Young Women With Relapse Of Acute Lymphoblastic Leukemia Mimicking The Myomatous Uterus
Precise
Case presenation of a rare clinical manifestation of a relapse of acute lymphoblastic leukemia in a young woman manifested by growing uterus mimicking a myomatous uterus.
We present a case of a rare clinical manifestation of a relapse of acute lymphoblastic leukemia ( ALL) in a young woman who desired for pregnancy. ALL relapse manifested by growing uterus mimicking a myomatous uterus.
Keywords: Acute Lymfoblastic Leukemia, Myoma, Laparoscopy, Chemoterapy
Acute lymphoblastic leukemia (ALL) is the most common childhood malignancy. Its manifestation is non-specific mainly. The most usual manifestations are hepatomegaly, splenomegaly, lymphadenopathy, pallor, fever, musculoskeletal pain, or bruising. We present a rare occurrence of ALL mimicking the myomatous uterus in young women wishing conception.
25 years old, Nuligravida (0 para/ 0 gravid)
Family health history: parents and brother are healthy
Personal health history: Infectious mononucleosis in 5 years of age mild hypothyroidism. Diagnosis of euploid common B-acute lymphoblastic leukemia (cALL) was made on 16.8.2010 at the patient´s age of 15. Initially without central nervous system infiltration. Since the day of diagnosis she was treated with a pediatric protocol and based on high minimal residual disease (MRD) values at week 12, she received intensive chemotherapy, achieved MRD negativity and was indicated for allogeneic hematopoietic stem cell transplantation (HSCT), which was then performed on 23.2.2011 from unrelated mismatched male donor. Since then, she has been in remission.
operation: 0
allergies: 0
abuses: 0
Pharmacological anamnesis: Euthyrox 50 ug 1-0-0, Hormonal contraception – Ethynil estradiol 0,03 mg+ drospirenon 3 mg social history: university student
Gynecological anamnesis: She had menses since14 years with a regular cycle. Following chemotherapy, she was suspected of ovarian failure and therefore received hormonal substitution (hormonal contraception).
Surgery: none
Current disease: A gynecologist referred the patient for a growing myoma and intercourse pain. She is planning a pregnancy this year.
Examination by gynecological mirrors: A 4cm myoma was visible in the vaginal fornix right to the cervix.
Palpation: The uterus in the anteversion-flexion (AVF) was enlarged by numerous myomas; both adnexa were without any pathology.
