Tubular Apocrine Adenoma – Case Report and Systematic Review
Tubular apocrine adenomas are relatively rare, benign, skin adnexal tumors with a limited number of cases reported in the literature. Herein is offered an additional case, as well as a thorough review and analysis of all previously reported cases.
Keywords: Tubular apocrine adenoma; Nevus sebaceous; Syringocystadenoma papilliferum
There are many benign skin adnexal tumors with four main types of differentiation—apocrine, eccrine, follicular, and sebaceous [1]. A number of these tumors are very rare; amongst them is tubular apocrine adenoma (TAA), first described by Landry and Winkelmann in 1972 [2].
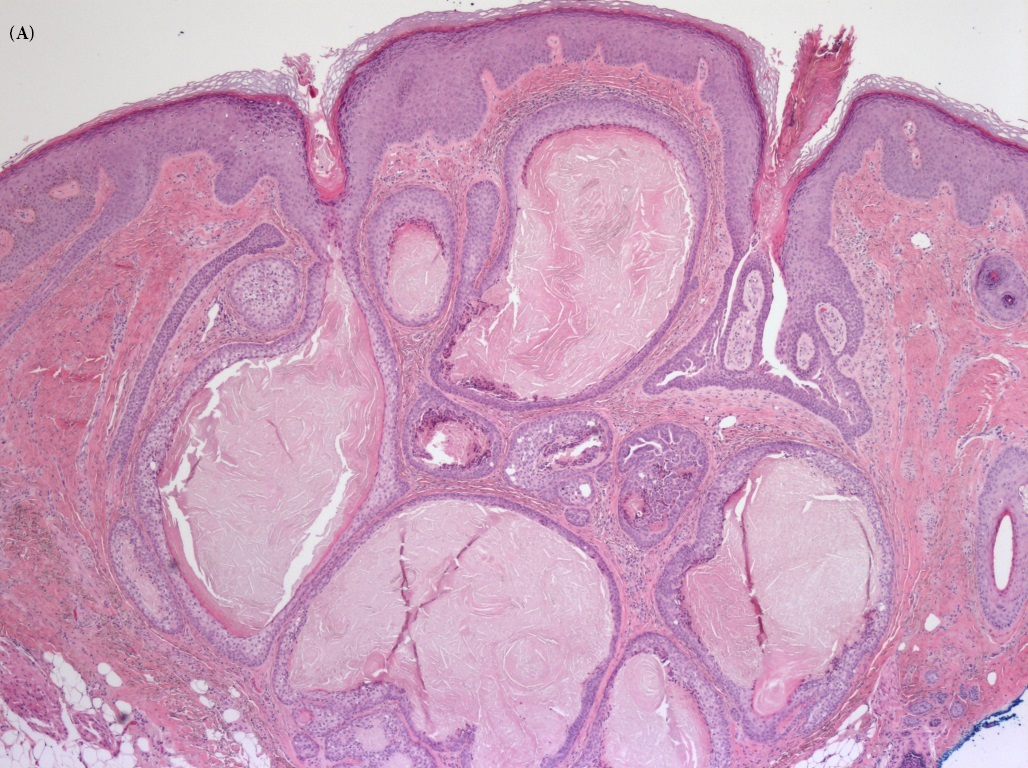
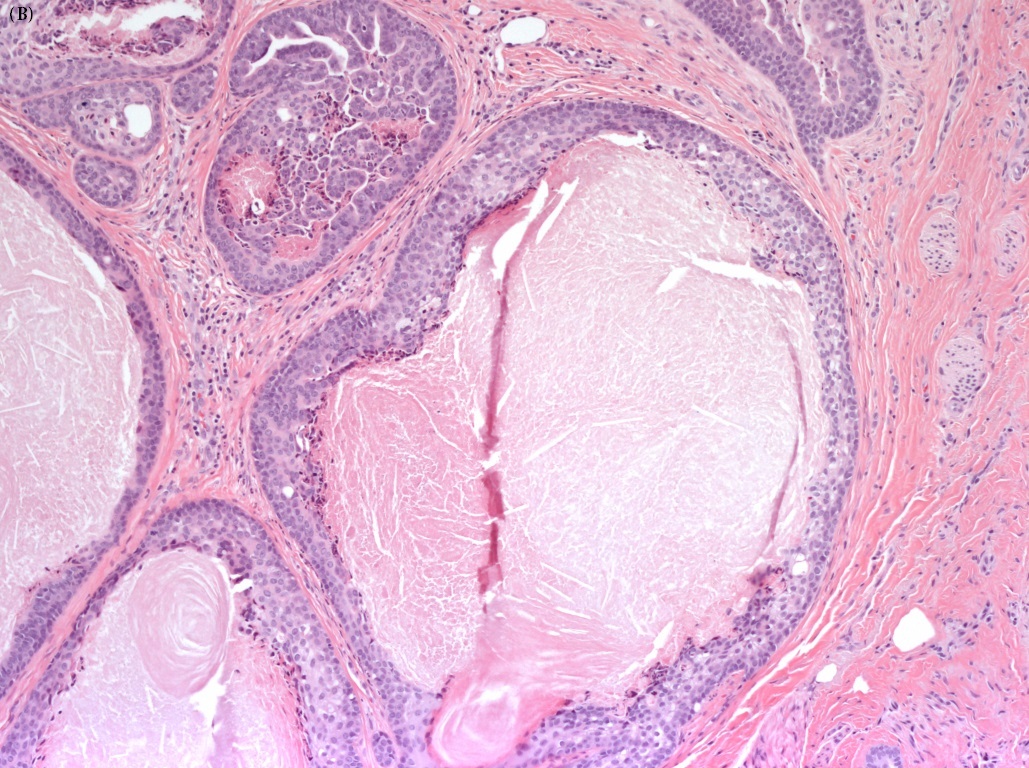
In their original description, Landry and Winkelmann used light microscopy, electron microscopy, and histochemistry to classify TAA. Some of the histologic findings that they described included numerous, well-defined lobules in the dermis, which were composed of variably sized tubules lined by two cell layers. The outer layer was cuboidal or flattend cells; the inner layer was columnar and exhibited decapitation secretion, as seen with apocrine sweat glands. The surrounding stroma was fibrous connective tissue with few plasma cells [2].
In addition to structure, Landry and Winkelmann used histochemistry to classify their patient’s tumor. At that time, certain enzymes indicated eccrine or apocrine differentiation. Eccrine glandular tissues were positive for phosphorylase, whereas apocrine tissues were positive for acid phosphatase [2]. Later, investigators developed immunohistochemical methods to differentiated the two tissue types. In 1989, Ansai et al contributed to this diagnostic approach by identifying anti-CEA antigen and anti-S 100 protein as indicative of a TAA [10].
Since Landry and Winkelmann’s initial description, greater than forty cases have been reported in the literature. We report another case of TAA appearing on the scalp of an elderly female. In addition to this case report, we completed a comprehensive review of other reported cases in an effort to summarize the characteristics of the tumor and help with future diagnoses.
