figure 3).
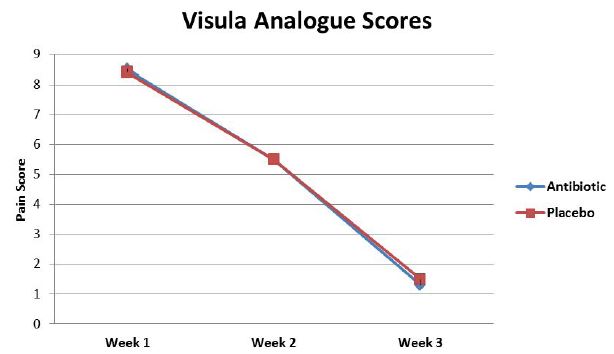
The post-operative pain turned to be worse from day four to six in both groups (Figure 4). The scores for the visual analogue scale (VAS) were 8.4 and 8.8 for week one (p=0.445), 5.5 and 5.3 for week 2 (p=0.767), 1.7 and 1.4 for week three (p=0.348) for Group-A and Group B respectively all being statistically insignificant. The VAS showed a steady decline over the three-week period.
The day of resumption of normal duty for Group-A and Group-B was 8.1 and 8.8 days respectively with a statistically insignificant p-value of 0.433 (Figure 5).
The day of resumption on normal diet for Group-A and Group-B was 2.2 and 2.5 days respectively with p-value of 0.433 (Figure 6).
The commonest microorganisms cultured were staphylococcus aureus (27) Group A β- haemolytic streptococcus (20) and haemophilus influenza (19). In 23 patients, no organisms were cultured. The antibiotic sensitivities are indicated in Table 1 Viral cultures were not reported.
When data compared between patients who had pain but ate early and continuous and those who had pain but were reluctant to eat continuously. Those who ate early and continuously show statistical significant benefit in both pain and return to normal activity (p-0.045 and p-0.041 respectively) in both group A and group B.
No bleeding reported in both groups during the study period of 3 weeks.
Pain is the main complaint from patients undergoing tonsillectomy despite the use of anti-inflammatory analgesics. The cause of pain is thought to be the exposed nerve endings and the chemical mediators of inflammation such as lactic acid, leukotrienes and prostaglandins that lead to muscle spasms [4,2]. The use of antibiotics in post tonsillectomy patients was found to reduce the bacterial content of tonsillar fossa therefore minimizing infections and facilitating healing [2,9]. The presence of infection would be indicated by secondary haemorrhage, severe pain, fever and delayed resumption of normal activity and diet. There was no secondary haemorrhage experience in this study suggesting that there was no severe infection even in the placebo group. However, considering the size of the sample, one need to interpret this finding rather cautiously as the incidence of post-operative bleeding is generally estimated around 3-5% [1,4]. Pain perception and scoring (VAS) is very subjective and varies between different age groups and between different races, males and females [3,10]. Although there was slight predominance of females in Group-A; this failed to reach statistical significance. Subjects in Group-B were younger but again this could not reach any statistical difference of significance. Although Colreavy, et al. found that patients on antibiotics recovered much earlier, the mean age group between the groups in not mentioned [11]. Their sample consisted of children with a mean age of 6.2 years. Inadequate food (fluid) consumption after tonsillectomy is significantly associated with an increased incidence of secondary haemorrhage [1,4]. Determination on the side of parents to persuade children to eat continuously therefore becomes a significant factor. Our study included only adults above sixteen years of age. In this study, all patients were encouraged to eat as soon as possible after recovering from anaesthesia and continue to eat regular meals thereafter regardless of the presence of pain. Patients who ate early and continuously showed a much quicker recovery regardless of whether they were on antibiotics or on placebo. The two methods used to assess pain (VAS and PMS) showed a steady decline of pain over the three-week period. There was however a tendency for the pain to get worse between day 4 and 6 in both groups with no statistically significant difference between the two groups (Figure 3). This pattern was consistent with findings of other studies [12,13]. Patients on antibiotics experienced significantly less mouth odour, were able to tolerate a regular diet sooner, and resumed the normal activities earlier that did patients who received placebo [12]. Burkart, et al. in a meta-analysis showed that patients on antibiotics resumed normal diet only one day earlier than the non-treatment/placebo group [2]. Our study showed no statistical difference in both pain and return to normal diet and activity in line with findings of O’Reilly 36% of tonsil swabs yielded no growth, which means that at the time of surgery a significant number of tonsils do not harbour significant bacteria or viral infection [2,9]. This low yield could not be explained by the fact that only swabs were taken and not tonsil tissue. Colreavy compared microbiological profile of tonsil core tissue and tonsil swabs and found similar organisms in both [11]. Staphylococcus aureus and β-haemolytic streptococcus were found to be the most common bacteria in keeping with other studies [5,6,14]. The one weakness in the microbiological technique in our study is that anaerobes and viruses were not specifically cultured. It has been shown that up to 25% of tonsil core grow significant anaerobes [11,13,15].
Burkart in the meta analysis studies made note of these findings that although cursory cost of analysis suggests possible cost effectiveness, clinical decisions regarding the routine use of post tonsillectomy antibiotics must include weighing the potential down sides of side effects and increased antibiotic resistance patterns against potential advantages of a one day earlier return to diet and activity [2].
From this study, it is evident that post-operative antibiotics usage does not affect the post tonsillectomy morbidity. The single most important beneficial factor is early and continuous regular feeding. Our recommendation is that routine use of antibiotics in post-tonsillectomy should be discouraged even in positive culture does not require routine antibiotics. Patient individualization in the emergency of antimicrobial resistance, side effect and cost of medication.
In the cultures; viruses and anaerobes were not specifically cultured for and post tonsillar fossae were not swabbed. The sample size is also small.
I thank patients, colleagues in the pharmacy department at Steve Biko Academic Hospital, and anaesthesiology, microbiology and statistics departments at the University of Pretoria for contributions they have made.
I also thank the patients and family members for unselfishly contributing to medical science through participation in research.
My secretaries, Bernadette Khoele and Patricia Kgari for typing.