Three-Year Incidence Trend Analysis of Tuberculosis Cases in Northern Sierra Leone
Background: Pulmonary tuberculosis is a highly contagious airborne infection caused by Mycobacterium tuberculosis or Mycobacterium bovis. The risk of becoming infected with the pathogen is mostly determined by exogenous factors although the disease can also be caused by non-external factors. Tuberculosis remains a serious public health issue despite the availability of effective drugs to treat it.
Objective: In this study we analyse the three-year tuberculosis incidence rate from 2015 to 2017 for northern Sierra Leone in order to determine whether there are differences in tuberculosis trends based on annual incidence rate, sex and the different types of tuberculosis infection.
Methodology: We analysed the laboratory records of persons screened for tuberculosis using sputum smear and culture diagnostic methods at the Stoko TB/Leprosy Center in Makeni, Sierra Leone from 2015 to 2017. All study subjects whose laboratory results were analysed in this study had come for tuberculosis tests after showing clinical signs and symptoms of tuberculosis.
Results: One thousand four hundred and sixteen subjects (1416) were screened for tuberculosis at various dates between the period 01/01/2015 to 12/31/2017. Majority (941/1416) were positive for pulmonary tuberculosis. The incidence rate of tuberculosis is higher in men (78.20%) than in women. There was a statistical difference in the average number of pulmonary tuberculosis and extra pulmonary tuberculosis cases (t = -13.11, df = 63.77, p – value = 2.2e-16, 95% CI = -19.39775 -14.26891).
Conclusion: More male tuberculosis cases than female were reported in our study.
Recommendations: We are calling on the up scaling of tuberculosis control program that will target the screening of women for TB in Sierra Leone. We are calling for an upscaling of programs that will make women to present themselves for tuberculosis screening. Also, we are calling on the national tuberculosis programmes to step-up and recognise men as an underserved high-risk group as well as for an improvement of overall men’s access to both tuberculosis diagnostic and screening services in order to reduce the overall burden of TB and hence ensure TB care in terms of gender equity.
Keywords: Epidemiology; Trend; Tuberculosis; Screening; Incidence
Tuberculosis (TB) is a highly contagious and airborne infection mainly caused by Mycobacterium tuberculosis (MTB) or Mycobacterium bovis (M.bovis) [1]. MTB was first discovered by Robert Koch in 1882 and infects one third of the world’s population; with 8.7 million new cases reported annually [2]. M.bovis is the main cause of bovine tuberculosis but sometimes it can cross the species barrier and affects humans [3]. M.bovis infection accounts for a small fraction (0.5 – 7.2%) of all patients with laboratory-confirmed diagnosis of tuberculosis globally [4]. The risk of becoming infected with the TB pathogen is mostly determined by exogenous factors although the disease can also be caused by certain non-external factors. Alongside with HIV/AIDS, TB remains a serious public health issue despite the availability of effective drugs to treat it [4,5]. A third of the world’s population have been exposed to the TB pathogen as well as potentially infected [6]. In 2012, TB killed 1.3 million people [7]. The WHO among its Stop TB Strategy included the search for effective active TB diagnostic and treatment in order to address the major epidemiological and health care system challenges, as well as to promote innovative TB research [8]. Only a fraction of TB exposed persons becomes sick with TB [9,10]. People living with HIV, or having a weakened immune systems have elevated risk of falling ill from TB. The absolute number of incident TB cases has been decreasing slowly since 2000s [11].
There are differences in TB notification rates based on socio-demographic characteristics; with higher TB notification rates recorded in men compared to women [12]. Thorson, et al. 2007 postulated that the high TB notification rates in men compared to women may be due to biological differences between men and women in certain age groups which affects the risk of being infected with TB as well as the risk of the disease progressing to active disease [13]. Differences in societal roles of men and women which influences it with men’s risk to TB exposure as well as to access is also cited as possible reasons for differences in TB notification rates among sexes to TB and access to care (gender differences) [11,14-16].
There are different types of TB based on the location of the disease: pulmonary TB (PTB) occurs when the Mycobacterium tuberculosis pathogens reside in the lungs or tracheobronchial tree; extra pulmonary TB (EXPTB) occurs when the Mycobacterium tuberculosis reside in sites such as the peritoneum, lymph nodes, genitourinary tract, bone and joint.
Sierra Leone is one of 30 countries with the highest burden of the disease in the world [15]. In 2016, there were 14,114 TB cases although many more cases likely go unreported and that 8,000 Sierra Leoneans living with TB are unaware of their status and hence untreated [16]. In this study we analysed the TB incidence rates from 2015 to 2017 to determine whether there are differences in trends based on types of TB infection.