A 73 year-old African American woman presented with 2 non-painful, freely moveable lumps on her scalp. The lesions were circular in shape with regular boarders and measured 3 mm and 2 mm in size. The larger of the two masses was located near the apex of the scalp and had been slowly growing in size for the past year. The smaller mass was located near the occiput and had been present for only a couple of months. Even though they were not painful, she noticed them while combing her hair and requested their excision.
Both lesions were excised with a wide local excision. An oblong incision was made with 2 mm of clinically normal boarders along the narrowest portion. The incision was carried down to the hypodermis. Histologic analysis of the superior, larger lesion demonstrated a 6 mm papule with irregular tubular epithelial cells and stromal fibrosis (Figure 1). This was consistent with a tubular apocrine adenoma and the margins were involved with the tumor. The smaller lesion was found to be a 4 mm verruca vulgaris. No immunohistochemistry was performed on either lesion.
The patient was seen in follow up and doing well. She was recommended to undergo repeat excision to obtain negative margins, but she has declined repeat excision and also elected to forgo clinical follow up.
A search of PubMed was performed on December 26, 2014 using the keywords “tubular apocrine adenoma” to identify reported cases of TAAs. The resultant manuscripts were reviewed by two authors (SM & TPP) to assure appropriateness, and the references were reviewed to screen for additional case reports not previously identified. Demographics, accompanying pathology, and outcomes measures were abstracted from the manuscripts. Empty data sets were excluded from the analysis.
Summative data analysis was performed with the inclusion of the aforementioned case report included in the data set. Data are presented as mean ± standard deviation. Categorical data are compared using a chi-square analysis and continuous outcomes are compared with a Student’s t-test. A p-value of < 0.05 was considered significant. All statistical analyses were performed using IBM SPSS Statistics, Version 22.