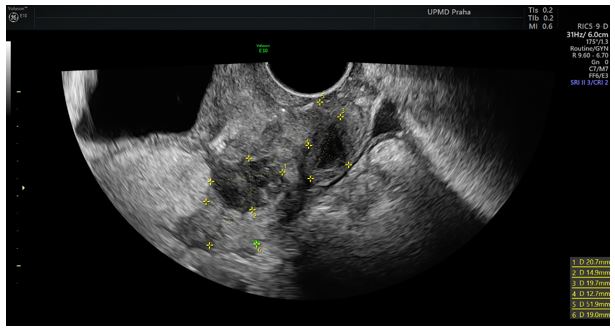
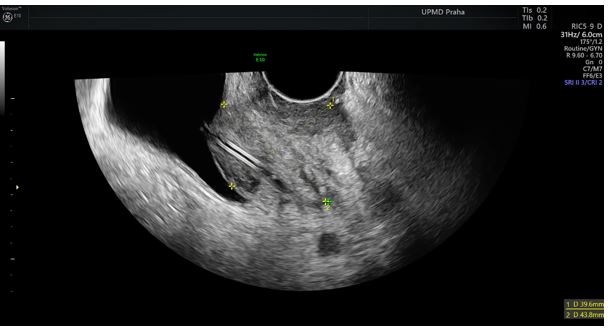
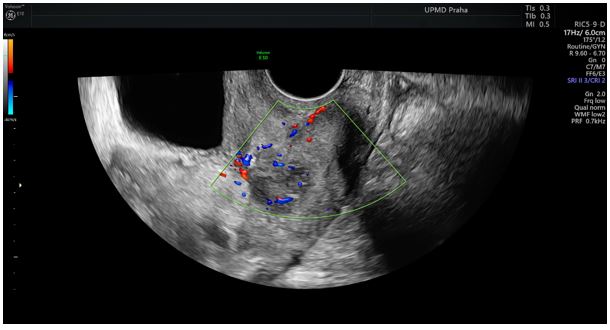
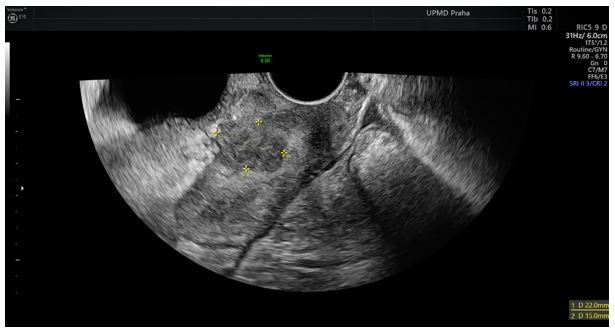
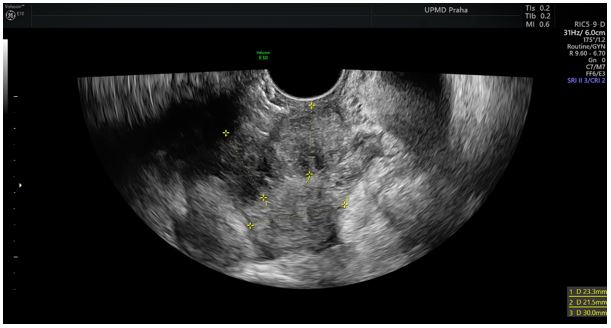
Ultrasound (figures 1, 2, 3, 4 ) : The uterus was in AVF (52x35 mm), the uterine wall was not homogeneous. There were several myomas:
1. An intraligamentous myoma (43mm) on the right side of the uterus near the internal cervical ostium
2. An intramural myoma (25mm) in the right uterine edge
3. Subserous myoma (20mm) on the anterior wall
4. Subserous myoma (20mm) in the fundus
Anti-Müllerian hormone (AMH): 0.2
We recommended surgery, including vaginal extirpation of myoma and laparoscopic enucleation of myomas, and the patient agreed.
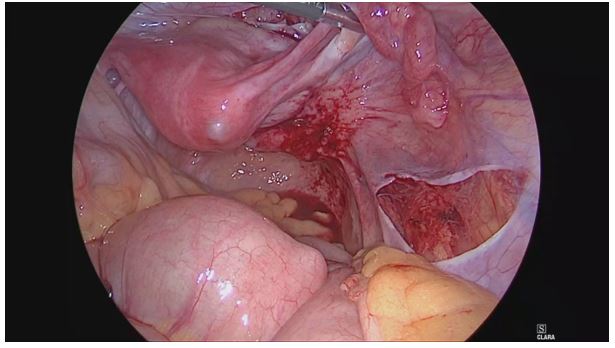
Surgery: We extirpated most of the intraligamentous myoma (1.) from the vaginal approach during the surgery. The myoma appeared soft, and we suspected it of adenomyosis. We continued laparoscopically (see the record). Only the subserous myoma (3.) on the anterior uterine wall was send for biopsy due to its atypical appearance. (see the Figures from the operation 1,2,3). The surgery was terminated. We are waiting for the result of histology.
Seven days after surgery, patient reported pain in the right abdomen. An ultrasound examination revealed compression of the right ureter with a myoma on the right uterine edge and dilatation of the right kidney excretory system. The patient received an ureteral stent (Figures 2, 3).
The tissue specimens consisted of smooth muscle, which was minor, and tumourous elements of a lymphoid character. This tumor diffusely infiltrated all specimens and had a high nucleoplasmic ratio in favor of the nucleus. The nuclei had a fine chromatin structure and pronounced nucleolus. Morphologically, they were more blasts. Blasts lined up concentrically around larger vessels. In a limited immunohistochemical examination, the proliferative activity determined by the MIB index in blasts was about 60-70%. B-ALL / LBL infiltration (positivity PAX5, CD79a, CD10, TdT, CD43, LCA; Ki67 80-90%).
The conclusion was relapse of lymphoblastic leukemia.
The PET / CT examination confirmed massive bone marrow infiltration with the extramedullary infiltrates in the uterus, vagina, the visceral and parietal peritoneum, and the skeleton (osteolytic deposits).