We analysed the laboratory records of persons screened for TB at the Stoko TB/Leprosy Center (STBLC) in Makeni, Sierra Leone from 2015 to 2017. STBLC is the main TB/Leprosy treatment center in northern Sierra Leone. All study subjects whose laboratory results were analysed had come for TB tests after showing certain clinical signs and symptoms of either TB or HIV. STBLC uses the sputum smear and culture methods for TB diagnosis. The sputum smear method of TB diagnosis involves mounting a small portion of the sputum of a suspected TB case under a microscope. The presence of visible TB germs under the microscope indicates sputum smear positive TB. A culture test is a validation test usually done after the sputum smear microscopy technique. The culture method involves growing the Mycobacterium tuberculosis obtained from the sputum of a suspected TB patient on anagar culture plate in order to determine its presence. For microscopic TB test STBLC is using the acid fast bacteria modified Zieh Neelsen (ZN stain) staining test in its laboratories. The Zieh Neelsen is being used because of its affordability. This study analysed the laboratory results of all persons who were screened for TB at STBLC from 2015 to 2017.We only analysed smear positive TB cases that have been confirmed by culture test. In this study, all cases that were smear positives ended up to be culture positive as well. All analysis of the medical records of the TB cases in this study was done irrespective of whether such cases are comorbid with HV or other disease.
The TB patients whose laboratory results were analysed in this study were either self-reported or brought to STBLC by their relatives as suspected TB cases. These suspected TB patients were first screened upon their first appearance, diagnosed and had their medical history recorded on case report forms.
R software package version 3.3.1 was used for all descriptive and exploratory statistical analysis in this study and p-values of < 0.05 were considered significant for all two-sided statistical tests. The results of our descriptive analysis were presented as frequencies, proportions, means and standard deviations for all variables analysed in this study. T-tests were used to compare differences in the average between continuous variables.
Approval for this study was obtained from both the management of STBLC and the Institutional Review Board of Njala University in Sierra Leone. The Njala University Institutional Review Board waived the requirement to obtain informed consent on the grounds that the study involves minimal health risk on participating study participants.
One thousand four hundred and sixteen persons residing in Bombali district and environs were screened for TB at various dates between the period 01/01/2015 to 12/31/2017. Majority of the people screened were PTB positive (941/1416) and were male (61.23%). There were more PTB positive male (78.20%) cases than female (21.80%) (Table 1).
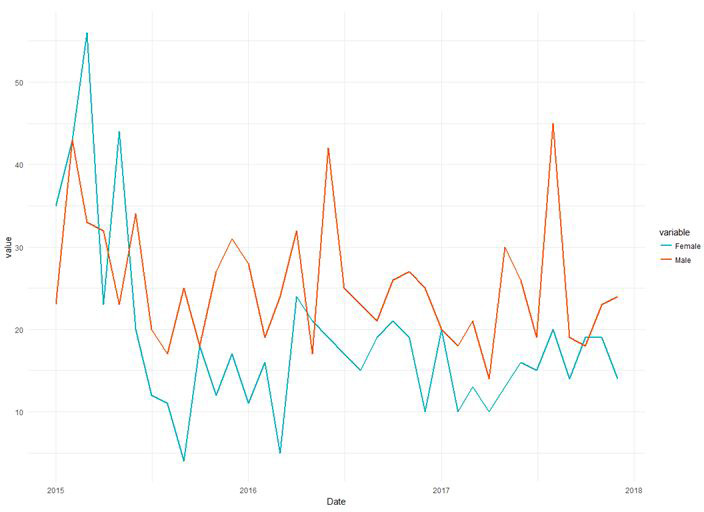
Few (9.89%) of those screened were negative for PTB. There was a statistical significant difference in the average number of positive and negative PTB cases (t = 19.91, df = 45.61, p – value = 2.2e-16, 95% CI = 20.00 -24.50). There was a statistical difference in the average number of male subjects screened compared to female (t = 6.70, df = 64.30, p – value = 6.095e-09, 95% CI = 6.20-11.47) (Figure 1).