Review of the literature identified 37 manuscripts describing 44 individual cases of TAAs, with the present case now accounting for a 45th patient (Table 1). All of the data points were not able to be abstracted from every case.
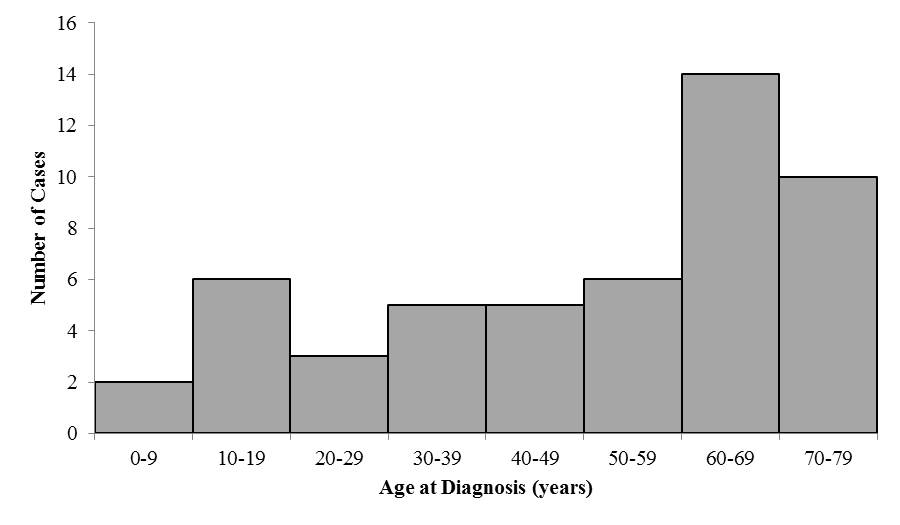
The mean patient age at diagnosis was 48.9 ± 22.1 years with a trend toward increased incidence in the latter decades of life (Figure 2). However, it should be noted that several patients had a history of waiting multiple years to have the mass excised, and therefore the onset may be younger than the current data suggests. In fact, nine patients (20%) the lesions excised were reported to have been present since birth. The majority of patients (64%) were females. These findings of a predominance of tubular apocrine adenomas occurring in middle-aged females is in keeping with what other have reported [28,29,33].
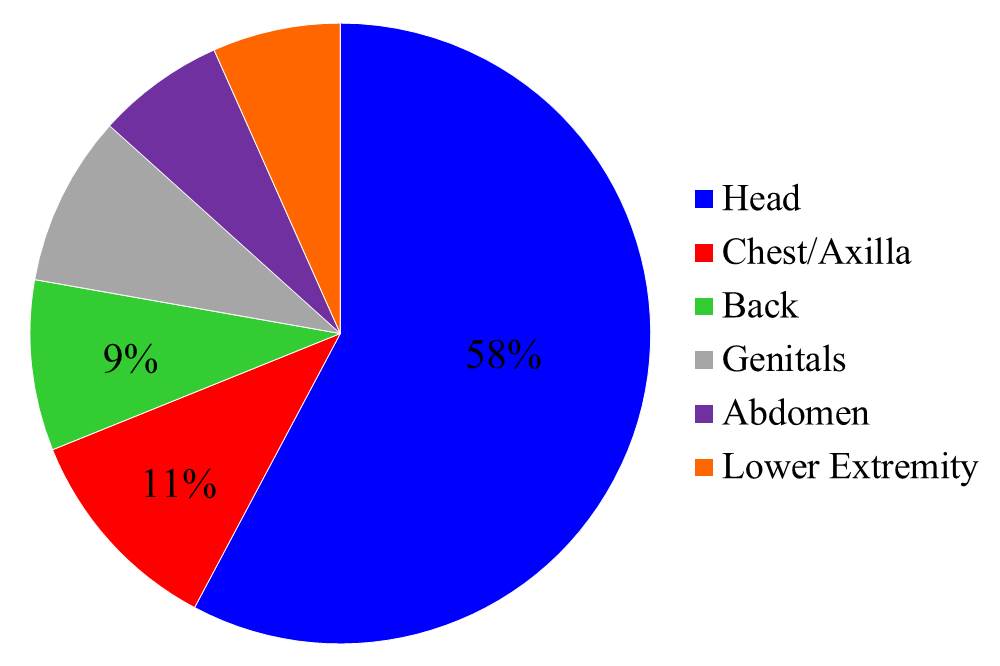
Tubular apocrine adenomas have been described as occurring on a variety of areas across the body (Figure 3), however the majority of cases occur on the scalp and over half of them occur above the level of the shoulders. Other less commonly reported body areas include the chest (including axilla and breast), back, lower extremity, genitals, and abdomen. As tubular apocrine adenomas are a benign skin adnexal tumor with apocrine gland differentiation, this body distribution is surprising since apocrine skin glands typically have a very limited distribution in the body, being found usually in the axilla and anogenital regions [39].
