Vascularized Bone Graft of Zaidemberg in the Upper Pseudarthrosis of the Scaphoid
The authors studied the results of a series of 11 cases concerning the vascularized bone graft of Zaidemberg in scaphoid pseudoarthrosis. This graft is indicated in case of proximal or old nonunion, or in the presence of proximal polar necrosis. This graft gives a better rate of consolidation of pseudoarthrosis compared to conventional grafts and also remains a suitable solution and rescue during a surgical recovery.
Keywords:Pseudoarthrosis of the Scaphoid; Vascularized Bone Graft; Superior Pole; Poor Vascularization
Carpal scaphoid fractures evolve in 10% of cases towards pseudarthrosis [1-3]. When the pseudoarthrosis is located at the proximal pole, given the precarious vascularization at this level, it may be associated with superior polar devascularization or even necrosis. If left untreated, it may progress to degenerative osteoarthritis of the wrist [4-8].
The appearance of vascularized bone grafts has led to a rethinking of the management of pseudarthrosis. The literature has demonstrated a significantly higher rate of consolidation in patients with necrosis of the proximal pole of the scaphoid with these vascularized grafts [9-10]. In this indication, they are generally recommended. Indeed, they would facilitate consolidation and bone revascularization. They would have a biological and mechanical superiority over conventional grafts. Thus, when there is necrosis of the proximal pole, the consolidation rates seem to be higher than with conventional grafts [11].
In 1991, Carlos Zaidemberg of Argentina [12] described a new technique for scaphoid repair using vascularized graft taken from the radial styloid. We wanted to verify these data by studying the results of this type of graft performed in our department.
11 scaphoid pseudarthroses treated with Zaidemberg graft [12] between 2007 and 2014 were studied retrospectively with a mean follow-up of 3.5 years (9 months - 6.5 years).
Among them ,2 patients benefited from palliative surgery after failed consolidation.
We operated on 7 scaphoids on the right side and 5 scaphoids on the left side.
In 8 cases it was the dominant hand
There was a clear male predominance (10 men and 01 woman).
No patient had any comorbidities.
07 patients (men) used tobacco.
The average age of the patients at the time of the accident was 26 years (18-45 years)
The average age of the patients at the time of the intervention was 29 years (19-48 years)
The average time from injury to management was 3 years (6 months-6 years)
The main cause of the fracture at the time of the initial accident was:
A work accident (08cas)
Sports accident (03 cases)
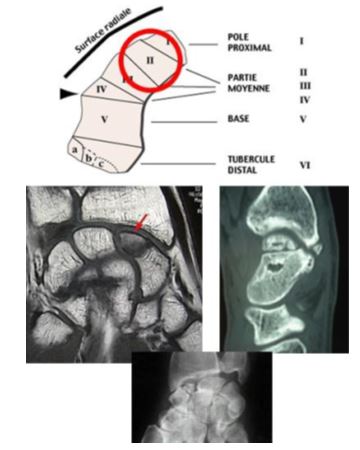
According to Schernberg’s classification (8), the pseudoarthrosis was located in zone 3 in 8 cases and in zone 2 in 3 cases.
We had 8 cases of stage 2a and 3 cases of stage 2b according to the Alnot classification [1,2].
The diagnosis of necrosis was retained 7 times (Figure 1), in case of fragmentation of the proximal pole, absence of enhancement of the latter after injection of gadolinium on MRI, or by the absence of bleeding, or by a white and chalky aspect, the consistency of the bone according to Green’s intraoperative criteria [6].
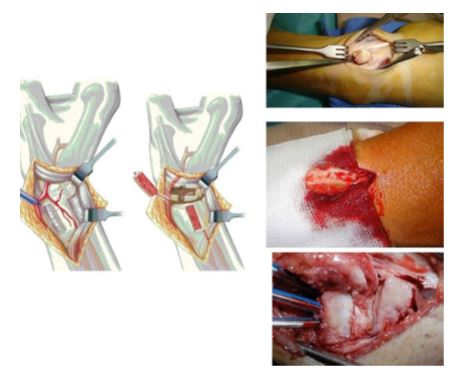
The principle of the operation was to incarcerate a dorso-radial bone graft in the previously cured pseudarthrosis site, pedicled on the supra-retinacular artery of the radius. Osteosynthesis was performed with pins followed by immobilization until radiological consolidation of the pseudarthrosis site.
