Uterine Didelphys, Blind Hemivagina and Homolateral Renal Agenesis about a Case
We here report a teenage girl with the uterus with blind hemi-vagina associated with renal agenesis. She was treated surgically with good outcome. Some different modalities of management protocols/strategies were retrieved with the literature review, which may be of use for physicians who may have chance to treat patients with this condition.
Keywords:Teenage girl; Women; Humans; Kidney Abnormalities; Uterus abnormalities; Vagina abnormalities
In the 20th century, the embryology of the female urogenital system was more studied, observed and discussed in view of the emergence of anomalies of the female genital tract, which affects both the lower and upper genital tracts.
A 15-year-old girl presented with continuous lower abdominal pain for the past 6 months. (With menstruation: 6 menstruations). She had her first menstrual period at age 15 and a normal menstrual cycle of 4/28 days. The physical examination revealed normal external genitalia: vulva and perineum, speculum examination and vaginal touch not done (patient said she was a virgin). Rectal examination demonstrated a painless left uterine mass that is mobile on palpation. The abdominal clinical examination was unremarkable. The blood count and other biochemical parameters were within the normal range.
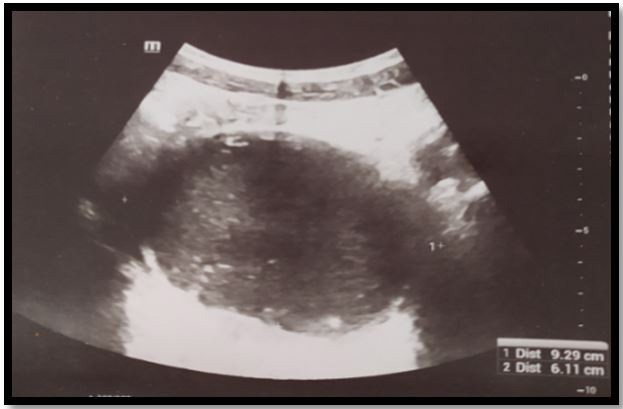
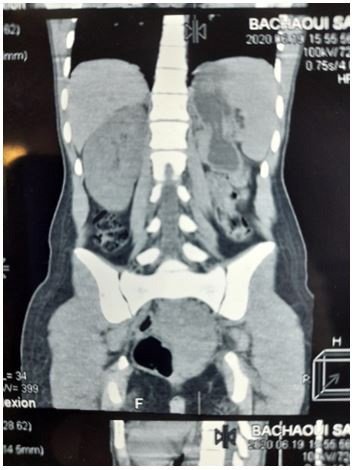
The ultrasound examination performed elsewhere was reported as intrauterine effusion: and the patient also benefited from an abdomino-pelvic CT scan + ultrasound complement with axial sections carried out in spiral acquisition with frontal and sagittal reconstructions in 3D having as results: presence of a collection with thick contents of 12 cm long x 7cm wide retro vesical taking the shape of the uterus in favour of a retention of the periods: hemato-utero colpos most probably with right kidney hypertrophy normal compensatory small kidney left pelvic atrophy normal bladder liver spleen with no anomalies. Then the patient was sent to us for confirmation of the ultrasound findings and evaluation.
Further evaluation was performed by MRI: with an appearance in favor of a bicornuate
Uterus with hematocolpos on the left associated with agenesis of the left kidney:
Presence of a left latero uterine formation with a long uterine parenchyma on the upper pole in quantity with the contralateral uterine horn, thus evoking a bicornuate uterus
This tubular formation whose inferior pole projects below the pubic symphysis, showing a T1,T2 hypersignal, persisting in T1 hypersignal after fat erasure, thus corresponding to hemorrhagic content
This formation is extended over a height of 150 mm by 61 mm of anteroposterior diameter
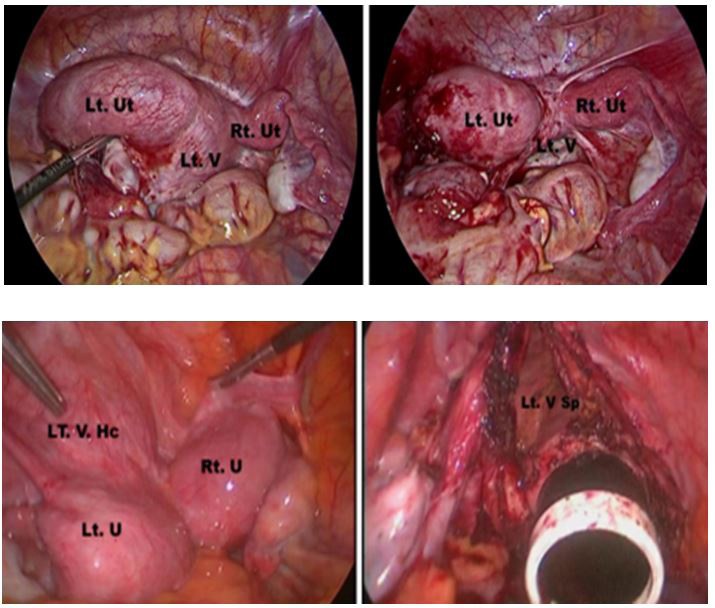
The patient was treated surgically by celescopy which confirmed the malformation by opening an opening in the septum between 2 hemivaginas and incising the collection of the obstructed right hemivagina flowing into the patent left hemivagina. The patient was relieved of her symptoms. Postoperative ultrasound follow-up 1 month later revealed complete disappearance of the hematocolpos and collapse of the right hemivagina. The cyclic dysmenorrhea disappeared. The surgical result was satisfactory with an expectation of almost normal fertility and normal sexual abilities.
