Transient Drug-Induced Myopia
Myopia (nearsightedness) is a refractive error, a condition in which the cornea and lens of the nonaccommoding eye have too much plus power for the length of eye. As a result, images of distant objects are focused in front of the retina and thus appear blurred. Transient drug-induced myopia is a myopia induced by a drug as a transient side effect. Several case reports of transient drug-induced myopia have been reported. These cases have been associated with secondary angle closure glaucoma and other ocular conditions such as choroidal detachment, maculopathy, retinal folds. Drugs known to produce this effect include sulfa drugs and other medications. The possible mechanism is thought to be an allergic reaction to the drug. Both ciliary muscle contraction and ciliary body edema may play role in the pathomechanism. Differential diagnosis is made with a number of conditions, either ocular in origin or associated with an underlying systemic cause. Discontinuation of medications leads to complete resolution of the anatomic shift.
Keywords: Transient; Drug-induced myopia; Myopia; Sulfonamide; Drugs; Side effects
Myopia is the most common eye disease and is one of the leading causes of vision impairment worldwide [1,2]. Prevalence of myopia is significantly different among racial groups, although its worldwide prevalence is approximately 30% (3%–84%) [3]. The highest prevalence is found in East Asia, such as mainland China [3]. The prevalence of myopia in the US population was estimated in the early 1970s to be 25% in persons aged 12 to 54 years [4]. A recent meta-analysis of population-based studies found a prevalence of 25% in persons over age 40 [5].
Myopia (nearsightedness) is a refractive error, a condition in which the cornea and lens of the nonaccommoding eye have too much plus power for the length of eye. As a result, images of distant objects are focused in front of the retina and thus appear blurred.
Myopia has been recognized as a distinct visual disability for millennia and has been known for more than 2000 years and was first described by the ancient Greeks [6,7]. It was probably the ancient Greeks who coined the term, using the roots myein (to close) and ops (eye) to characterize those individuals who narrow their eyelids to improve distance visual acuity, the pinhole effect. The focus of distant parallel rays of light falls anterior to the retinal plane and produces a blurred image in myopia. This situation can arise because either the primary refractive components are too powerful or the globe is too long. Thus, myopia can be due to increased corneal or lenticular curvature, or an increase in the lens index of refraction, as occurs with the development of nuclear sclerosis. More commonly, myopia is the result of axial elongation of the posterior segment of the eye.
Transient drug-induced myopia is a myopia induced by a drug as a transient side effect. A side effect (adverse drug reaction) is basically an unintended, unwanted occurrence that results from taking a drug. An adverse drug reaction is an expression that describes harm associated with the use of given medication at a normal dosage during normal use. Adverse drug reactions may occur following a single dose or prolonged administration of a drug or result from the combination of two or more drugs [8]. All drugs that come in the market may cause side effects, where many are minor and few are serious.
Several case reports of transient drug-induced myopia have been reported. These cases have been associated with secondary angle closure glaucoma and other ocular conditions such as choroidal detachment, maculopathy, retinal folds [9]. Drugs known to produce this effect include sulfa drugs. Ingestion of sulphonamide-derived drugs has been reported to possibly have ocular side-effects [10-15]. Among these drugs are acetazolamide (Diamox) [16-21], indapamide [22,23], sulphasalazine [24], methazolamide [25], cotrimoxazole [26,27], ethoxzolamide (Cardrase)[28], hydrochlorothiazide (Hydrodiuril) [29-31], chlorthalidone (Hygroton) [15], psychotropic agents [32].
Several case reports of a similar condition have been published following the use of topiramate, a sulfonamide derivative used for treatment of migraine headaches, seizures, alcohol abuse and other drug dependencies [15, 33-51].
Transient myopia can also be caused by other drugs such as promethazine hydrochloride (Phenergan) [52], prochlorperazine (Compazine) [53], insulin [54-57], IGF1 and FGF2 [58], antithrombotic [59], opiate [60], tetracycline [15,61], aripiprazole [62,63], amisulpride [64], oseltamivir [65], mefenamic acid [66], ectasy [67], phendimetrazine and ephedrine used as anorexiants [68], equine antilymphocyte globulins [69], metronidazole [70], aspirine and deturgylone [71,72], isotretinoin (accutane) [73], isosorbide dinitrate [74], quinine [75].
Drugs may induce refractive power of the eye by one of three mechanisms: [1] substained contraction (spasm) of the ciliary muscle, causing increased refractivity of the lens; [2] increases refractive power of the lens contents as the result of water imbibition; and [3] swelling of the cilairy processes, causing forward displacement of the lens. Increased refractive power of the lens or sustained accommodation increased myopia.