After a dorso-radial, longitudinal, straight approach, centered on the radiocarpal space and careful control of the radial nerve branches, the supraretinacular artery (SRA) is exposed. Opening of the first two extensor compartments on either side of the path of the artery always. A longitudinal arthrotomy in the axis of the second compartment is performed and then the capsuloperiosteal flap is removed. De-periostealization and styloidectomy are performed while protecting the graft pedicle. Elevation of the pseudarthrosis site, harvesting of the cortico-cancellous graft, which must be cut to the right dimensions by an osteotomy centered on the ASR, which will be incorporated into the scaphoid by spreading its 2 fragments with a foam spatula. Osteosynthesis by 2 wires inserted from the isthmus of the scaphoid. Their orientation through the graft to the proximal pole is done under permanent visual control. Closure without drainage after hemostasis and removal of the tourniquet. Segmental splinting to immobilize the wrist for 3 weeks, followed by a resin glove for 8 to 10 weeks, depending on the radiological evolution.
On average, 9 out of 11 patients consolidated in 8.5 weeks.
The average duration of immobilization was 8 weeks with a resin BAP.
Postoperative rehabilitation also lasted 12 weeks.
No patient required vocational retraining
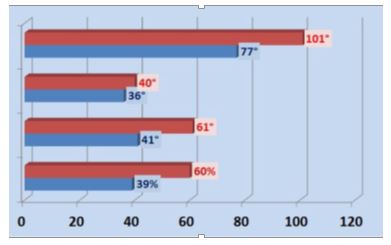
The clinical criteria studied were: joint amplitudes, wrist strength, the Quick Dash which was 12%, the PRWE questionnaire which includes 15 questions with a total score reported at 100, it reflects the inability of the patient to use his operated wrist in comparison with the healthy side. and the Mayo Wrist Score combining a subjective and objective functional evaluation by studying the intensity of the pain, the ability to return to work, mobility and strength. (Figure 3).
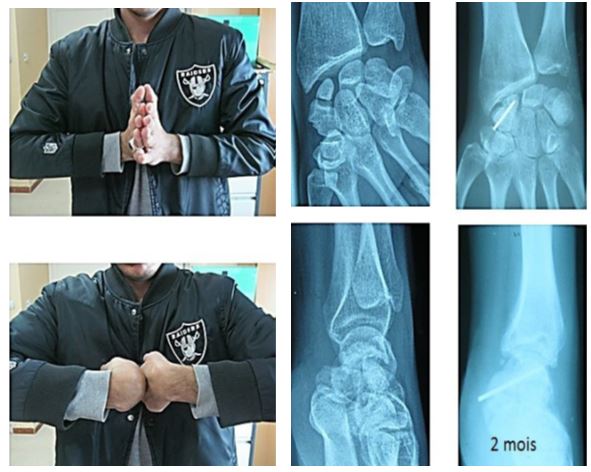
Overall, the clinical results are comforting in more than one way, since there was a clear improvement in all the clinical evaluation parameters, the arc of mobility in flexion-extension went from 77° preoperatively to 101° postoperatively, as well as the strength of the hand, which improved from 39% to 60%, explained by the reduction in pain (Figure 4).
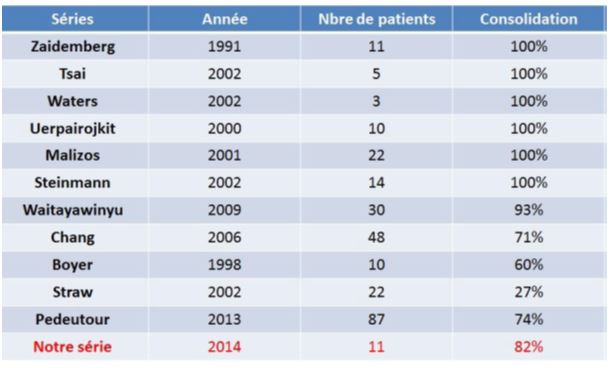
The radiographic workup allowed us to monitor the consolidation. On review of the literature, our results on consolidation are close to the worldwide data, as summarized in the table comparing the results of the various authors (Figure 5). We observed 9 consolidations out of 11 in 8.5 weeks on average.