Müllerian duct abnormalities are a rare and underdiagnosed group of entities that cause specific symptoms in adolescent girls and may be associated with infertility as well as adverse pregnancy outcomes. These malformations occur as a result of arrest or abnormal development of the Müllerian ducts at various stages of the female reproductive system during gestation. Obstructed hemivagine and ipsilateral renal abnormality syndrome (OHVIRA), formerly known as Herlyn-Werner-Wunderlich syndrome, is a rare entity characterized by the presence of a didelphys uterus with an obstructed hemivagin caused by a vaginal septum and the association ofThis syndrome can go undiagnosed during childhood and usually becomes symptomatic after menarche, causing obstructive symptoms. Sometimes it can be identified after evaluating a patient with infertility or recurrent pregnancy loss. Clinical diagnosis is very difficult and requires imaging studies in which ultrasound and MRI play an essential role in diagnosis, classification and treatment plan. Proper diagnosis and treatment results in complete improvement of symptoms, an adequate reproductive prognosis and avoids major complications such as endometriosis, pelvic adhesions and infertility.The aim of this review is to demonstrate the pathophysiology, clinical manifestations, diagnostic methods and treatment of obstructed hemivagine and ipsilateral renal anomaly syndrome. Clinical diagnosis is very difficult and requires imaging studies in which ultrasound and MRI play an essential role in diagnosis, classification and treatment plan. Proper diagnosis and treatment results in complete improvement of symptoms, an adequate reproductive prognosis and avoids major complications such as endometriosis, pelvic adhesions and infertility.The aim of this review is to demonstrate the pathophysiology, clinical manifestations, diagnostic methods and treatment of obstructed hemivagine and ipsilateral renal anomaly syndrome. Clinical diagnosis is very difficult and requires imaging studies in which ultrasound and MRI play an essential role in diagnosis, classification and treatment plan. Proper diagnosis and treatment results in complete improvement of symptoms, an adequate reproductive prognosis and avoids major complications such as endometriosis, pelvic adhesions and infertility.The aim of this review is to demonstrate the pathophysiology, clinical manifestations, diagnostic methods and treatment of obstructed hemivagine and ipsilateral renal anomaly syndrome. adequate reproductive prognosis and avoid major complications such as endometriosis, pelvic adhesions and infertility. The aim of this review is to demonstrate the pathophysiology, clinical manifestations, diagnostic methods and treatment of obstructed hemivagine and ipsilateral renal anomaly syndrome. adequate reproductive prognosis and avoid major complications such as endometriosis, pelvic adhesions and infertility. The aim of this review is to demonstrate the pathophysiology, clinical manifestations, diagnostic methods and treatment of obstructed hemivagine and ipsilateral renal anomaly syndrome.
The utero-cervical development was supposed to come from paired paramesonephric ducts; the sinovaginal bulb of the urogenital sinus was thought to develop into the lower vagina; the kidneys and ureters were thought to come from pro / meso / metanephros of wolf. Vertical or horizontal fusion or arrest of the paramesonephric ducts during development has been understood to successfully explain various uterine anomalies. Some complex uterine anomalies such as Obstructed Hemi Vagina Syndrome with Ipsilateral Renal Agenesis still defied conventional theory of urogenital development until recently, when the theory of development of the entire vagina from the mesonephric ducts was postulated [1].
The efficacy and safety of the vaginoscopic incision of the oblique vaginal septum in adolescents with obstructed hemivagina syndrome and ipsilateral renal agenesis (hese are approximately fourteen adolescents with this syndrome managed by vaginoscopic incision of the oblique vaginal septum using a “No-touch” technique over a period of 8 years.