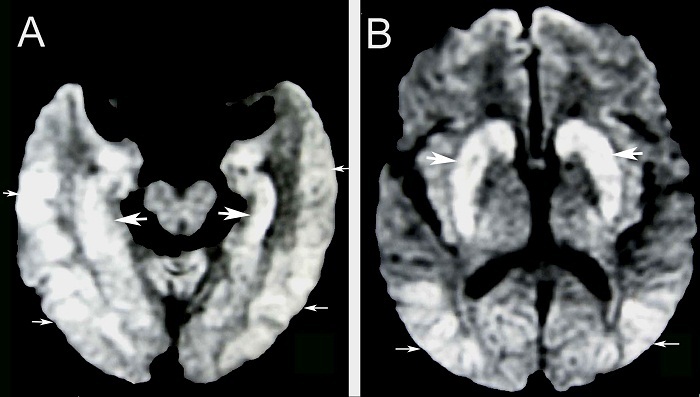
The possible mechanism is thought to be an allergic reaction to the drug. Both ciliary muscle contraction and ciliary body edema play a role in the pathomechanism. Ultra Biomicroscopy (UBM) explains this mechanism by demonstrating supraciliary choroidal (ciliochoroidal) effusion causing forward displacement of the ciliary body-lens-iris block (diaphragm) and relaxation of zonular fibers leading to myopia, anterior chamber shallowing and angle closure glaucoma [76].
Patients present with headache, pain and sudden bilateral loss of distant vision with normal vision at near representing the myopic shift, and occurring prior to symptoms and elevated intraocular pressure. Patients present acute onset of blurry vision and have features of bilateral acute angle closure, myopic shift and elevated intraocular pressure. Examination shows anterior chamber flattening combined with lens thickening and echography disclosed bilateral 360 degrees shallow choroidal detachments. Clinical presentation is variable, not all patients have the complete presentation.
Transient myopia has been reported to occur in a number of conditions, either ocular in origin or associated with an underlying systemic cause. Other causes of transient myopia may include:
1. Nearwork-induced transient myopia: after a sustained near task, near work [77,78].
2. Transient myopic shift after phakic intraocular lens implantation [79]: a potential complication of iris-claw pIntraOcularLens implantation.
3. Transient myopic shift following inflammation. Myopic changes induced by inflammatory diseases can occur in uveitis. Uveitic conditions that can induce a myopic shift include sclero-choroidal inflammation, lens induced myopia due to steroid cataracts, juvenile idiopathic arthritis (JIA) induced myopia; Uveitis can cause acute, transient or constitutive myopization in different contexts. These include acute inflammation such as in choroidal or scleral inflammation, chronic uveitis as in juvenile idiopathic arthritis (JIA) related uveitis, as a consequence of therapy such as lens related myopization following long-term corticosteroid therapy [80].
4. Transient myopia following (blunt) trauma [81-85]: Transient myopia after blunt trauma is caused by anatomic changes in the ciliary body and crystalline lens. It is noted an anterior lens displacement, increased lens thickness probably due to lens edema, choroidal detachment, and ciliary body edema. Ultrasound imaging shows an iridocorneal angle closure that could have led to angle-closure glaucoma. UBM shows also an annular ciliochoroidal effusion with ciliary body edema, anterior rotation of the ciliary processes, and disappearance of the ciliary sulcus. Transient myopia following blunt trauma is a rare transient situation which may be seen in the injured eye or both eyes after blunt ocular trauma. Myopia may have been due to ciliary spasm arising from stimulation of the efferent autonomic system and ciliary body edema.
5. Transient myopic shifting in systemic lupus erythematosus [86-88]: The ocular complications could be related to antiphospholipid syndrome.
6. Transient myopia in systemic tuberculosis [89]: a rare presenting feature of systemic tuberculosis; sudden onset blurred distance vision and fever are observed; anterior segment examination reveals narrow angles on gonioscopy.
7. Transient myopic shift after pars plana vitrectomy [90,91] and after panretinal photocoagulation [92]. Choroidal effusion is noted.
8. Other considerations in a patient with narrow angles similarly caused by a ciliochoroidal effusion include scleritis, uveitis, juvenile idiopathic arthritis, tumors such as retinoblastoma and medulloepithelioma (in the child), and exudative retinal detachments.
Discontinuation of these medications leads to complete resolution of the anatomic shift. The ocular and myopic changes clear up completely. Ciliochoroidal effusion, transient myopia resolve and rapid resolution of angle closure occurs after discontinuation of the drug. If intraocular pressure remains uncontrolled, additional therapies such as topical intraocular pressure-lowering medications may need to be considered. Active measures like cycloplegic may play a role, too short.