Therapy: 1st relaps was confirmed 6.5.2019 (after a year of observing suspected “myomatosis uteri”) by the biopsy from uterine masses described in this case report (histology: B-ALL/LBL infiltration ,positivity of PAX5, CD79a, CD10, TdT, CD43, LCA; Ki67 80-90 %, Ph+, CD20-). Massive bone marrow infiltration was subsequently confirmed on 29.5.2019. According to PET/CT extramedullary sites in uterus, visceral and parietal peritoneum and skeleton (osteolytic foci) were involved. After steroid prephase, hyperCVAD (cyclophosphamide, vincristine, anthracycline, dexamethazone) regimen, inotuzumab and lymphodepletion regimen, CAR-T cells (Kymriah) were applicated on 24.9.2020.
2nd relapse was diagnosed. 30.11.2020 both medullary and extramedullary. In 3rd complete remission after inotuzumab and three chemotherapy cycles the patient underwent 2nd allogeneic hematopoietic transplantation in reduced-intensity conditioning on 5.5.2021, complete molecular remission was achieved after allogeneic transplantation (29.6.21).
3rd molecular relapse was detected on 2.9.2021 and hematologic relapse on 6.10.2021. After bridging with hyperCVAD regimen, the patient received 25.11.2021 in-house CAR-T cells (antiCD19) in clinical trial UHKT-CAR10-01.
The patient is in complete molecular remission shortly after the last therapy.
The most common uterine tumors in reproductive women are myomas. [1,2] Usually, they are noncancerous monoclonal tumors arising from the smooth muscle cells and fibroblasts of the myometrium. The incidence cannot be precisely determined, but it is around 15-25%. [3,4,5] Clinical symptoms depend on their location and size. It mainly includes dysmenorrhea, dyspareunia, hypermenorrhea, lower abdominal pressure, and pregnancy-related complications such as miscarriages or premature births [6,7,8] Myomas are usually diagnosed by ultrasound, and they appear as hypoechoic, well-circumscribed round masses, frequently with shadowing. Palpation and health problems can help diagnose them [9,10]
The differential diagnosis includes other types of uterine tumors; adenomyosis, uterine sarcomas, which are more often in older women, endometrial carcinoma invading the myometrium, carcinosarcoma, and endometrial stromal sarcoma invading myometrium. We must also consider metastasis most often origination in the urogenital tract [11,12,13].
Acute lymphoblastic leukemia (ALL) is a rapidly proliferative malignant disease with only a very short survival if left untreated. It is the most common malignancy of childhood - it´s incidence in the age group between 1st and 5th year of life is about 7,7 per 100 000. The incidence among adults is about 1/100 000 with a second peak in elderly patients over 60. [14,15] Manifestations of the disease are usually unspecific in early phases – lost of weight, fevers and chills, bone pain and fatigue followed by the complications of cytopenias (neutropenic infections, thrombocytopenic bleeding, fatigue from anemia) and lymph node and liver and spleen enlargement including cases of mediastinal or abdominal bulky lesions. Less frequently are pronounced symptoms due to extramedullar involment of central nervous system, skin, testicles and other regions and organs. [16] The diagnosis of ALL is based on a complete blood count and differential count, review of the peripheral blood smear and bone marrow examination, sometimes an analysis of a lymph node biopsy. [17] The diagnosis of ALL is established by characteristic morphology of lymphoblasts and a diagnostic immunophenotype that confirms a lymphoid lineage and excludes a myeloid lineage. The cytogenetic and molecular features are of prognostic importance and help navigate the intensity of a treatment plan. The mainstay of ALL therapy is still combination chemotherapy (adapted according the minimal residual disease level dynamics) followed by allogeneic bone marrow transplantation for selected patients. More and more patients profit from addition of the modern therapies to the older protocols: tyrosine kinase inhibitors for Ph+ ALL, rituximab, blinatumomab, inotuzumab, nelarabine for T-cell ALL, CAR-T cell therapy. The childhood ALL has an excellent prognosis. The complex intensive protocols, novel therapies and allogeneic transplants have lead to improved long term survival of above 50 % also in adults [18,19,20,21].
In this case report, we present a rare localization of ALL relapse in young women. According to clinical behavior and the ultrasound, this disease mimicked a typical disease in women of this age - myoma. Interestingly, the rapid progression of the disease led to the right-side ureteral compression with the need for stent insertion. Now the patient is in remission after chemotherapy with remission of all foci described on PET / CT.