In the fourteen adolescents with OHVIRA, the oblique vaginal septum was successfully incised without any intraoperative complications. Postoperative pain was unremarkable, and each patient’s symptoms resolved after the operation [2].
Although the actual incidence of Mullerian anomalies is approximately 1.1 to 3.5% , it is thought to be much higher (approximately 25%) in women with recurrent miscarriages and subfertility. Review of the literature in 15 reported studies comprising 1771 patients during the period 1965 - 1996 revealed a mean incidence of uterus didelphys at 11.1% [3].
A strong association of renal agenesis with uterine didelphys (81%) [3] has also been suggested.
The incidence of OHVIRA syndrome is very low and only isolated case reports have been published. Many of these are present in early childhood due to the collection of secretions in the obstructed vagina under the influence of maternal hormones; others are collected within 1 to 2 years of the onset of menarche due to the development of hematocolpos, hematometrium or even hematosalpinx. These patients present with cyclic dysmenorrhea, which later progresses to persistent pelvic pain. Almost all of them are initially misdiagnosed clinically, as in our case, which was thought to be endometriosis / tuberculous collection for clinical reasons.
To understand the pathogenesis of Mullerian abnormalities and their association with renal abnormalities, the embryology of utero-vaginal development must be reviewed. Vaginal embryonic development has become a hot topic of debate following Acien’s proposal for a new theory of vaginal origin [4].
The classical theory of vaginal development says that the upper part of the vagina develops from the mullein duct (paramesonephric) and the lower part from the sinovaginal bulbs derived from the urogenital sinus. The fusion of 2 sinovaginal bulbs forms a vaginal plaque, which later channels to form a vaginal lumen [5].
Classical theory has proved insufficient to explain complex Mullerian malformations such as OHVIRA and their coexistence with renal abnormalities. Acien suggested that, although the uterus and cervix are derived from paired channels paramesonephricfused (2 nd part) and diverging distal paramesonephric channels (3 rd party), the vagina was completely mesonephric origin ( wolffian) although its lining revealed Mullerian cells derived from the Mullerian tuber. Therefore, the paramesonephric ducts do not contribute to the formation of the vagina, unlike the Mullerian tubercle, so the vagina is lined with cells of the Mullerian tubercle. This theory was further reinforced by data published by Sánchez [6] in his experiments with female rats using histoimmunochemical techniques.
Early failure of the metanephric diverticulum to develop (approximately 5 weeks) from the mesonephric duct results in agenesis of the ureteral bud, which leads to agenesis of the ipsilateral ureter and kidney.
The mesonephros is responsible for the development and positioning of nearby paired paramesonephric conduits. Around 9 weeks of gestation, the paramesonephric duct is positioned in such a way that it is lateral to the mesonephric duct in the first part, crosses it anteriorly and is located medial in relation to the latter in part converging. Due to improper positioning of the paired paramesonephric duct, both hemi-uteri and hemicervices fail to unite, resulting in uterus didelphys. In OHVIRA syndrome, stopping the development of the ipsilateral mesonephric duct results in failure of development of the distal hemivagina, resulting in obstructed hemivagin.OHVIRA syndrome consists of uterine didelphys, unilateral lower vaginal obstruction, and ipsilateral renal agenesis, all 3 components being secondary to müllerian abnormalities induced by the mesonephric duct.
Treatment invariably requires surgery in the form of excision of the vaginal septum to relieve the obstruction. In addition to relieving pain due to obstruction, surgery also reduces the risk of pelvic endometriosis due to retrograde menstrual seeding. Patients can have a normal sex life. Some are even able to conceive and carry a pregnancy to term. In fact, hemihystrectomy, performed in the past, is no longer preferred now, as the reported incidence of pregnancy in both horns is almost equal. Altchek and Paciuc reported a pregnancy that occurred twice in a didelphys uterus previously obstructed after surgical correction. The surgeon must therefore do everything possible to preserve the blocked uterus.
OHVIRA syndrome is a rare congenital anomaly with clinical significance and simple surgical management. Imaging, especially MRI, plays a major role in diagnosis, which is often clinically missed. Proper surgery is a one-step procedure to completely excise or divide the obstructing septum. Complex Mullerian abnormalities have been difficult to diagnose correctly without the help of imaging. An MRI was particularly helpful. Correct early diagnosis is the goal of relieving symptoms and preventing complications, caused by retrograde menstruation which can lead to endometriosis and, also, to preserve sexual and conception capacities.
This condition sometimes causes abdominal mass and the symptoms are sometimes non-specific. Kidney anomalies are frequently associated. This condition should be born in mind in the examination of adolescent girls.