The criterion for analysis of bone consolidation was strict: consolidation was considered effective in the absence of interfragmentary deviation at the pseudarthrosis site, in the absence of movement of the material or a lysis chamber around it, and in the absence of progressive displacement of the graft. The two failures in consolidation were explained by malposition of the graft. From the global result point of view, our patients had an average Mayo Wrist Score of 78%. The three poor results were explained by the unfavorable evolution of the two pseudarthroses that did not consolidate and by one pseudarthrosis that finally consolidated but retained poor wrist mobility and persistent pain.
In cases of prolonged pseudarthrosis or necrosis of the proximal pole, the results with vascularized grafts are better compared with conventional bone grafts especially the Matti-Russe technique.
Recently, experimental studies have shown that in a poor quality recipient site, incorporation of a vascularized graft was better than that of a non-vascularized graft. These well-known studies have also shown that revascularization of a bone was facilitated by a vascularized graft and that consolidation was faster [3,4].
Since Zaidemberg’s description [12], the supraretinacular artery-based graft has been increasingly used in scaphoid pseudarthrosis, with variable consolidation rates depending on the series, generally exceeding 90% consolidation. Zaidemberg’s series [12], consisting of 11 patients, shows a 100% consolidation rate in 6.2 weeks.
The meta-analysis by Merrell [11] found a consolidation rate of 47% with conventional grafts in 64 patients with vascular necrosis of the proximal pole, rising to 88% with a vascularized graft. Our results appear to be consistent with those reported in the literature, which are summarized in Table 1.
The dorso-radial approach used in the Zaidemberg technique [12] is untouched by any intervention, and is a valuable advantage. This approach gives access to the graft harvesting site in the immediate vicinity of the reconstruction site. It allows for graft harvesting and treatment of the pseudarthrosis in the same operating time (minor morbidity, aesthetic advantage). The anatomy of the supraretinacular artery is constant, which allows for a reliable and reproducible technique. Morbidity at the donor site using a minor vascular axis is therefore minimal and the pedicle is long enough to reach the pseudarthrosis without the slightest tension. This harvesting procedure allows us to dispense with general anesthesia, with the possibility of outpatient treatment under locoregional anesthesia [13].
Graft harvesting thus allows a shorter operating time, but for iliac harvesting, there are risks of haematoma, which may become infected, and of fracture of the iliac wing, which may cause pain and injury to the femoral-cutaneous nerve [14-16].
The major concern is in the manipulation to adapt it to the bone loss because of the risk of injury to the pedicle. Indeed, a free graft is easier to cut to the desired shape than a pedicled graft [16]. Its embedding in the scaphoid also remains a difficulty. The graft cannot be impacted at the recipient site, as one would impact a non-vascularized graft, an impaction could damage the pedicle and consequently compromise the vitality of the graft in addition a graft of radial origin is more friable and less consistent than an iliac graft [14,15].
Our results on a series of 11 cases concerning the vascularized Zaidemberg bone graft in scaphoid pseudarthrosis are consistent with those in the literature. This graft is indicated in cases of proximal or old pseudarthrosis, or in the presence of proximal polar necrosis. It allows for better consolidation of pseudarthrosis than conventional grafts. It is thus a suitable solution for revision surgery.
The Zaidemberg graft [12] improves the radiometry of the carpus and seems to prevent arthrosis. (Figure 6).
This procedure remains difficult and therefore requires a learning curve. Given the difficulties in harvesting the graft, the persistence of its vascularization after osteosynthesis remains an uncertainty. The series concerning vascularized grafts do not allow us to affirm the persistence of vascularization during the bone consolidation process [23].