Theories regarding the origin of the tumor have been developed [11]. These types of tumors may develop from primary epithelial germ cells, pluripotent cells, or cells of pre-existing structures. Based on the distribution seen in Figure 3, it seems unlikely that these TAAs could be derived from cells of pre-existing structures, because, as mentioned, apocrine glands are considered normal adnexa of the axilla and anogenital regions, not the head. Therefore, these benign skin tumors are likely derived from primary epithelial germ cells or pluripotent cells.
Tubular apocrine adeonomas are commonly found with other dermatologic neoplasms. In 40% of cases, the patient also had a nevus sebaceous/organoid Nevus of Jahassohn (NS) and/or syringocystadenoma papilliferum (SCAP). The presence of multiple benign adnexal tumors in the same specimen has led to some controversy regarding the classification and relationship of these tumors to each other. This controversy emerged shortly after Landry and Winkelmann’s first description of tubular apocrine adenomas [2] when Fisher argued that TAAs were merely a variant of SCAP [40]. However, subsequent studies using light microscopy, electron microscopy, and immunohistochemical analysis have shown that these are related, but distinctly separate tumors [17]. Findings that are more suggestive of a TAA include a predominantly tubular pattern to the epithelial layer, stromal fibrosis, and the presence of comedo-like structures, whereas findings more suggestive of SCAP include cystic dilation of the epithelial tubules, plasma cells in the stroma, papillomatosis, and cystic invagination of the surface of the skin [14].
It has been proposed that much of the difficulty in differentiating between these tumors may be due to the potential for TAAs to develop from SCAP and/or NS [31]. Apocrine glands have been noted to be present deep within NS, and these glands may be the origin of TAAs that develop later in life [21]. Further supporting this assertion are the observations that all cases of TAAs occurring with NS and/or SCAP occur in lesions present for over 5 years prior to excision, and that the majority of lesions had been present since birth or childhood. These findings suggest that these tumors arise from either pluripotent or primary epithelial germ cells.
Despite the similarities between these tumors, minor differences exist in the epidemiology of these conditions as summarized in Table 2. Patients with concomitant TAAs and SCAP are diagnosed at a similar age, but are more likely to have been reported to occur in a lesion present since birth or childhood than patients with isolated TAAs. Also, the female predominance is lost in the setting of concomitant disease. The distribution of involved body parts is essentially unchanged between the two groups. While none of these differences reach statistical significance, the limited number of reported cases does allow for a potential type II error.
Since Landry and Winkelmann’s original case, the treatment of tubular apocrine adenoma has consistently been excision of the lesion to negative margins. This recommendation has been reinforced by Burkett & Zelickson, who presented a case of tubular apocrine adenoma that showed perineural invasion [8]. In light of this case, many authors have recommended excision of the lesion with wide margins. Excision or re-excision (if necessary) has been curative according to all case reports, although long term follow up is limited.
Tubular apocrine adenomas are an infrequently reported skin adnexal tumors with less than 50 reported cases in the literature. It typically forms on the head, specifically the scalp, but has been reported in multiple areas throughout the body. The tumor is more common in males and is generally diagnosed during adulthood. However, the age of onset of the lesion is more difficult to ascertain as there are numerous reports of these lesions having been present since childhood. While this tumor has been associated with other benign skin adnexal tumors, making diagnosis difficult, it remains a distinct entity. The management of this tumor has not changed since its first description in 1972 [2]; the curative treatment remains excision. The relatively limited number of reported cases has hindered a thorough understanding of this tumor and its natural history. However, this remains a clinical entity that the practitioner should be aware of and consider within their differential diagnosis as there is some concern for malignant degeneration and/or perineural invasion.
The views expressed herein are those of the authors and do not reflect the official policy of the Department of the Army, Department of Defense, or the U.S. Government