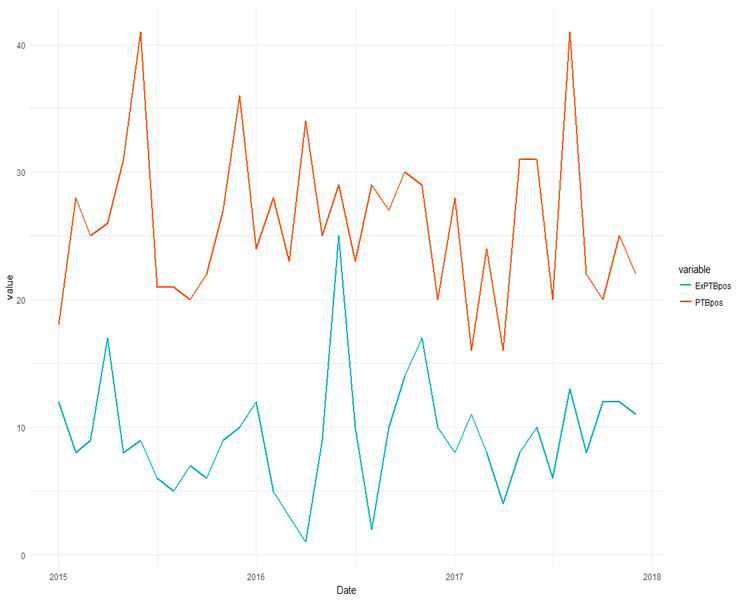
Majority (66.46%) of those screened were positive for PTB; while 23.66% were positive for EXPTB (Figure 2). Majority (77.58%) of the EXPTB cases were lymph node EXPTB; few (22.42%) cases were osteal EXPTB. Majority of the subjects tested positive for PTB.
2016 recorded the highest (118 per 100,000) incidence of EXPTB; 2015 (106 per 100,000) and 2017 (111 per 100,000). Overall, 2016 recorded the highest (325 per 100,000) PTB incidence; 2015 (317 per 100,000) and 2017 (299 per 100,000).There was a statistical significant difference in the average number of PTB cases and EXPTB cases (t = -13.11, df = 63.77, p – value = 2.2e-16, 95% CI = -19.39775 - -14.26891).
Majority (489/1416 per 100,000) were screened in 2016 compared to 2015 (467 per 100,000) and 2017 (460 per 100,000) (Table 1). In 2015, slightly more male (64.18%) than female were screened and tested positive for PTB (59.23%). Of the PTB positive cases diagnosed in 2015, majority (64.35%) belonged to the age group 25- 30 years. In 2016, more male (58.65%) were screened and tested positive for PTB (69.38%). Of the PTB positive cases, majority (57.46%) belonged to the age group 20-25 years. Few people were screened for TB in 2017; male (58.24%) and male positive PTB (63.81%). Majority (66.26%) of those tested for PTB belonged to the age group 25 – 30 years.
Incidence trend analysis studies are important steps in formulating and evaluating preventive strategies for a disease. The incidence rates for PTB and EXPTB varies for the period under review. Majority of the subjects screened in this study were positive for pulmonary TB (66.46%) and were male (61.23%). TB incidence which is estimated as the number of new PTB, EXPTB and smear positive cases is often used to evaluate national TB control programs. From our findings the incidence of TB for northern Sierra Leone for the period under review is very high. The TB incidences recorded in this study are 423 per 100,000, 443 per 100,000, and 410 per 100,000 for 2015, 2016 and 2017 respectively. The WHO annual TB incidence for Sierra Leone in 2016 is 304 per 100,000 [17]. Our high male TB burden is similar to that of many studies [11,18-23].
Our high male TB burden may not be unconnected with our high male TB case notification rates although notification data is insufficient to account for sex differences in disease burden. The high male TB incidence in this study may also be attributed to the fact that men are often disadvantaged in seeking or accessing TB care in most low and middle-income country [23]. This analysis was done on aggregate data obtained from the laboratory results of subjects screened from 2015 to 2017 hence we are unable to present any conclusion on the significance of the role played by the socio-demographic characteristics of screened subjects on the TB incidence trend.
Our study presents a clear insight into the trend of TB in northern Sierra Leone, particularly the incidence on PTB. We have highlighted the need for women to present themselves for TB screening as well as provided the epidemiological data that will serve as a meaningful start for designing measures and policies to help mitigate the rising trend of PTB in the country. We are calling on the up scaling of TB control program that will target the screening of women for TB in Sierra Leone. Finally, we are calling on the national TB programmes to step up and recognize men as an underserved high-risk group as well as for an improvement of overall men’s access to both TB diagnostic and screening services in order to reduce the overall TB burden of TB more effectively and hence ensure TB care in terms of gender equity.
Based on the low TB screening rate for women we are recommending an upsurge in female TB surveillance since we believe that TB cases for women are underreported.
We are grateful to the staff of Stoko TB/Leprosy center in Makeni, Sierra Leone for graciously providing the data used in this study.